Abstract
Background
Osteomas are benign slow-growing tumors, which typically arise on the surface of the bone. They rarely arise from the temporal bone, accounting for 0.1–1% of all benign tumors of the skull. The external auditory canal (EAC) is the most common site for osteomas in the temporal bone. Other extra-canalicular osteomas of the temporal bone are uncommon and infrequently reported. In this case report, we discuss the clinical presentation and surgical management of osteoma of the squamous part of the temporal bone. A limited review of literature is also presented.
Case presentation
A 20-year-old male presented to the outpatient department (OPD) with a chief complaint of a hard swelling above his left ear, for 4 years. He had no other complaints other than cosmetic concern. On examination, there was a solitary, smooth, bony hard swelling just antero-superior to the left pinna, and the overlying skin was unremarkable. The left EAC and tympanic membrane were normal. A non-contrast computed tomography (CT) scan of the head and face with 3-D reconstruction showed a16 × 18 mm exophytic, pedunculated bony lesion arising from the squamous part of the temporal bone suggestive of an osteoma. The patient was taken up for surgical excision under general anesthesia. The bony lesion was removed from its attachment to the skull using a gouge and a mallet. The base of the tumor was drilled using a polishing burr to ensure complete removal and prevent recurrence. The histopathology was confirmatory of compact osteoma. Postoperative period was uneventful, and follow-up at 18-month post-surgery did not reveal any recurrence clinically.
Conclusion
Osteoma of the temporal squama is rarely reported, and surgical excision is the definitive treatment if symptomatic. This case report highlights the surgical management of this rare tumor. A limited review of literature suggests that squamous part of the temporal bone is an unusual site for extra-canalicular osteomas, and the prognosis is good after surgery.
Similar content being viewed by others
Background
Osteoma is a benign slow-growing mesenchymal osteogenic tumor comprising of well-differentiated bone [1, 2]. In the head and neck region, osteomas are known to emerge from the skull, mandible, and facial bones [2]. Temporal bone osteomas are rare and commonly arise from the external auditory canal [3]. Gardener’s syndrome, previous surgery, radiotherapy, trauma, chronic infection, and pituitary gland dysfunction are reported causes for development of osteomas [1]. The aim of this case report is to discuss the clinical and radiological presentation and surgical management of a rare case of osteoma of squamous part of the temporal bone. Another objective of this report is to present a limited review of literature.
Case presentation
A 20-year-old male presented to the outpatient department (OPD) with a chief complaint of a hard swelling above his left ear, noticed since 4 years, which was insidious in onset and gradually progressing in size. He had no other complaints other than cosmetic concern. There was no additional history suggestive of ear infection or trauma. On examination, there was a solitary, smooth, bony hard swelling just antero-superior to the left pinna, and the overlying skin was unremarkable. The left external auditory canal (EAC) and tympanic membrane were normal. A non-contrast high-resolution computed tomography (HRCT) scan of the temporal bones and 3-D reconstruction of the face showed a 16 × 18 mm exophytic, pedunculated bony lesion arising from the squamous part of the temporal bone suggestive of an osteoma (Figs. 1 and 2a–b). There was no similar bony lesion elsewhere in the craniofacial region.
The patient was taken up for surgical excision under general anesthesia. A 3-cm vertical incision was made above the pinna starting at the attachment of the root of helix. Subcutaneous flaps were raised anteriorly and posteriorly. The temporalis muscle was separated and retracted superiorly and inferiorly to expose the bony lesion completely. The pedicle of the lesion was identified at its posteroinferior aspect. The bony lesion was removed from its attachment to the skull using a gouge and a mallet (Figs. 3 and 4). The base of the tumor was drilled using a polishing burr to ensure complete removal and prevent recurrence. The surgical wound was closed in 3 layers, and the postoperative period was uneventful. The histopathology was confirmatory of compact osteoma (Fig. 5). Postoperative period was uneventful, and follow-up at 18-month post-surgery did not suggest any recurrence clinically.
