Abstract
Background
Individuals with single-sided deafness have difficulty understanding speech in noise and determining sound direction in their daily lives. Cochlear implantation, a globally accepted rehabilitation method, has recently become used in Turkey in patients with single-sided deafness. In this study, the effects of cochlear implants on auditory temporal processing skills, speech-in-noise perception performance, tinnitus, and subjective benefit were reported in two patients with single-sided deafness.
Case presentation
The cochlear implant was applied to two children with single-sided deafness with and without inner ear malformation. Speech in noise score, gaps in noise test, duration, and frequency pattern test were used. Also, cochlear implant benefits and the presence of tinnitus were questioned by questionnaires. Speech-in-noise perception performance and auditory temporal processing skills improved in the postoperative period compared to the preoperative period. It was also observed that although the cochlear implant improved the quality of life, motivation for device use decreased in the first 6 months of the postoperative period.
Conclusions
Cochlear implantation in individuals with single-sided deafness with and without inner ear malformation is useful in increasing auditory temporal processing skills and understanding speech in noise ability. In addition, cochlear implantation is a useful method to improve quality of life, especially regarding spatial perception, and it did not cause tinnitus in our patients. Selecting an implant model that enables data logging provides an advantage in determining the motivation to use the implants.
Similar content being viewed by others
Background
Individuals with Single-Sided Deafness (SSD) have difficulty in sound localization, particularly in understanding speech in noise, because they cannot use spatial auditory cues [1, 2]. Cochlear implantation has recently become the primary approach to treating SSD. This mainly stems from the restored binaural hearing provided by cochlear implants in SSD, which enhances the spatial localization of the sound and improves speech-in-noise perception [3,4,5]. There has yet to be a published article on this topic in Turkey. This study evaluated the effectiveness of cochlear implants in patients with unilateral hearing loss from various perspectives.
Case presentation
Case 1
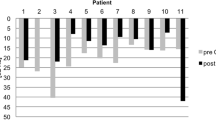
The male patient was born at full term in 2009. No risk factors have caused hearing loss in the postnatal period. Newborn hearing screening was bilaterally normal. The patient has a history of febrile convulsion at 4 years of age. In February 2018, the patient had a sudden hearing loss in his right ear. Subsequently, following therapy at another clinic, the hearing loss became permanent. The patient had normal hearing in the left ear and severe sensorineural hearing loss in the right ear. Radiology results, as per the temporal CT and MRI were bilaterally normal. The patient received a cochlear implant (CI 422 Slim Straight) in the right ear in 2020. Intra/post-operatively, all electrode impedances were normal, and electrically evoked compound action potential was obtained on 5 electrodes. According to the data logging, the duration of implant use decreased to 5.6 h/day at 3 months after implant activation. Duration of implant use increased to 11.7 h/day, 12 h/day, and 13 h/day at 6-month, 1-year, and 2-year follow-ups, respectively. The hearing thresholds with CI in the free field were evaluated by delivering constant noise at 50 dB to the healthy ear (pure-tone average (PTA):10) with headphones. The results of the masked hearing thresholds with the CI in month 6, year 1, and year 2 are demonstrated in Fig. 1.
The auditory temporal processing was evaluated with the gaps-in-noise (GIN) test, duration, and frequency pattern test. Signal intensity was determined as 55 dB SL for both tests. Speech-in-noise perception performance was assessed by determining the monosyllabic word recognition score in noise. Speech signal was kept constant at 60 dB and evaluation was made under three conditions, i.e., at signal-to-noise ratio (SNR) levels of 0, + 5, and + 10. All of the tests were evaluated in a free field (0º azimuth, 1 m distance). The Speech, Spatial, and Qualities of Hearing Scale (SSQ), The Tinnitus Handicap Inventory (THI), and Mini Tinnitus Questionnaire (TQ) were used in the subjective evaluation. All objective and subjective evaluations were carried out preoperatively and at postoperative 6 months, year 1, and year 2. All of the results for case 1 are demonstrated in Table 1.
Case 2
The female patient was born at full term in 2006. She did not undergo a newborn hearing screening. Her mother had normal hearing in the right ear and moderate sensorineural hearing loss in the left ear. She has a history of febrile convulsion at one year of age. She noticed her hearing loss in 2019 during a training course with multiple speakers. The patient had normal hearing in the left ear (PTA 10) and profound SN hearing loss in the right ear. Radiological evaluation showed Incomplete Partition Type 1 (IP-1) and Cochlear Hypoplasia Type 4 inner ear anomalies in the right and left ears, respectively. In 2021, she received a cochlear implant (Sonata Form 19) in the right ear. A C-arm was used to check the accuracy of electrode placement during surgery. Intra/post-operatively, all electrode impedances were normal whereas evoked compound action potential could not be obtained. The duration of implant use was verbally questioned since the CI brand used by the patient did not possess data logging properties. Four months after implant activation, her parent stated that she only used the implant when outside. In subsequent follow-up visits, she used her CI consistently. The hearing thresholds with the CI by masked were determined at month 6 and year, using the test procedure specified in case 1. The values obtained are shown in Fig. 2.
