Abstract
Background
Facemasks are routinely used among healthcare providers, especially after the COVID-19 pandemic. However, they negatively impact speech perception. Our study investigated how speech perception using the word discrimination score (WDS) was affected by wearing surgical and KN95 masks while dealing with hearing-impaired healthcare recipients.
Method
This case–control study included 60 participants [15 with normal hearing and 45 with varied degrees of sensorineural hearing loss (SNHL)], for whom word discrimination scores (WDS) were evaluated under various mask conditions.
Results
On applying repeated measures of two-way analysis of variance (RM two-way ANOVA), there was statistically significant interaction (p = 0.0018), meaning that the level by which the mask affects the WDS depends on the underlying hearing level. Both main factors showed a statistically significant effect (p < 0.0001). Surgical masks had a lesser impact on speech discrimination compared to KN 95.
Conclusions
It was concluded that KN95 severely impacted the WDS among all groups relative to surgical mask and the no-mask condition. Although the high-frequency SNHL (HF-SNHL) group had mild hearing loss in the pure tone audiometry (PTA) average, they showed lower WDS relative to the mild to moderate flat SNHL (MM-SNHL). Moderately severe to severe SNHL expressed the worst values. As a result, the surgical mask is recommended over the KN95 mask since it provides better speech discrimination while giving adequate protection. These findings should be taken into consideration as they will have an impact on communication, especially in situations like hospitals where the patients must understand the instructors and healthcare providers very well.
Similar content being viewed by others
Background
Face masks are considered very crucial to protect against infection from upper respiratory tract infections [1]. Many authorities across the world advocate their use in public spaces during pandemics and hospital facilities as a routine. Face masks attenuate the speech acoustic signals and reduce the influence of verbal communication, both of which are important features for message intelligibility [2,3,4]. Facemasks occlude the visual cues obtained from mouth and lip motions, and change speech acoustic aspects that reduce speech discrimination, particularly in a noisy environment or when the listener has hearing impairment [4, 5]. Masks muffle speech sounds, especially higher frequencies that are responsible for the discrimination of similar sounds [3, 6].
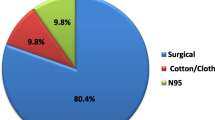
During the COVID-19 pandemic, the two widely used masks were the surgical masks and the KN95 [7]. For optimum protection, the Centers for Disease Control and Prevention (CDC) advises using an NIOSH-approved respirator N95 mask and KN95 followed by a surgical disposable mask and a cloth mask with the least protection [8,9,10]. However, a new systematic review and meta-analysis research published in 2020 revealed that surgical masks and N95 respirators gave similar protection against viral respiratory infection including coronavirus among healthcare workers during non-aerosol-generating care [11]. The impact of those masks, however, varies significantly on how speech is perceived. The higher the barrier level a mask provides, the more significant impact it would have on the voice signals [6, 12, 13].
Previous research regards the effect of wearing facemasks on speech discrimination has been done on normal-hearing individuals [14,15,16], and on patients with hearing impairment [2, 13]. However, in the current study, different levels of SNHL were involved (mild to moderate SNHL, high-frequency SNHL, moderately severe to severe SNHL). Our research, it was aimed to investigate the impact of using surgical versus KN95 masks among healthcare providers on speech discrimination. The routine use of these face masks nowadays among healthcare providers emphasizes the importance of addressing this critical issue. To the authors’ knowledge, it is the first study to investigate the effect of mask-wearing on Arabic speech materials among the Arab population.
Method
This is a prospective observational study comprising 60 subjects [15 subjects with normal hearing and 45 with varied degrees of sensorineural hearing loss], for whom word discrimination scores (WDS) were evaluated under various mask conditions. It was conducted at a tertiary referral hospital, between June 2022 to January 2023. Our Institutional Review Board approved the study (Ethical approval code no. 34941). This study conforms to the Declaration of Helsinki. Every participant provided their informed permission.