Discussion
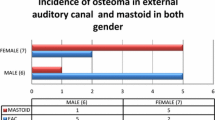
Osteomas of the temporal bone are rare, constituting 0.1–1% of all benign tumors of the skull [3, 4]. Osteomas are seen more frequently in men (male:female ratio 1.5:1), with a mean age of 50 years [5]. The most common site of origin for osteomas in the temporal bone is the external auditory canal. Mastoid process is the most frequent extra-canalicular site for osteomas involving the temporal bone [1]. Other rare sites in the temporal bone where osteomas arise are internal auditory canal, petrous apex, middle ear, and glenoid fossa [6,7,8]. They are mostly asymptomatic and present as painless slow-growing swellings [7, 9, 10]. The symptoms are based on the location, tumor size, and local extension. When they occur in the squamous part of the temporal bone, patients usually consult for cosmetic concerns [1, 9, 10]. Occasionally, osteomas of the internal auditory canal can compress the seventh and eighth cranial nerves manifesting as facial palsy and sensory-neural hearing loss [4, 6]. Osteomas involving the EAC are usually unilateral, solitary, and pedunculated arising from the tympanomastoid suture at the bony cartilaginous junction [11]. They are slow growing and asymptomatic but can cause recurrent ear discharge, external auditory canal cholesteatoma, and conductive hearing loss if there is significant canal obstruction [1, 11].
Reported etiological factors have included hereditary (Gardener’s syndrome), surgery, radiotherapy, trauma, chronic infection, and pituitary gland dysfunction [1, 7, 8]. No definitive etiology could be identified in our patient. Histologically, osteomas are composed of well-differentiated mature cancellous bone, characterized by dense lamellae with organized Haversian canals and fibrofatty marrow with small blood vessels [1]. Osteomas can be classified histologically into compact (cancellous), spongiotic, and mixed subtypes, the former being the most common [1, 4, 7]. CT scan with 3-D reconstruction is the best imaging modality as it precisely localizes the tumor [12]. On CT, they are seen as well-defined hyperdense outgrowths of the bone [2, 4, 10]. Osteoid osteomas, osteoblastomas, ossifying fibromas, fibrous dysplasia, chondromas, osteochondromas, Paget’s disease, and giant cell tumors can have a similar presentation in this location and should be considered as differentials [7].
Surgical excision is the treatment of choice for temporal bone osteomas [6, 7]. Asymptomatic osteomas can be kept under observation with regular follow-up and imaging [9]. For osteomas arising from cortical bone, the base of the tumor must be drilled until normal cortical bone is seen to prevent recurrence [4, 7, 10]. Cortical mastoidectomy is advised if the mastoid air cells are involved [3, 7]. Malignant transformation of osteoma has not been reported [9, 12].
A review of literature of the reports of extra-canalicular osteomas of temporal bone, published in the English language from the PubMed database using keywords such as osteoma, temporal bone, mastoid, squama, and extra-canalicular and squamous part of temporal bone in various combinations, from the year 2012 to 2022 is also presented (Table 1). Only those case reports which give information about the indication for surgery and histopathology were included.
In our review, male to female ratio is 1:4, and age at presentation ranged from 13 to 59 years. The most frequent extra-canalicular site for temporal bone osteoma was the mastoid part of the temporal bone. The most common indication for surgery for mastoid osteomas was due to cosmetic concerns, followed by pain. Hearing loss was seen in a middle ear osteoma arising from the incus [18]. Trigeminal neuralgia was seen in an osteoma involving the petrous apex impinging on the 5th cranial nerve [17]. The largest mastoid osteoma in our review measured 7 cm in the largest dimension [16]. The most common histological subtype of osteoma reported was compact osteoma. Recurrence was not documented in any of the case reports.
Conclusion
Osteomas rarely occur in the temporal bone and are usually asymptomatic, presenting mostly as painless swellings. Osteoma of the temporal squama is rarely reported, and surgical excision is the definitive treatment if symptomatic. Excision is done through the pedicle, and the base is drilled to prevent recurrence. This case report highlights the surgical management of this rare tumor. The review of literature suggests that squamous part of the temporal bone is an unusual site for extra-canalicular osteomas, and the prognosis is good after surgery.
Availability of data and materials
Not applicable.
