Abstract
Background
In otolaryngology outpatient clinics, patients frequently present with unilateral vocal cord paralysis (UVCP). During the pandemic, various new protocols were designed to identify UVCP. An experienced otolaryngologist must conduct a thorough history-taking, examination, and investigation to determine the cause of UVCP.
Objectives
To evaluate various causes of UVCP during the pandemic.
Methods
Thirty patients with UVCP on 70-degree rigid endoscopy were studied. Detailed general and systemic examinations were done. All COVID-19 precautions were followed during the evaluation, and real-time reverse transcription-polymerase chain reaction was done before the endoscopic procedure. High-resolution computed tomography scan of skull base to mediastinum with contrast was performed for etiology. Patients were treated according to the standard protocols. Follow-up at 1, 3, and at 6 months was performed.
Results
The mean age was 42.3 ± 14.83 years. All the patients had presented with a change in voice. Twenty percent had UVCP post a surgical procedure. No cause could be found in 16.67% of patients. Five patients had succumbed to complications relating to their other prevailing conditions. At 6 months, 10 patients continued to have palsy, 9 showed paresis, and 6 showed complete mobility of the cords.
Conclusion
During the pandemic, diagnosing and following up such patients were a challenge. Investigating a cause of UVCP, the symptoms of which might be trivial at presentation, leads to discover a much sinister cause. UVCP in post-covid mucormycosis was an entity requiring multimodality management. Pandemic-induced restrictions lead to formulations of newer protocols for tackling this entity.
Similar content being viewed by others
Background
The COVID-19 pandemic was heralded by the SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) in the year 2019. With the morbidity and mortality rate of around 3.4%, this viral agent had varied neurotrophic effects apart from primarily affecting the respiratory tract.
The COVID-19 era brought new obstacles in the field of ENT as, being a droplet infection, it meant increased exposure to the ENT specialists in OPDs and delayed diagnosis of basic conditions due to the requirement of mandatory RTPCR. In the wake of the pandemic, use of rigid 70-degree endoscope for the evaluation of larynx was thus restricted.
Unilateral vocal cord palsy (UVCP) is an often-encountered entity in outpatient clinics. Patients can present with varied symptoms like change in voice in the form of breathy voice, vocal fatigue, swallowing difficulties, weak cough, or the sensation of shortness of breath [1].
It is not a disease entity per se but a sign of an underlying disease process that can be central or peripheral. Proper evaluation and treatment can aid in the restoration of the normal function of vocal cords. Due to the ongoing pandemic, surgical interventions were limited, and conservative line of management was adopted. Also, the COVID restrictions prevented patients from acquiring early care and assessments. The present study evaluates the various etiologies of UVCP and evaluation of UVCP in the pandemic.
Methods
A single-site, observational prospective study was performed at the Department of ENT of a tertiary healthcare centre from November 2019 to May 2021 on 30 consecutive cases of UVCP on 70-degree rigid endoscopy.
All consenting patients above 18 years of age, of either sex, who had presented with hoarseness of voice, breathlessness, aspiration, and incidentally diagnosed as UVCP, and all who were not previously treated/undertaking treatment were included. Patients with laryngeal malignancies were also excluded.
A valid written informed consent was obtained from all the patients at the time of recruitment. A detailed history of the participants was taken. Patients were asked about any history of fever, URTI, trauma, neck surgery, hospitalisation, immunocompromised status, addictions, and COVID-19 vaccination. Detailed general and systemic examinations were done for all the patients. All COVID-19 precautions were followed during the evaluation (Fig. 1), and RT-PCR was done before the endoscopic procedure.
Clinical assessments
-
Seventy-degree Hopkin’s rigid endoscopy: It provided information regarding the mobility of vocal cords and thus the affected side, arytenoid mobility, the presence of any phonatory gap, compensation by opposite side cord (unaffected side), and structural abnormalities of the vocal cord or another part of the larynx.
-
High-resolution computed tomography scan of skull base to mediastinum with contrast: This was done in all the patients to find out the etiology of the vocal cord palsy and features suggestive of UVCP.