Sample size calculation
The sample size and power analysis were established utilizing Epi-info software statistical package version 2002, produced by the World Health Organization and Center for Disease Control and Prevention (Atlanta, GA, USA). With a 95% confidence level, the power analysis showed that enrolling sixty participants would provide our study with 88% power to detect differences in word discrimination scores across groups with different degrees of hearing loss under various mask conditions.
Our study included four groups:
Control group (normal-hearing group)
Normal hearing sensitivity was defined as having pure-tone air-conduction thresholds ≤ 25 dB HL at all audiometric-tested frequencies 250 Hz to 8000 Hz. This group had normal middle ear function as determined by tympanograms and acoustic reflexes.
Mild to moderate SNHL (MM-SNHL)
Patients in this group had hearing thresholds ranging from > 25 to 55 dB on average, at audiometric test frequencies of 250 Hz to 8000 Hz.
High-frequency SNHL (HF-SNHL)
This group included patients with normal-hearing sensitivity (≤ 25 dB) up to 1 kHz and sloping to high-frequency SNHL at a frequency range of 2–8 kHz with a hearing threshold average of > 25 dB on average, at audiometric test frequencies 250 Hz to 8000 Hz.
Moderately severe to severe SNHL (MS-S SNHL)
Patients in this group had an average hearing threshold of 55 to 90 dB at all audiometric-tested frequencies. They all had bilateral symmetrical sensorineural hearing.
All participants age ranged from 18 to 65 years old. They had no systemic diseases or neurological disorders.
Equipment
Pure tone audiometry. Madsen Astera which is a type 1, two channels, and PC-based audiometer with headphones of TDH39 type. Immittancemetry: Interacoustics (AT235) Impedance Audiometer. We assessed the word discrimination across different groups by speech lists that were developed and validated by Soliman et al. [17]. These lists are equal in difficulty. The word recording was made by a native female speaker. She was instructed to speak naturally at a comfortable pitch and pace and to maintain clarity and effort while uttering words. These involved eight lists of open sets of phonetically balanced monosyllabic words. Each list was comprised of 25 words with a score of 4% for each correct word. The words were recorded on Audacity, and they were sampled as WAV to 24-bit/96 kHz which was used for high-resolution recordings. Recordings were made in a double-walled sound-treated room and a microphone was placed perpendicular to the speaker at 0.5 m. The recordings were done under three conditions. The 1st condition was done while the speaker was wearing no masks. The second condition was recorded while the speaker was wearing a surgical mask. The 3rd condition was done while the speaker was wearing the KN95 mask. Figure 1 demonstrates the spectrogram of one word uttered under three different conditions. Signal levels were monitored with an oscilloscope throughout the recording session to confirm that peak signals were not clipped. Then spectrogram of the whole recordings was visually inspected to detect and remove artifacts (non-speech mouth movements, clicks….). All participants were blinded to the recording condition, i.e., they did not know that they were receiving words under different mask conditions.
Procedure
All subjects underwent a detailed audiological history, a thorough otological examination, and a basic audiological evaluation that included pure tone audiometry, speech audiometry, and immittancemetry. Word discrimination score (WDS) test: using the recorded word lists. For each participant, a WDS was established for each ear separately by three different lists (one list without any mask, the second list with the surgical mask, and the third list with the KN95 mask). Three different lists were used for each ear. The presentation level was 40 dB suprathreshold or at the most comfortable level if there was recruitment.
Statistical analysis of the collected data
Results were collected, tabulated, and statistically analyzed by Prism 8 (GraphPad software).
Two types of statistical analysis were done:
Descriptive statistics were expressed in Number (No), percentage (%) mean (x̅), and standard deviation (SD)
Analytic statistics, e.g.
