Abstract
Objectives
Salvage surgery for hypopharyngeal cancer remains a major challenge, and only a few studies have been conducted. In this study, we review our 10 years of experience in treating patients with hypopharyngeal cancer. The main aim of this study is to analyze survival outcomes in patients who underwent salvage surgery compared with those who had complete remission or inoperable residual tumors.
Methods
Chart reviews were performed for all patients with hypopharyngeal squamous cell carcinoma who underwent curative treatment at a tertiary care hospital between 2009 and 2019. Data on survival, clinical course, and complications were analyzed.
Results
Salvage surgery was performed in 15 of the 34 patients with residual hypopharyngeal cancer. Of these, 10 patients with isolated residual neck disease underwent salvage neck dissection, and five patients with residual primary tumors underwent salvage total or partial laryngopharyngectomy.
The overall 3-year survival rate of patients who underwent salvage surgery was 33.3%. Patients who underwent salvage neck dissection alone had significantly better survival rates than those who received palliative treatment, with median survival times of 21 and 12 months, respectively. The median survival time of patients who underwent laryngopharyngectomy for residual primary tumors was 14 months, which was not significantly different from that of patients who received palliative treatments.
Conclusion
Salvage surgery was associated with improved survival in patients with hypopharyngeal cancer and isolated residual neck disease. Nevertheless, the survival benefit of salvage surgery in patients with residual primary disease remains unclear.
Similar content being viewed by others
Background
Hypopharyngeal cancers are relatively rare, accounting for approximately 3% of all head and neck cancer cases. It is among the cancers with the worst prognosis, with a reported 5-year overall survival rate of approximately 30 − 35% [1]. The prognosis is often worse due to the advanced stage commonly seen at presentation [2]. Moreover, the hypopharynx is rich in submucosal lymphatic network, which promotes the possibility of tumor metastasis [3]. Squamous cell carcinoma is the most common histology identified in 95% of the cases, while adenocarcinoma, sarcoma, and non-epidermoid carcinoma account for the remaining cases [1].
Treatments for hypopharyngeal cancer include surgery, radiotherapy, concomitant chemoradiotherapy, and a combination of these treatments [4, 5]. Patients with hypopharyngeal cancer require complex multimodal management that is best achieved with experienced multidisciplinary teams. Deciding and selecting the appropriate treatment for each patient are essential, as treatments significantly affect important functions as well as patient quality of life [6].
According to the National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology, chemoradiotherapy or surgery is a valid treatment option for resectable hypopharyngeal squamous cell carcinoma [7]. For patients with advanced disease (T4b, N0–3) or those who are unfit for surgery, the selection between curative and palliative aims depends on their performance status [7].
Patients in whom curative treatment fails should be evaluated for salvage surgery. However, salvage surgery for hypopharyngeal cancer often results in difficulty in resection and reconstruction, a high rate of perioperative complications, and poor survival [8]. Three-year survival rates after salvage surgery for hypopharyngeal cancer ranged from 35.8 to 50%, which was relatively low compared with the survival rates after salvage surgery for laryngeal cancer [9,10,11].
Salvage surgery for hypopharyngeal cancer remains a major challenge, and only a few studies have been conducted. In this study, we reviewed our 10 years of experience in treating patients with hypopharyngeal cancer. Outcomes and survival after salvage neck dissection and conservative and radical surgery in patients with residual hypopharyngeal cancer were analyzed and compared with those who had complete remission or inoperable residual tumors.
Methods
This retrospective descriptive study was conducted at a tertiary care hospital in Thailand. Data regarding survival, clinical course, and complications were obtained from patients’ medical records and hospital cancer registrations. The study’s protocol was approved by the hospital ethics committee and waived the requirement for informed consent.
The inclusion criteria were as follows: a new diagnosis of hypopharyngeal squamous cell carcinoma, hospital admission between 2009 and 2019, and receiving curative treatment. The exclusion criteria were as follows: distant metastatic disease at the first diagnosis and premature discontinuation of treatment.