All mentioned tests and questionnaires were performed preoperatively and at postoperative 6 months and year 1, in the same manner as the test procedure specified in case 1. All of the results for case 2 are demonstrated in Table 2.
Discussion
The significance of auditory temporal processing in speech comprehension in quiet and noisy environments has been well-documented [6]. In case 1, continuous improvement in auditory temporal processing skills was observed. In the GIN test, the approximate threshold decreased from 6 to 4 ms, leading to improved temporal acuity. While case 1 failed to do the preoperative frequency pattern test, he could perform the test postoperatively and increase his score. Also, case 1 achieved a remarkable 92% speech comprehension in noise, specifically under the challenging SNR + 10 condition two years after cochlear implantation. Conversely, case 2 observed variable improvement in auditory temporal processing and speech-in-noise perception skills. Six months after implantation, a peak in speech comprehension in noise was observed, followed by a slight decline in scores. However, at the postoperative 1-year mark, case 2 significantly enhanced speech-in-noise perception skills compared to the preoperative period. Also, The GIN test results reflected this variability. The GIN test was increased by 8 ms at postoperative six months and reduced by 6 ms at postoperative 1 year. Despite the fluctuations observed in case 2, all auditory skills demonstrated improvement at the postoperative 1-year assessment, highlighting the positive impact of cochlear implant usage. Case 2 had IP-1 cochlear malformation in the ear that received the implant. In addition, case 2 had Cochlear Hypoplasia Type 4 in her normal hearing ear, which made the CI indication stronger due to the possibility of developing hearing loss. IP-1 malformation generally progresses with progressive severe sensorineural hearing loss [7]. Case 2 stated that she noticed her hearing loss at 12. Unlike case 1, case 2 did not undergo newborn hearing screening. Therefore, there is insufficient information to conclude that case 2 has acquired SSD. Although the degree of hearing loss due to inner ear anomaly is not precisely known in case 2, the patient might have realized that she had hearing loss in an environment of multiple speakers even though she probably had congenital hearing loss. In SSD, contralateral afferent pathway dominance, observed in normal hearing, is reduced. Delivery of stimulus from the healthy ear to both hemispheres reorganizes the auditory pathway, leading to aural preference syndrome. In SSD, delayed treatment may decrease the benefit of auditory prostheses such as cochlear implants [8]. The variability in the improvement of auditory skills in case 2, compared to case 1, could stem from the longer duration of hearing loss. Additionally, a cochlear anomaly in case 2 likely contributed to this variability. In conclusion, both cases demonstrated noteworthy improvement in auditory temporal processing skills and speech perception in noise performance due to cochlear implant usage. These findings underscore the efficacy of cochlear implants in promoting the restoration of binaural hearing in individuals with SSD, irrespective of inner ear anomaly.
It has been reported that there is no complaint of tinnitus in the affected ear in congenital SSD, whereas acquired SSD generally involves tinnitus in the affected ear [9]. Case 1, diagnosed with single-sided deafness (SSD), did not report tinnitus before or after cochlear implantation. In the case of case 2, presumed to have congenital hearing loss due to an inner ear anomaly, tinnitus was present both preoperatively and postoperatively. However, the tinnitus observed in case 2 was very mild, only perceivable in quiet environments, as indicated by the THI. Additionally, according to the TQ, it was of a degree that did not pose significant clinical concern and did not increase postoperatively. Regardless of the inner ear anomaly, it was established that SSD did not induce significant tinnitus in either case, and the utilization of cochlear implants did not trigger or exacerbate tinnitus.
Individuals with SSD have difficulty establishing communication in noisy environments, places with poor acoustics, and places with limited direct listening. This has a negative impact on social communication in such patients [10]. Both cases have been found to increase all scores of subscales of SSQ after the surgery compared to the preoperative period. The most dramatic increase due to CI use was observed in the spatial perception subscale in both cases. This result shows that CI effectively increases the quality of life using spatial auditory cues in individuals with SSD. On the other hand, in both cases where the positive impact of the implant on the quality of life was noted, there was a decrease in motivation to use the implant during the first six months postoperatively. Both patients struggled to acclimate to the sound of the cochlear implant during the initial 6 months of implantation. While case 1 had an implant with data logging capabilities, case 2 did not have such features. Therefore, information regarding implant usage was obtained through verbal communication, primarily based on the clinical experience gained from case 1. This feature proves advantageous, enabling clinicians to effectively assess patient progress and tailor interventions accordingly. Additionally, in cases of SSD, more frequent monitoring of cochlear implant usage might be necessary during the initial months. Consequently, we are of the opinion that selecting a CI brand that enables checking the data for the duration of implant use during the implant adaptation period provides an advantage to the clinician.