-
Paired t test was employed to compare different readings of normally distributed data in the same group (Rt versus left ear scores). One-way analysis of variance (ANOVA) was applied to compare age between the distinct groups. Chi-square test (χ2) was utilized to compare the sex distribution between distinct groups. Two-way repeated measures ANOVA was applied to compare the WDS among the groups under the different mask conditions. Tukey’s test was utilized as a post hoc test for the correction of multiple tests. A p-value of 0.05 was considered statistically significant. The normality of distribution parameters was evaluated by the D’Agostino and Pearson normality test.
-
GraphPad software’s Prism 8 was used to create the graphics.
Results
Our study included four groups. There were no significant differences between groups as regards age and sex (p value > 0.05). The control group included 15 normal-hearing healthy volunteers from the outpatient clinic (8 males, 7 females) whose ages ranged from 19 to 50 years” 35 ± 9.5 years”. Fifteen participants with MM-SNHL (10 males, 5 females), their ages ranged from 20 to 55 years “38 ± 10 years”. Fifteen participants with HF-SNHL (6 males and 9 females), their ages ranged from 19 to 56 years “39 ± 13 years”. Fifteen participants with MS-S SNHL (7 males and 8 females), their ages ranged from 18 to 55 years “36 ± 12 years”. Since all patients with hearing loss exhibited symmetrical sensorineural hearing loss on both sides, and the results of WDSs showed no significant differences between right and left ears (Paired t test; p > 0.05), so, the values of right and left ears were combined for further analysis. So, there were 30 ears with normal hearing (control group I); 30 ears with MM-SNHL group (group II); 30 ears with HF-SNHL (group III), and lastly 30 ears with MS-S SNHL (group IV). In Fig. 2, we represent the mean ± SD air-conduction thresholds in right versus left ears for the normal-hearing and hearing-impaired groups. WDS (mean ± SD) in normal hearing was 98.9 ± 2.6; 94.27 ± 4.8; 87.2 ± 5.89 under (no mask condition; surgical mask and KN95) respectively. In MM-SNHL it was 96.9 ± 2.9; 90.8 ± 4.7; 82 ± 6.7 under the three conditions. In HF-SNHL, it was as follows 94 ± 3.7; 84.7 ± 6.4; 78 ± 8.5 under the three conditions. Lastly, in MS-S SMHL it was 72 ± 11; 62.9 ± 13.8; 57.6 ± 12.4 under the three conditions (Table 1). Figure 3 represents the scatterplot of WDS in subjects of the study under various mask conditions.
Mean and standard deviation (SD) of pure tone air-conduction thresholds (dB HL) in right versus left ears for the normal-hearing and hearing-impaired subgroups. RT: right, LT: left. MM-SNHL: mild to moderate sensorineural hearing loss, HF-SNHL: high-frequency sensorineural hearing loss, MS-S SNHL: moderately severe to severe sensorineural hearing loss, Hz: hertz, dB HL: decibel hearing level
Scatterplot showing the word discrimination score (WDs) across groups with different degrees of hearing loss under various mask conditions (without mask, with surgical mask, and with KN95 mask). Pure-tone averages (PTA) are represented on the y-axis and word recognition scores (WDS) are represented on the x-axis. A Normal hearing group, B group with mild to moderate-SNHL “MM-SNHL”, C group with high-frequency SNHL “HF-SNHL”, D group with moderately severe to severe SNHL” “MS-S-SNHL”, PTA average “pure tone audiometry average”
RM two-way ANOVA was applied to test the effect of both hearing level and mask effect (the two independent variables) on the word discrimination score (WDS) (the dependent variable), and Tukey’s multiple comparisons was applied as post hoc test. The interaction between the hearing factor and the mask factor was statistically significant (F (6, 232) = 3.646P = 0.0018), meaning that, the manner in which the mask affects the WDS depends on the underlying hearing level (Table 2, Fig. 4).