Treatment protocols
In our hospital, patients with stages I–II disease underwent definite radiotherapy. In patients with stages III–IVA disease, primary surgery was the treatment of choice. The selection between organ-preserving radiotherapy and radical surgery depended on the patient’s decision after being fully informed of the risks and benefits. Patients with the operable disease who chose to undergo radiotherapy were categorized as having the organ-preserving disease.
In patients with inoperable tumors, treatment with concomitant chemoradiotherapy was the standard treatment. Induction chemotherapy plus concomitant chemoradiotherapy might be used in selected patients depending on the node status, patient condition, and waiting time for radiotherapy. The patient and the hospital tumor board made the final decision regarding the treatment plan.
The radiotherapy protocol used conventional radiation with a linear accelerator at a dose of 66 − 70 cGy. Concomitant chemotherapy was cisplatin based and administered every week for four to six cycles depending on patient tolerance. The induction chemotherapy regimens in the selected patients were cisplatin/5-fluorouracil, carboplatin/5-fluorouracil, or paclitaxel/carboplatin.
According to the hospital protocol, endoscopic examination and imaging were performed within 3 months of the completion of radiotherapy. Follow-up examinations were performed every 2 − 4 months during the first year. A residual tumor was determined using endoscopic examination and computed tomography (CT)/magnetic resonance imaging (MRI) scan. Patients with persistent or progressive abnormality after 3 months of the completion of radiotherapy were categorized as having residual disease. Punch or fine-needle aspiration biopsies were performed before planning salvage surgery or palliative chemotherapy.
Patients who underwent salvage surgery must have a realistic perspective of the cure. Preoperative metastasis screening included CT or MRI of the neck, chest, and upper abdomen. Positron emission tomography/CT imaging was not performed in this study.
Statistical analysis
Continuous and categorical data were analyzed using the Student’s t-test and chi-squared test, respectively. The survival time was defined as the interval between the date of diagnosis and the date of death. Intervals were measured in months. The Kaplan–Meier method was used to establish the estimated survival outcomes, and differences between the groups were compared using the log-rank test. Differences were considered statistically significant at p < 0.05.
Results
Between 2009 and 2019, 92 of the 248 patients with hypopharyngeal cancer were included in this study. The median follow-up duration was 20.5 months. Figure 1 shows the study flow and outcomes diagram.
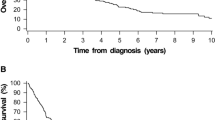
Table 1 shows a comparison of the stages and overall survival outcomes between patients with primary surgery, organ preservation, and inoperable tumors. Figure 2 shows survival curve comparison between these groups. The analysis revealed that patients who underwent primary surgery had better survival rates than those who underwent organ-preserving radiotherapy. However, the difference was not statistically significant (p = 0.055).
Of the 17 patients who underwent organ-preserving radiotherapy and 57 patients who received chemoradiotherapy for inoperable tumors, nine (52.9%) and 25 (43.9%) patients, respectively, had residual disease. Table 2 shows a comparison of the overall survival outcomes of patients after curative radiotherapy. Figure 3 shows survival curve comparison between patients with and without residual tumor. Of the 19 patients with inoperable residual disease, 17 received palliative chemotherapy, and two received supportive care. Figure 4 shows the flow and outcomes diagram between patients undergoing organ-preserving radiotherapy and those with inoperable disease.
Salvage surgery after failed curative radiotherapy
Of the 34 patients with residual disease, 15 underwent salvage surgery, of whom 10 underwent neck dissection alone, and five underwent primary tumor resection with or without neck dissection. All salvage surgeries were performed between 3 and 6 months after completion of the radiotherapy.
Patients who underwent salvage neck dissection alone had significantly better survival than those with inoperable disease. Furthermore, patients who underwent salvage neck dissection alone had survival outcomes comparable to those with complete disease remission.
At our institute, elective neck dissection during salvage surgery is not mandatory for patients without the clinically detectable residual nodal disease. Therapeutic neck dissection includes radical or modified radical neck dissection (type I or II). The major complications after neck dissection were chylous leakage in one patient (7.7%) and wound dehiscence in two patients (15.4%).