-
Voice assessment: Maximum phonation time (MPT) was obtained by instructing the patient to sustain the vowel /‘A’/ for as long as possible after deep inspiration, vocalising at a comfortable frequency and intensity. Three separate measurements were taken, and the longest MPT was registered.
-
Ultrasonography of larynx (Fig. 2): Using transcutaneous laryngeal sonography for vocal fold movement assessment as a screening tool specially when RT-PCR report of COVID-19 was not available.
Trans-cervical laryngeal ultrasonography was used to assess the vocal cord mobility as a screening tool for UVCP. This reduced the aerosol exposure to the healthcare professional due to conventional endoscopic examination during the pandemic. Trans-cervical laryngeal USG of a patient with normal mobility of cords whereby a shows abducted cord and anterior commissary (yellow arrow). b Shows adducted cords. c USG for vocal cord mobility being performed during the COVID-19 pandemic. d Left vocal cord palsy as seen on the USG
Follow-up
All the patients were treated according to the standard protocols. They were started on conservative management with speech and swallowing therapy and instructed about vocal hygiene and on anti-reflux medications like proton-pump inhibitors. Patients with specific conditions like skull base osteomyelitis, tuberculosis, mucormycosis, sarcoidosis, and malignancies were given appropriate and specific treatmen. Tables 1, 2 and 3.
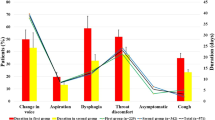
The patients were asked to follow-up at 1, 3, and at 6 months. Patients were reassessed based upon symptomatology, MPT, and 70-degree endoscopy on each visit. Figs. 3, 4, 5, 6 and 7.
A 58-year-old female case of post-COVID mucormycosis with multiple cranial nerve palsies. a Clinical photo. b CT paranasal sinus showing irregular mucosal thickening of sinuses. c Skull base involvement seen on T2-weighted MRI. Patient had left unilateral vocal cord palsy, left facial nerve palsy, and d neuromuscular incoordination of distal segment of oesophagus (Barium swallow)
A 21-year-old female presented with recent onset change in voice. The patient was 32-week pregnant and was a diagnosed case classical Hodgkin’s lymphoma. The patient was taking chemotherapy for the same. The patient had left vocal fold paralysis. a, b, and c MRI reveals a mediastinal mass causing compression of the left RLN and intrauterine foetus. The patient underwent a planned caesarean section at 36-week period of gestation
A 22-year-old female in immediate postpartum period presented with difficulty in breathing and neck swelling. On clinical evaluation, patient had left UVCP with retrosternal extension of the thyroid swelling. Patient suffered cardiac insufficiency, and post-mortem histopathology of the thyroid swelling revealed lymphoma. a Clinical picture and b CT of laryngeal region indicate features of left vocal cord palsy which are medialisation and thickening of aryepiglottic fold, anteromedial deviation of arytenoid cartilage. The presence of enlarged left lobe of thyroid with erosion of the thyroid cartilage is seen. c and d CT scan of the neck and thorax reveals retrosternal extension with airway compromise
A 52-year-old male with change in voice and dysphagia presented to us. USG larynx (before RT-PCR report) revealed cord paralysis. On confirmation of right UVCP, CT was advised. a CT thorax, axial section showing oesophageal growth causing compression of left RLN at the trachea-oesophageal groove. b Barium swallow skiagram of same patient revealed mid-oesophageal narrowing. The patient was then referred to the oncology department for further management. Unilateral vocal fold paralysis in this patient leads us to discover a much sinister cause
A 60-year-old female presented to us with hoarseness and aspiration along with giddiness. Endoscopic evaluation revealed left UVCP, whereby there was also pooling of saliva. This indicated high vagal lesion affecting both RLN and superior laryngeal nerve. a and b MRI brain coronal section suggestive of acute non-haemorrhagic infarct in left posterolateral medulla oblongata (Wallenberg syndrome)
Statistical analysis
All the data was analysed using IBM SPSS ver. 25 software. Frequency distribution was performed to prepare the tables. Quantitative data were expressed as mean and standard deviation, whereas categorical data were expressed as numbers and percentages.