RM two-way ANOVA was applied to test the effect of both hearing level and mask condition (the two independent variables) on the (WDS) (the dependent variable). The interaction between the hearing factor and the mask factor was statistically significant, meaning that, the manner by which the mask affects the WDS depends on the underlying hearing level. MM-SNHL: mild to moderate sensorineural hearing loss, HF-SNHL: high-frequency sensorineural hearing loss, MS-S SNHL: moderately severe to severe sensorineural hearing loss, WDS: word discrimination scores
Furthermore, the main effect of both mask condition and hearing level were both of higher statistical significance (F (1.742, 202.1) = 396.9 P < 0.0001; F (3, 116) = 100.6 P < 0.0001). That is, the WDS was better while the speaker was wearing (no mask > surgical mask > KN95 mask), and it was also better when the audience had (normal-hearing > MM SNHL > HF SNHL > MS-S SNHL). Following the ANOVA, a post-hoc Tukey’s multiple comparisons test was utilized to compare all scores in pairs. Post hoc multiple comparison tests revealed that.
-
I) Within groups’ analysis (mask factor)
In all groups, WDS under KN95 was the worst relative to surgical mask and relative to no mask condition (Table 3 and Figs. 4 and 5). There were statistically significant differences between the KN95 versus no mask condition, surgical mask versus no mask condition and KN95 versus surgical mask in all groups.
-
II) Between groups’ analysis (hearing level factor)
-
(a)
Under no mask condition: normal hearing group differed significantly from all other groups of hearing loss. The group of HF-SNHL had statistically significantly lower scores than the MM-SNHL (p = 0.01) with a mean difference from the NH of 4.8–2 respectively, although they have better PTA average relative to MM-SNHL. The MS-S SNHL group expressed the worst WDS, (b) Under the surgical mask condition: the groups exhibited the same pattern as in the no mask condition, however, the difference between the MM-SNHL and HF-SNHL was much higher (p = 0.0005). This is owed to the more deterioration that happened to the HF-SNHL under the surgical mask. (c) Under the KN95 condition: both MM-SNHL and HF-SNHL showed further deterioration in WDS and there was no significant difference between both groups (p = 0.19). In all conditions, the WDS in the NH group was more than MM-SNHL which was more than HF-SNHL. Also, this last group had more WDs than MS S-SNHL (Table 4).
-
(a)
Word discrimination score (WDS) at different conditions (no mask, surgical mask, KN95) in different groups (normal-hearing; MM-SNHL; HF-SNHL, and MS-S SNHL) [within group analysis]. NH: normal hearing, MM-SNHL: mild to moderate sensorineural hearing loss, HF-SNHL: mild to moderate high-frequency sensorineural hearing loss, MS-S SNHL: moderately severe to severe sensorineural hearing loss
Discussion
Facemasks are important for preventing disease transmission via aerosols and droplets. Various types including woven fabric masks, surgical, and N95 filtering facepiece respirators (N95 mask) can be used [18]. Surgical and KN95 masks are widely used in the marketplace and give good protection [7]. KN95 has filtering and fitting characteristics, that are responsible for the high barrier level of that mask, but has a greater impact on the voice signals [6, 12] as seen in (Fig. 1).
Mask-wearing is challenging for all populations, particularly those with hearing impairment [19, 20]. The acoustic attenuation of the various masks has an enormous influence on speech perception among this group of populations. These patients with poorer audibility and more distorted spectral resolution will suffer more when communicating with subjects wearing masks [20].
Depending on their barrier effect, masks variably impact the voice signals. Certain masks, particularly the N95/KN95 masks have a profound impact on speech discrimination [3, 4, 6, 12]. Facemasks reduce the speech acoustic signals and act as a low-pass filter that impacts speech perception [2, 3, 6]. Face masks may influence the speech spectrogram (Fig. 1) and decrease vocal intensity [12, 13]. They eliminate the lip readings, which enhance speech recognition and are necessary for some people with hearing loss. [21, 22].
Speech comprehension is a challenge for those with SNHL. This can be attributed to the impairment in their ability to resolve the frequency component of the complex sounds together with the degradation of their ability to process the temporal fine structures [23, 24]. Due to cochlear injury and the resultant reduction in nonlinear cochlear processes, patients with SNHL may have lower frequency selectivity [25]. Earlier studies have demonstrated that the frequency resolution is related to the degree of hearing impairment [26].