Of the five patients with operable residual tumors, three underwent total laryngopharyngectomy, and two underwent partial laryngopharyngectomy. Of these five patients, therapeutic neck dissection was performed in three. Survival analysis showed that the prognosis of patients who underwent surgery for residual primary tumors was poor, and the survival rate was not significantly different from that of patients receiving chemotherapy and supportive care for inoperable residual disease.
In our study, two out of 19 patients with T1–2 tumors had persistent primary tumors after organ-preserving radiotherapy. These patients underwent partial salvage laryngopharyngectomy. Both patients developed severe postoperative salivary fistula. The patients spent over 2 months in the hospital and required intensive wound care. However, local recurrence developed, and both patients died before the restoration of laryngeal and swallowing functions was achieved.
Pectoralis major myocutaneous flap reconstruction was performed in three patients undergoing total laryngopharyngectomy. A pharyngeal fistula developed in two patients. The fistula spontaneously resolved in both patients. Table 3 shows the characteristics and outcomes of the patients who underwent salvage surgery for residual primary tumor.
Of the 15 patients who underwent salvage surgery, 10 survived for < 3 years. Local recurrence was found in 70% of the cases, followed by the development of a second primary cancer (20%) and distant metastasis (10%).
Discussion
Hypopharyngeal cancer has the worst prognosis among head and neck cancers. Improving the survival of patients with hypopharyngeal cancer remains a challenge. Salvage surgery is considered a last-resort treatment for patients with hypopharyngeal cancer who experience radiotherapy failure. The outcomes of salvage surgery for hypopharyngeal cancer are often uncertain in terms of prognosis, survival, and quality of life.
Understanding the prognostic factors is a crucial step in performing salvage surgery. Previous reports demonstrated that factors indicating a poor prognosis after salvage surgery were older age, initial N3, initial stage IV, unresectable at first visit, local and regional concurrent recurrent or residual disease, positive surgical margin, and extranodal spread [11, 12]. However, this topic remains unthoroughly researched in patients with residual hypopharyngeal cancer.
The overall 3-year survival rate of the patients who underwent salvage surgery in this study was 33.3%. Patients with residual neck disease alone had a better prognosis than those with residual primary tumors. The survival of patients who underwent salvage neck dissection was comparable to that of patients who achieved complete remission after radiotherapy. The survival rate of patients who underwent salvage surgery for residual primary tumors was poor and not significantly different from that of those who received palliative treatment.
At our institute, neck dissection was only performed in patients with clinically detectable residual nodal disease. Some studies have suggested that elective neck dissection during salvage surgery may be beneficial in determining prognosis [13, 14]. However, there is no evidence that performing elective neck dissection improves the survival of patients who undergo salvage surgery [15].
The incidence of overall, local, and fistula complications after salvage surgery for hypopharyngeal cancer was higher than that for laryngeal cancer because the treatment of hypopharyngeal cancer usually requires chemotherapy with a higher dose of radiation and flap reconstruction.
Reconstructive modalities after hypopharyngeal resection include anterolateral thigh flap, radial forearm flaps, jejunal flap, gastro-omental flap, and pectoralis flap. The choice of flap depends on individual surgeon’s expertise and preference. A consensus on the flap selection has not been reached [16]. Pharyngocutaneous fistula is the most common early complication after major laryngopharyngeal surgery, ranging from 5 to 65% [17]. Although the fistula complication rate in our study was high, none of the patients experienced catastrophic events, such as carotid artery rupture.
More than 80% of patients with hypopharyngeal cancer initially presented with advanced stage III/IV disease [18]. Radical surgery with salvage total laryngopharyngectomy is commonly performed in patients with persistent disease after radiotherapy to ensure oncological safety. This surgery leads to lifelong changes in communication, airway functions, swallowing, and patient appearance [19].