Conclusion
In SSD cases, cochlear implantation is an effective treatment that improves the auditory skills provided by restoring binaural hearing. This approach, verified to be beneficial by objective and subjective methods, does not cause tinnitus. Selecting a CI brand with a data logging feature would ensure an advantage in follow-up in patients with SSD.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SSD:
-
Single-sided deafness
- CI:
-
Cochlear implant
- GIN:
-
Gaps-in-noise
- SNR:
-
Signal-to-noise ratio
- SSQ:
-
The Speech, Spatial and Qualities of Hearing Scale
- THI:
-
The Tinnitus Handicap Inventory
- TQ:
-
Mini Tinnitus Questionnaire
- PTA:
-
Pure-tone average
References
Noble W, Gatehouse S (2004) Interaural asymmetry of hearing loss, speech, spatial and qualities of hearing scale (SSQ) disabilities, and handicap. Int J Audiol 43(2):100–114. https://doi.org/10.1080/14992020400050015
Firszt JB, Reeder RM, Skinner MW (2008) Restoring hearing symmetry with two cochlear implants or one cochlear implant and a contralateral hearing aid. J Rehabil Res Dev 45(5–8):749–768. https://doi.org/10.1682/jrrd.2007.08.0120
Arndt S, Aschendorff A, Laszig R, Beck R, Schild C, Kroeger S et al (2011) Comparison of pseudobinaural hearing to real binaural hearing rehabilitation after cochlear implantation in patients with unilateral deafness and tinnitus. Otol Neurotol 32(1):39–47. https://doi.org/10.1097/MAO.0b013e3181fcf271
Firszt JB, Holden LK, Reeder RM, Waltzman SB, Arndt S (2012) Auditory abilities after cochlear implantation in adults with unilateral deafness: a pilot stud. Otol Neurotol 33(8):1339–1346. https://doi.org/10.1097/MAO.0b013e318268d52d
Tavora-Vieira D, Boisvert I, McMahon CM, Maric V (2013) Rajan GP (2013) Successful outcomes of cochlear implantation in long-term unilateral deafness: brain plasticity. NeuroReport 24(13):724–729
Gordon-Salant S, Fitzgibbons PJ, Yeni-Komshian GH. Auditory temporal processing and aging: implications for speech understanding of older people. Audiol Res 1(1): 9–15. https://doi.org/10.4081/audiores.2011.e4
Sennaroğlu L, Bajin MD (2017) Classification and current management of inner ear malformations. Balkan Med J 34(5):397–441. https://doi.org/10.4274/balkanmedj.2017.0367
Gordon K, Henkin Y, Kral A (2015) Asymmetric hearing during development: the aural preference syndrome and treatment options. Pediatrics 136(1):141–153. https://doi.org/10.1542/peds.2014-3520
Lee SY, Nam DW, Koo JW, De Ridder D, Vanneste S, Song JJ (2017) No auditory experience, no tinnitus: lessons from subjects with congenital-and acquired single-sided deafness. Hear Res 354:9–15. https://doi.org/10.1016/j.heares.2017.08.002
Wie OB, Hugo Pripp A, Tvete O (2010) Unilateral deafness in adults: effects on communication and social interaction. Ann Otol Rhinol Laryngol 119(11):772–781 (PMID: 21140638)
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Concept—BG, Aİ, EK; design—BG, Aİ, EK; supervision—Aİ, EK; materials—BG; data collection and/or Processing—BG; analysis and/or interpretation—BG; literature review—BG; writing—BG, Aİ, EK; critical review—Aİ, EK. The authors read and approved the final manuscript
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was ethically approved by Eskisehir Osmangazi University’s non-interventional Clinical Research Ethics committee (Decision no.: 49, Date: 20. 06.2023). The written informed consent was obtained from parents in our study.
Consent for publication
All authors consent to the publication of the article in The Egyptian Journal of Otolaryngology.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gumus, B., Incesulu, A. & Kaya, E. Effects of cochlear implantation on auditory temporal processing in single-sided deafness: a report of two cases. Egypt J Otolaryngol 39, 180 (2023). https://doi.org/10.1186/s43163-023-00548-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00548-3