This research was designed to investigate the influence of various mask conditions (no mask condition, surgical mask, and KN95 mask) on WDS for listeners of distinct groups of the population (normal hearing, MM-SNHL, HF-SNHL, and MS-S SNHL). The interaction between the hearing factor and the mask factor was statistically significant [F (6, 232) = 3.646; P = 0.0018], meaning that, the manner by which the mask affects the WDS depends on the underlying hearing level. Moreover, the main effects of both the mask factor and hearing level factor on WDS were statistically significant. That means the WDS was better while the speaker was wearing (no mask > surgical > KN95), and it was also better when the audience had (normal-hearing > MM-SNHL > HF-SNHL > MS-S SNHL). The significant main effect for hearing level suggested that listeners with hearing loss had a lower WDS than the listeners with normal hearing. Moreover, the significant main effect for the mask condition showed that the performance under the KN95 was worse than the surgical mask and both were worse than with no mask condition.
-
I.
Within groups’ analysis (mask factor)
In all groups, WDS under KN95 was the worst relative to surgical mask and relative to no mask condition (Table 3 and Figs. 4 and 5). There were statistically significant differences between the KN95 versus no mask condition, surgical mask versus no mask condition, and KN95 versus surgical mask in all groups. KN95 has filtering and fitting characteristics, that are responsible for the high barrier level of that mask, but has a greater impact on the voice signals [6, 12], so, it has the worst significant effect on speech discrimination.
-
II.
Between groups’ analysis (hearing level factor)
-
a)
Under no mask condition
Normal hearing group showed a statistically significant difference from all other groups of hearing loss. The group of HF-SNHL showed more lower scores than the MM-SNHL, although they had a better PTA average relative to the MM-SNHL. There was a statistically significant difference in WDS between MM-SNHL and HF-SNHL (p = 0.01). The MS-S SNHL group expressed the worst WDS.
-
b)
Under the surgical mask condition
The groups exhibited the same pattern as in no mask condition; however, the difference between the MM-SNHL and HF-SNHL was much higher (p = 0.0005). This could be due to the deterioration which occurred in subjects with HF-SNHL under the surgical mask. That is because patients with such types of hearing losses had poorer audibility and spectral resolution in high frequencies and were thus more liable to be influenced by the surgical masks. Subjects with HF-SNHL had difficulty accessing spectral information higher than 2 kHz, a region important for the perception of consonants [25].
-
c)
Under KN95 condition
Both MM-SNHL and HF-SNHL showed deterioration in WDS and there was no significant difference between both groups (p = 0.19). In all conditions the WDS in NH group > MM-SNHL > HF-SNHL > MS S-SNHL). The last group with MS-S SNHL had the worst WDS under the three mask conditions. These patients with poorer audibility and more distorted spectral resolution will suffer more when communicating with people wearing masks [20]. It is documented that patients with poorer hearing have a poorer spectral resolution [25, 26].
-
a)
Previous research investigated the impact of wearing different masks on communication. Some found non-significant differences in speech discrimination between no-mask conditions and different mask conditions in a quiet environment in the normal-hearing population [27, 28]. A study done on forty individuals with normal hearing revealed that speech discrimination with personal protective equipment (N95 + faceshield) was significantly lower than without wearing personal protective equipment [29]. Another study was performed on normal-hearing subjects using speech perception in a noise test under the following conditions (no mask, surgical mask, surgical mask with shield), they found that the performance under the surgical mask was statistically significantly different from the no mask condition. However, the greatest effect occurred when the face shield was added [14]. Toscano and Toscano [16] reported that, at a low level of noise, the three mask types (surgical, N95, and 2 different cloth masks) showed no significant effect on speech recognition. However, at a prominent level of noise, the difference in speech recognition was more apparent with the homemade cloth and N95 masks.