Results
The mean age of the patients who presented with UVCP was 42.3 ± 14.83 years, the youngest patient being 18 years of age and the oldest patient being 75 years of age. The most common age group was 29–48 years (46.47%), 20% had age between 18 and 28 years, whereas 33.2% had aged ≥ 49 years. Male patients comprised 60%, and females comprised 40% of the patients recruited.
Discussion
UVCP, a commonly encountered challenge in otolaryngology, is not a disease entity per se. In fact, it is often a tell-tale sign of an underlying disease or an iatrogenic injury. Its correct management depends upon the speedy delineation of its cause. If temporary, UVCP can well recover within 6–12 months, aided by speech therapy and specific measures like injection laryngoplasty. In cases with permanent UVCP, intervention would be limited to improving the voice, preventing aspiration and decreasing voice fatigue [2].
During the COVID pandemic, there was a paradigm shift in the diagnostic protocol of these cases. Since the oral cavity is identified as a high-risk infectivity site, every patient had to be subjected to COVID RT-PCR prior to 70-degree scopy. Patients who tested positive had to be excluded. To further reduce the risk of transmission, pre-procedure mouthwash with povidone iodine was compulsorily done. According to a study conducted by Martinez et al. in 2020, povidone iodine reduced the viral load of SARS-COV-2 in saliva to almost undetectable limits, and the effects lasted for nearly 3–4 h [3].
Though scientific data is replete with data on UVCP in the western population, scanty information is available from India. Hence, our aim was to improve this data. However, due to the advent of the pandemic, lack of transport facilities and change in management protocols made data collection and treatment very challenging. We have a significant difference in the age distribution. Shafkat et al. have reported an incidence of 0.42% with most patients presenting in the 5th and 6th decades (77.2%) [4]. In our study, most patients were in their 3rd and 4th decades. This difference in age distribution may be explained on the basis of higher life expectancy in Western population and also a possible neuropathic effect of the SARS-COV-2, the pathophysiology of which still needs validation and elaboration.
In our study, the number of patients having left-sided UVCP was marginally higher. These results are similar to those of Anil et al., [5] who found 52% with left sided and 48% with right-sided palsy.
In this study, hoarseness of voice was the presenting symptom in all patients (100%). In addition to hoarseness, 50% of the patients also had vocal fatigue, 20% patients had symptoms suggestive of aspiration, 6.67% patients presented with stridor, and 3.33% also had dysphagia. Our findings were similar to those of Toutounchi et al. [6], where voice change was seen in 97.8% and aspiration in 37.8%. However, vocal fatigue was not much highlighted in other studies. In contrast, voice fatigue was the second most common symptom in our study.
Hoarseness is the most common complaint because these patients almost always have a phonatory gap, making their voices breathy and challenging to understand. Vocal fatigue is the second most common symptom because patients often run out of air when the vocal cords fail to approximate. This is demonstrated by the reduced maximum phonation time (MPT) and glottal incompetence. In addition, glottal closure is needed to create positive end-expiratory pressure (PEEP). Thus, a few patients with immediate postoperative UVCP can experience decreased pulmonary function because of loss of the natural PEEP that happens with adequate glottal closure. Aspiration can be present in UVCP if the site of lesion is high vagal, where there is superior laryngeal nerve (SLN) involvement along with recurrent laryngeal nerve (RLN). SLN involvement also causes significant anaesthesia of the pharynx. In the current study, the stridor present in 2 patients may be a confounding symptom of the pathology, which was actually due to significant retrosternal extension of thyroid swelling causing tracheal compression. Dysphagia, found in one case in our study, was attributed to oesophageal malignancy.
In this study, patients presenting with UVCP had varied etiologies. Majority (20%) of patients had UVCP post surgery. Thyroidectomy was the most common iatrogenic cause of UVCP in the present study. Another iatrogenic cause for post-intubation UVCP is seen in two patients.