The principles of cancer management have evolved in the recent past with an emphasis on organ preservation. Organ preservation surgery after radiotherapy failure in patients with early laryngeal cancers has been reported [20]. Although organ preservation surgery, such as partial laryngopharyngectomy, is used as the primary treatment for early-stage hypopharyngeal cancer, no study has reported the outcomes of using conservative surgery as a salvage treatment for residual hypopharyngeal cancer [21].
Partial laryngopharyngectomy may preserve function and improve the quality of life of patients with residual early hypopharyngeal cancer. However, a small number of patients with hypopharyngeal cancer are diagnosed at an early stage, and it is uncommon for these patients with early stages to experience the failure of modern chemoradiotherapy [6, 22].
In the present study, we reported our experience with two patients with residual T1–2 hypopharyngeal cancer who underwent salvage partial laryngopharyngectomy. However, the results were not promising. Restoration of voice and swallowing functions was not achieved, and both patients died from local recurrence within 6 months of the operation.
The main limitations of this study were its retrospective and single-center design, which resulted in a relatively small number of patients. The patient’s decision to choose between salvage surgery or palliative chemotherapy is affected by several factors and does not depend solely on the operability status. Several factors concerning patients, underlying health status, and tumor characteristics and location could not be controlled.
Conclusion
Salvage surgery significantly improved the survival of patients with hypopharyngeal cancer and isolated residual neck disease. Survival was poor among patients who underwent salvage surgery for residual primary tumors, and none of them survived for > 3 years postoperatively. Although the median survival time of patients in this group was slightly longer than that of patients receiving palliative treatment, the survival benefit of salvage surgery in patients with residual primary disease remains unclear. Addressing this question requires further research using larger sample sizes.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Garneau JC, Bakst RL, Miles BA (2018) Hypopharyngeal cancer: a state of the art review. Oral Oncol 86:244–250. https://doi.org/10.1016/j.oraloncology.2018.09.025
Bradley PJ (2019) Epidemiology of hypopharyngeal cancer. Adv Otorhinolaryngol 83:1–14. https://doi.org/10.1159/000492299
Zhang X, Zhang Y, Yu X et al (2021) Different primary sites of hypopharyngeal cancer have different lymph node metastasis patterns: a retrospective analysis from multi-center data. Front Oncol 11:727991. https://doi.org/10.3389/fonc.2021.727991
Panda S, Sakthivel P, Gurusamy KS et al (2022) Treatment options for resectable hypopharyngeal squamous cell carcinoma: a systematic review and meta-analysis of randomized controlled trials. PLOS One 17:e0277460. https://doi.org/10.1371/journal.pone.0277460
Pointreau Y, Biau J, Delaby N, Thariat J, Lapeyre M (2022) Radiotherapy for hypopharynx cancers. Cancer Radiother 26:199–205. https://doi.org/10.1016/j.canrad.2021.10.006
Bozec A, Poissonnet G, Dassonville O, Culié D (2023) Current therapeutic strategies for patients with hypopharyngeal carcinoma: oncologic and functional outcomes. J Clin Med 12:1237. https://doi.org/10.3390/jcm12031237
NCCN Clinical Practice Guidelines in oncology: head and neck cancers, version 1.2023. (2022). Accessed 9 Feb 2023: https://www.nccn.org.