Abbreviations
- EAC:
-
External auditory canal
- HRCT:
-
High-resolution computed tomography
- OPD:
-
Outpatient department
References
Park SJ, Kim YH (2012) A case of giant osteoma developed from the mastoid cortical bone. Korean J Audiol 16(2):95. https://doi.org/10.7874/kja.2012.16.2.95
Yudoyono F, Sidabutar R, Dahlan RH, Gill AS, Ompusunggu SE, Arifin MZ (2017) Surgical management of giant skull osteomas. Asian J Neurosurg 12(3):408. https://doi.org/10.4103/1793-5482.154873
Abdel Tawab HM, Kumar VR, and Tabook SMS (2015) Osteoma presenting as a painless solitary mastoid swelling. Case Rep Otolaryngol 2015. https://doi.org/10.1155/2015/590783
Borissova IB, Venturin JS, Claro-Woodruff WI, Shintaku WH (2020) Mastoid osteoma: a rare incidental finding in an orthodontic patient. Imaging Sci Dent 50(4):347. https://doi.org/10.5624/isd.2020.50.4.347
Larrea‐Oyarbide N, Valmaseda‐Castellón E, Berini‐Aytés L, and Gay‐Escoda C (2008) Osteomas of the craniofacial region. Review of 106 cases. J Oral Pathol Med 37(1):38–42. https://doi.org/10.1111/j.1600-0714.2007.00590.x
Kandakure VT, Lahane VJ, Mishra S (2019) Osteoma of mastoid bone; a rare presentation: case report. Indian J Otolaryngol Head Neck Surg 71(2):1030–1032. https://doi.org/10.1007/s12070-016-0988-y
Karataş A, Cebi IT, Yanık T, Koçak A, Selçuk T (2017) Osteoma originating from mastoid cortex. Turk Arch Otorhinolaryngol. 55(1):48–50. https://doi.org/10.5152/tao.2017.2128
El Fakiri M, El Bakkouri W, Halimi C, Mansour AA, Ayache D (2011) Mastoid osteoma: report of two cases. Eur Ann Otorhinolaryngol Head Neck Dis 128(5):266–268. https://doi.org/10.1016/j.anorl.2011.03.001
Dhingra R, Davessar JL, Midha N, Singh H, Monga S (2019) Osteoma: a rare case of painless postauricular swelling. Indian J Otolaryngol Head Neck Surg 71(2):1238–1240. https://doi.org/10.1007/s12070-018-1289-4
Lee J, Han K, Kim CH (2020) Rare tumors presenting as a mastoid mass. Case Rep Otolaryngol 2020. https://doi.org/10.1155/2020/8985730
Chen CK, Chang KP, Chien CY, Hsieh LC (2021) Endoscopic transcanal removal of external auditory canal osteomas. Biomedical J 44(4):489–494. https://doi.org/10.1016/j.bj.2020.04.003
Starch-Jensen T (2017) Peripheral solitary osteoma of the zygomatic arch: a case report and literature review. Open Dent J 11:120. https://doi.org/10.2174/1874210601711010120
Ahmadi MS, Ahmadi M, Dehghan A (2014) Osteoid osteoma presenting as a painful solitary skull lesion: a case report. Iran J Otorhinolaryngol 26(75):115
Donati G, Redaelli de Zinis LO (2022) Long-term surgical results of cortical mastoid bone osteomas. Audiol Res 12(3):290–296. https://doi.org/10.3390/audiolres12030030
Remacha J, Navarro-Díaz M, Larrosa F (2022) Experience with three-dimensional exoscope-assisted surgery of giant mastoid process osteoma. J Laryngol Otol 136(9):875–877. https://doi.org/10.1017/S0022215121004588
Marfatia H, Ashwathy K, Madhavi A, Goyal P (2021) Challenges and operative strategy in an unusual case of giant mastoid osteoma. BMJ Case Rep 14(6):e242706. https://doi.org/10.1136/bcr-2021-242706
Guo H, Wang X, Song C, Song Z, Liang J, Song, et al (2018) Trigeminal neuralgia secondary to osteoid osteoma of the petrous bone: report of 4 cases and brief review of literature. World Neurosurg 114: e713-e718. https://doi.org/10.1016/j.wneu.2018.03.065
Benoit C, Chebib E, Bloy O, Elmaleh M, Morcrette G, Van Den Abbeele T (2021) Right incus osteoma in a child: a differential diagnosis of middle ear malformations. J Int Adv Otol 17(6):566. https://doi.org/10.5152/iao.2021.21163
Acknowledgements
Not applicable.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
SSV, acquisition of data and drafted the manuscript. NV, revised the manuscript. PAMP and AS, revised the manuscript and assisted in acquisition of data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
As this is a case report, no ethics committee approval was taken. Consent was taken, and the patient is willing to participate.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Varghese, S.S., Kumar, N., Paul, P.A.M. et al. Osteoma of the temporal bone squama: a case report and review of literature. Egypt J Otolaryngol 39, 129 (2023). https://doi.org/10.1186/s43163-023-00491-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00491-3