Few researches were done to study the influence of different masks on hearing loss populations. Mendel et al. [28] reported no significant differences in hearing loss under the surgical mask in quiet, but in noise, there was a detrimental effect. Atcherson et al. [2] performed their study on normal hearing, moderate hearing impairment, and severe profound hearing impairment; and under three mask conditions: no mask, standard paper surgical mask, and transparent surgical mask. The authors noticed that the individuals with normal hearing performed consistently well through all conditions. However, a comparison between normal and hearing impairment groups revealed statistically significant differences between the participants with normal hearing and those with severe-to-profound hearing impairment for all types of masks. A more recent study was done by Moon et al. [13] to test the effect of N95 mask-wearing on speech perception in subjects with normal hearing and those with bilateral moderate SNHL. The authors reported that in the case of the absence of visual cues, there were statistically significant differences between speech understanding with and without masks in both study groups.
The discrepancies among previous studies were multifactorial, which might be due to differences in methodology, study design, the condition of the test (type of mask, speech signal), and the population under the test (normal hearers versus patients with SNHL). However, future research should be done on a larger number of participants with distinct levels of hearing loss, under diverse types of masks (surgical, cotton, transparent, face shield…) while using more challenging stimuli, i.e., speech in noise.
Conclusions
Surgical masks have less effect on speech discrimination in all groups compared to KN95. Participants with high-frequency hearing loss are more susceptible to the negative effects of face masks. So, it is recommended to use surgical masks rather than the KN95, especially in situations that do not necessitate high degrees of protection. These findings should be taken into consideration as they will have an impact on communication, especially in situations like hospitals where the patients must understand the instructors and the healthcare providers very well.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author.
References
Chu DK, Akl EA, Duda S, Solo K, Yaacoub S et al (2020) Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The lancet 395:1973–1987
Atcherson SR, Mendel LL, Baltimore WJ, Patro C, Lee S et al (2017) The effect of conventional and transparent surgical masks on speech understanding in individuals with and without hearing loss. J Am Acad Audiol 28:58–67
Corey RM, Jones U, Singer AC (2020) Acoustic effects of medical, cloth, and transparent face masks on speech signals. J Acoust Soc Am 148:2371–2375
Palmiero AJ, Symons D, Morgan JW III, Shaffer RE (2016) Speech intelligibility assessment of protective facemasks and air-purifying respirators. J Occup Environ Hyg 13:960–968
Bond Z, Moore TJ, Gable B (1989) Acoustic–phonetic characteristics of speech produced in noise and while wearing an oxygen mask. J Acoust Soc Am 85:907–912
Gama R, Castro ME, van Lith-Bijl JT, Desuter G (2021) Does the wearing of masks change voice and speech parameters? Eur Arch Otorhinolaryngol 279:1701–1708
Bussan DD, Snaychuk L, Bartzas G, Douvris C (2022) Quantification of trace elements in surgical and KN95 face masks widely used during the SARS-COVID-19 pandemic. Sci Total Environ 814:151924
Asadi S, Wexler AS, Cappa CD, Barreda S, Bouvier NM (2019) Ristenpart WDJSr. Aerosol emission and superemission during human speech increase with voice loudness 9:1–10
MacIntyre CR, Seale H, Dung TC, Hien NT, Nga PT et al (2015) A cluster randomised trial of cloth masks compared with medical masks in healthcare workers 5:e006577
Bourouiba LJJ (2020) Turbulent gas clouds and respiratory pathogen emissions: Potential implications for reducing transmission of COVID-19. JAMA 323:1837–8