Zhang Y, Huang Z, Xu M et al (2022) Complications and oncological outcomes after salvage surgery for recurrent and residual hypopharyngeal squamous cell carcinoma: a retrospective cohort study. Ann Transl Med 10:525. https://doi.org/10.21037/atm-22-1844
Huang Q, Wu ZH, Zhou L, You Q (2022) Survival outcomes and prognostic factors of patients with salvage surgery for hypopharyngeal carcinoma after radiotherapy. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 57:191–196. https://doi.org/10.3760/cma.j.cn115330-20210318-00136
Dubsky PC, Stift A, Rath T, Kornfehl J (2007) Salvage surgery for recurrent carcinoma of the hypopharynx and reconstruction using jejunal free tissue transfer and pectoralis major muscle pedicled flap. Arch Otolaryngol Head Neck Surg 133:551–555. https://doi.org/10.1001/archotol.133.6.551
Maruo T, Zenda S, Shinozaki T et al (2020) Comparison of salvage surgery for recurrent or residual head and neck squamous cell carcinoma. Jpn J Clin Oncol 50:288–295. https://doi.org/10.1093/jjco/hyz176
Bulbul MG, Genovese TJ, Hagan K, Rege S, Qureshi A, Varvares MA (2022) Salvage surgery for recurrent squamous cell carcinoma of the head and neck: systematic review and meta-analysis. Head Neck 44:275–285. https://doi.org/10.1002/hed.26898
Lin C, Puram SV, Bulbul MG et al (2019) Elective neck dissection for salvage laryngectomy: a systematic review and meta-analysis. Oral Oncol 96:97–104. https://doi.org/10.1016/j.oraloncology.2019.07.008
Anwar M, Dewidar H, Hareedy A et al (2022) Role of elective neck dissection with salvage laryngectomy. Egypt J Otolaryngol 38:55. https://doi.org/10.1186/s43163-022-00249-3
Gross JH, Vila PM, Simon L et al (2020) Elective neck dissection during salvage laryngectomy: a systematic review and meta-analysis. Laryngoscope 130:899–906. https://doi.org/10.1002/lary.28323
Chen WF, Chang KP, Chen CH, Shyu VB, Kao HK (2013) Outcomes of anterolateral thigh flap reconstruction for salvage laryngopharyngectomy for hypopharyngeal cancer after concurrent chemoradiotherapy. PLOS One 8:e53985. https://doi.org/10.1371/journal.pone.0053985
Chu PY, Chang SY (2005) Reconstruction after resection of hypopharyngeal carcinoma: comparison of the postoperative complications and oncologic result of different methods. Head Neck 27:901–908. https://doi.org/10.1002/hed.20262
Liang Z, Wu M, Wang P et al (2023) Updated racial disparities in incidence, clinicopathological features and prognosis of hypopharyngeal squamous carcinoma in the United States. PLOS One 18:e0282603. https://doi.org/10.1371/journal.pone.0282603
Chotipanich A (2021) Total laryngectomy: a review of surgical techniques. Cureus 13:e18181. https://doi.org/10.7759/cureus.18181
Chen MM, Holsinger FC, Laccourreye O (2015) Salvage conservation laryngeal surgery after radiation therapy failure. Otolaryngol Clin North Am 48:667–675. https://doi.org/10.1016/j.otc.2015.04.011
Y-ling K, Chang C-F, Chang S-Y, Chu P-Y (2012) Partial laryngopharyngectomy in the treatment of squamous cell carcinoma of hypopharynx: analysis of the oncologic results and laryngeal preservation rate. Acta Otolaryngol 132:1342–1346. https://doi.org/10.3109/00016489.2012.700122
Li WX, Dong YB, Lu C, Bradley PJ, Liu LF (2022) Efficacy of larynx preservation surgery and multimodal adjuvant therapy for hypopharyngeal cancer: a case series study. Ear Nose Throat J 1455613221098784. https://doi.org/10.1177/01455613221098784
Acknowledgements
The author would like to thank the operating room staff at Chonburi Cancer Hospital for support in data collection.
Funding
None.
Author information
Authors and Affiliations
Contributions
AC was responsible for the conception of the study, acquisition, analysis of data, drafting, and revising.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study’s protocol was approved by the Chonburi Cancer Hospital ethics committee (approval number: 008/66, 15 Feb. 2023). The Chonburi Cancer Hospital ethics committee exempted the consent from participants as data was collected retrospectively from charts, and human subjects were not directly involved in the study.
Consent for publication
Written informed consent for publication of the patients, whose personally identifiable information is provided, was obtained from their next of kin.
Competing interests
The author declares no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chotipanich, A. Survival outcome of patients undergoing salvage surgery for hypopharyngeal cancer after failure of primary curative treatment: a retrospective study. Egypt J Otolaryngol 39, 119 (2023). https://doi.org/10.1186/s43163-023-00479-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00479-z