Other causes included thyroid malignancy, oesophageal malignancy, blunt trauma, Guillain–Barre’ syndrome, and skull base osteomyelitis (one patient each). Two patients had cerebral infarcts, one of them presenting as Wallenberg syndrome. The interesting finding was two patients who developed UVCP after suffering from post-COVID-19 mucormycosis. In this study, we also found involvement of VII and X nerves. The exact mechanism of nerve involvement is not known. However, a direct neurotoxic effect of the COVID virus has been hypothesised [7]. We had two patients of tubercular mediastinal lymphadenopathy leading to UVCP by mechanical compression of the RLN. Apart from all the above patients, the remaining 5 were classified as idiopathic cases. In the study carried out by Pavithran et al., the most common cause of UVCP was idiopathic [8].
In our study, special care was taken to prevent exposure of the healthcare professionals from risk of COVID infection, by developing new protocols. COVID-positive subjects were excluded, and all patients were given povidone iodine mouthwashes prior to examination. The aid of sonography of the larynx was used for diagnosis of UVCP. This modality can serve for imaging of the vocal cord immobility and has been hitherto under-utilised. Often, there is a lack of experience in usage and availability of laryngeal endoscope. However, current guidelines encouraged us to use less aerosol-generating procedures. USG larynx for cord mobility proved to be a dark horse for our department and aided in proper screening of the patients. UVCP was correctly diagnosed by USG in approximately 70% of our 30 cases on their preliminary visits. This finding was in concordance with the study by Shah et al. [9] who reported excellent values in terms of sensitivity, specificity, positive predictive value, and negative predictive value of transcutaneous laryngeal USG in the assessment of vocal cord mobility as compared with video-laryngoscopy in patients undergoing thyroidectomy. It proved to be an excellent noninvasive, bedside screening tool for assessing vocal cord palsy postoperatively. However, there is a relatively difficult learning curve for this modality and a less well-versed protocol.
In the present study, on subsequent follow-up at 3 months, 15 patients continued to have palsy same as during presentation. Five patients had developed flickering movements, and five had complete cord mobility. However, five patients had succumbed to complications relating to their other prevailing conditions. On 6-month visit, 10 patients continued to have palsy same as during presentation, 9 showed partial paresis, and 6 showed complete mobility of the cords. The patients were given speech therapy and taught vocal hygiene. The patients with tuberculous mediastinal lymphadenopathy were started on antitubercular treatment.
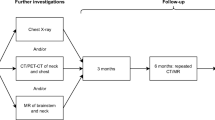
In the course of our study, we worked out a protocol for the evaluation of a patient of UVCP. Upon encountering symptoms pertaining to UVCP, the RT-PCR swab is taken with adequate use of personal protection equipment (N95 masks, double gloves, FDA-approved gowns, face shield). While awaiting the swab reports, the patient underwent radio-imaging in the form of USG of larynx as well as CT scan. The radio-imaging was carefully correlated so as to not only diagnose but also identify the etiology. Once the scab report was negative, the healthcare worker performed the endoscopy of the larynx. This endoscopy was also performed after the patient performed povidone iodine gargles. Donning of the PPE was a dictum as there is a high likelihood of acute COVID-19 among the RTPCR-negative individuals [10].
Conclusion
Unilateral vocal cord palsy is a relatively common diagnosis in the ENT OPD. The patient usually presents insidiously with change or fatigue in voice. Every patient requires proper investigations to pinpoint the exact cause as the etiology is widely varied.
During the COVID pandemic, there was a change in the diagnostic and management protocol, keeping in mind the possibility of newer etiologies and safety of the healthcare personnel. These changed protocols were applied during our study with special emphasis on prompt and accurate work-up, ensuring a speedy diagnosis.
The results in our study revealed iatrogenic vocal cord palsy to be the most common cause. This fact underscored the need to properly delineate the anatomy in order to avoid this complication. Also, attempts for salvaging of iatrogenic UVCP surgically yield poor results due to the intricate anatomy of the RLN and vagus nerve. Other causes of UVCP were also detected in our study, namely, mediastinal masses, oesophageal malignancy, and tuberculosis. We also noted two cases of post-COVID UVCP, which was a novel finding.