Bartoszko JJ, Farooqi MAM, Alhazzani W, Loeb M (2020) Medical masks vs N95 respirators for preventing COVID-19 in healthcare workers: a systematic review and meta-analysis of randomized trials. Influenza Other Respir Viruses 14:365–373
Nguyen DD, McCabe P, Thomas D, Purcell A, Doble M et al (2021) Acoustic voice characteristics with and without wearing a facemask. Sci Rep 11:1–11
Moon J, Jo M, Kim G-Y, Kim N, Cho Y-S et al (2022) How does a face mask impact speech perception? Proc. Healthcare 10:1709 (MDPI)
Wittum KJ, Feth L, Hoglund E (2013) The effects of surgical masks on speech perception in noise. Proc Meet Acoust ICA2013 19:060125
Rahne T, Fröhlich L, Plontke S, Wagner L (2021) Influence of face surgical and N95 face masks on speech perception and listening effort in noise. PLoS ONE 16:e0253874
Toscano JC, Toscano CM (2021) Effects of face masks on speech recognition in multi-talker babble noise. PLoS ONE 16:e0246842
Soliman S (1985) Speech discrimination audiometry using Arabic phonetically balanced words. Ain Shams Med J 27:27–30
O’Dowd K, Nair KM, Forouzandeh P, Mathew S, Grant J et al (2020) Face masks and respirators in the fight against the COVID-19 pandemic: a review of current materials, advances and future perspectives. Materials 13:3363
Chodosh J, Weinstein BE, Blustein J (2020) Face masks can be devastating for people with hearing loss. BMJ 370:m2683. https://doi.org/10.1136/bmj.m2683
Homans NC, Vroegop JL (2021) Impact of face masks in public spaces during COVID-19 pandemic on daily life communication of cochlear implant users. Laryngoscope Investig Otolaryngol 6:531–539
McGurk H, MacDonald J (1976) Hearing Voices and Seeing Eyes. Nature 264:746–748
Lalonde K, McCreery RW (2020) Audiovisual enhancement of speech perception in noise by school-age children who are hard of hearing. Ear Hear 41:705–719
Lorenzi C, Gilbert G, Carn H, Garnier S, Moore BC (2006) Speech perception problems of the hearing impaired reflect inability to use temporal fine structure. Proc Natl Acad Sci 103:18866–18869
Nada NM, Kolkaila EA, Gabr TA, El-Mahallawi TH (2016) Speech auditory brainstem response audiometry in adults with sensorineural hearing loss. EJENTAS 17:87–94
Başkent D (2006) Speech recognition in normal hearing and sensorineural hearing loss as a function of the number of spectral channels. J Acoust Soc Am 120:2908–2925
Peters RW, Moore BC (1992) Auditory filter shapes at low center frequencies in young and elderly hearing-impaired subjects. J Acoust Soc Am 91:256–266
Magee M, Lewis C, Noffs G, Reece H, Chan JC et al (2020) Effects of face masks on acoustic analysis and speech perception: implications for peri-pandemic protocols. J Acoust Soc Am 148:3562–3568
Mendel LL, Gardino JA, Atcherson SR (2008) Speech understanding using surgical masks: a problem in health care? J Am Acad Audiol 19:686–695
Bandaru S, Augustine A, Lepcha A, Sebastian S, Gowri M et al (2020) The effects of N95 mask and face shield on speech perception among healthcare workers in the coronavirus disease 2019 pandemic scenario. J Laryngol Otol 134:895–898
Acknowledgements
None
Funding
There were no funding resources for our study.
Author information
Authors and Affiliations
Contributions
Contributor NN was the chief investigator and was responsible for the data analysis. Contributor RML was responsible for the organization and coordination of the trial. NN, MOT, and RML developed the trial design. All authors contributed to the writing of the final manuscript. All members of the study team contributed to the management or administration of the trial. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation (Research Ethics Committee, Tanta University; Approval code: 34941). Every participant provided their informed permission.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nada, N., Tomoum, M.O. & Lasheen, R.M. How can the routine use of face masks by medical professionals affect hearing-impaired patients’ perception of speech? A case–control study. Egypt J Otolaryngol 39, 161 (2023). https://doi.org/10.1186/s43163-023-00520-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00520-1