In conclusion, UVCP has an insidious and seemingly trivial presentation. Proper investigations may reveal a sinister cause. Even the best surgical or medical management may not yield fruitful results, and noninvasive management like speech therapy would remain the only options for palliative treatment. Hence, the best strategy would be to focus on prevention and early treatment of UVCP.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Williamson AJ, Shermetaro C. Unilateral vocal cord paralysis.. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535420/. Accessed on 10 Aug 2022. Updated 2022 Feb 7
Ryu CH, Kwon TK, Kim H, Kim HS, Park IS, Woo JH, et al. Guidelines for the management of unilateral vocal fold paralysis from the Korean Society of Laryngology, Phoniatrics and Logopedics. Clinical and Experimental Otorhinolaryngology. 2020;13(4):340–60. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7669319/
Martínez Lamas L, Diz Dios P, Pérez Rodríguez MT, Del Campo Pérez V, Cabrera Alvargonzalez JJ, López Domínguez AM, et al. Is povidone iodine mouthwash effective against SARS-CoV-2? First in vivo tests. Oral Dis. 2022;28 Suppl 1(S1):908–11. Available from: https://doi.org/10.1111/odi.13526
Shafkat A, Muzamil A, Lateef M (2002) A study of incidence and etiopathology of vocal cord paralysis. I dial Journal of Otolaryngology-Head Neck Surg. 54(4):294–6
Anil HT, Lasya Raj N, Pillai N (2019) A study on etiopathogenesis of vocal cord paresis and palsy in a tertiary centre. Indian J Otolaryngol Head Neck Surg 71(3):383–389
Seyed Toutounchi SJ, Eydi M, Golzari SE, Ghaffari MR, Parvizian N. Vocal cord paralysis and its etiologies: a prospective study. J Cardiovasc Thorac Res. 2014;6(1):47–50. https://doi.org/10.5681/jcvtr.2014.009. Epub 2014 Mar 4. PMID: 24753832; PMCID: PMC3992732
Jungbauer F, Hülse R, Lu F, Ludwig S, Held V, Rotter N, Schell A (2021) Case report: bilateral palsy of the vocal cords after COVID-19 infection. Front Neurol 19(12):619545
Pavithran J (2011) Unilateral vocal cord palsy: an etiopathological study. Int J Phonosurgery and Laryngology 1(1):5–10
Shah MK, Ghai B, Bhatia N, Verma RK, Panda NK. ☆Comparison of transcutaneous laryngeal ultrasound with video laryngoscope for assessing the vocal cord mobility in patients undergoing thyroid surgery. Auris Nasus Larynx. 2019;46(4):593–8. Available from: https://doi.org/10.1016/j.anl.2018.12.007
Parmar H, Montovano M, Banada P, Pentakota SR, Shiau S, Ma Z, et al. RT-PCR negative COVID-19. BMC Infect Dis. 2022;22(1):149. Available from: https://doi.org/10.1186/s12879-022-07095-x
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Dr. AS, responsible for collection, compiling and analysis of all data, and drafting the article and revising it critically for important intellectual content. Dr. HM, PI, conception and design of the study and guided the authors to work for the publication, ensured ethical compliance, and final approval of the version to be published. Dr. AG, helping in clinical examination and record keeping. Dr. AA, helping in clinical examination and data collection. Dr. KN, helping data collection and analysis. Dr. MJ, helping data collection and analysis. Dr. SK, helping data collection and analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study obtained ethical clearance from the Institutional Ethics Committee (IEC-II), Seth G.S. Medical College & KEM Hospital Mumbai (project number: EC/163/2019). Letter no. IEC(II)/OUT/656/2020 dated 22nd December 2020. A written informed consent was taken from the participants in the language best understood by the patient. All the patients who had consented to participate were only included in the study. The consents had been verified by the IEC(II) of Seth G. S. Medical College & KEM Hospital, Mumbai.
Consent for publication
A written informed consent was taken by the individual participants for publication of the details pertaining to them in the study while keeping the identities anonymous. This was explained to all consenting participation in the written informed consent in the language best understood by them. The same was verified by the IEC(II).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sahai, A., Marfatia, H., Gaikwad, A. et al. Unilateral vocal cord palsy during COVID-19 era: a study from a tertiary care centre in India. Egypt J Otolaryngol 39, 144 (2023). https://doi.org/10.1186/s43163-023-00501-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00501-4