Abstract
Background
Sporotrichosis is a subcutaneous mycosis caused by a dimorphic fungus, Sporothrix schenckii infection, that usually results from the traumatic implantation of the fungus into the skin and subcutaneous tissue. Disseminated cutaneous sporotrichosis is a rare entity that usually presents in the immunosuppressed individual. They are sometimes mimicking malignancy and tuberculosis. Here, a rare case of disseminated cutaneous sporotrichosis involving the larynx and nasal cavity in an immunocompetent patient is reported.
Case presentation
A 54-year-old healthy lady presented with hoarseness and globus sensation over the throat with prior history of multiple skin lesions over the face, limbs, and trunk. Examination revealed erythematous papular lesions over the face, limbs, and trunk. Nasoendoscopy showed sloughy mucosa over bilateral nasal cavities, nasopharynx, base of the tongue, arytenoids, and both vocal folds with bony hard mass at the left frontal recess opening. Overall imaging features were suggestive of generalized fungal infections. Multiple biopsies from multiple sites revealed Sporothrix schenckii infection. She had resolution of the lesion after being treated with intravenous Amphotericin B for a month, oral Voriconazole for another month then oral Itraconazole for 6 months.
Conclusion
Diagnosis of disseminated sporotrichosis can be tricky and difficult to diagnose as it can mimic other diagnoses. Education is paramount important in identifying the illness as it can be seen in immunocompetent individuals, although it is more common in the immunosuppressed individual.
Similar content being viewed by others
Background
Sporotrichosis caused by Sporothrix schenckii is a relatively rare infection seen mainly in farmers, gardeners, and carpenters. Direct inoculation of the organism from either a contaminated thorn or a splinter through the skin can cause the infection [1]. However, it is mostly acquired by humans when a traumatic inoculation occurs after contact with animals such as cats, dogs, and horses [2].
It is characterized by the subacute and chronic evolution of cutaneous or subcutaneous nodular lesions. Sporotrichosis is usually encountered as a localized infection of the hand, but the disseminated disease is rarely seen [1]. Systemic disseminated sporotrichosis is considered a severe opportunistic infection which is usually reported in immunosuppressed patients. The diagnosis of this disease can sometimes be difficult as they are sometimes mimicking malignancy and tuberculosis. The culture of Sporothrix schenckii is the gold standard diagnostic test [3]. Thus, the aim of this study is to highlight the illness as it can be seen in immunocompetent individuals, although it is more common in the immunosuppressed individual.
Case presentation
A 54-year-old healthy lady presented with hoarseness and globus sensation over the throat for a month with initial 3 months history of multiple skin lesions over the face, limbs, and trunk. The lesions initially started as a small nodule then progressively worsened and ulcerated. No history of fever, nasal symptoms, or shortness of breath and no significant family or malignancy history. She had a history of a cat scratch previously. Examination revealed erythematous papular lesions over the face, limbs, and trunk measuring 5 × 5 cm, rounded in size with minimal contact bleeding (Fig. 1). Nasoendoscopy showed sloughy mucosa over the left inferior and middle turbinate, right inferior turbinate, nasopharynx, base of the tongue, arytenoids, and both vocal fold with bony hard mass at left frontal recess opening on probing with ballprobe (Figs. 2, 3, and 4). Bilateral inguinal lymph nodes were palpable, but other examinations were unremarkable.
Computed tomography (CT) scan of the brain, thorax, abdomen, and pelvis showed lesions over ethmoidal, left frontal sinusitis, nasal cavity lesions, left vallecula, and posterior pharyngeal wall with the presence of subcutaneous abscesses over the right frontal scalp and right cheek. There was also hepatosplenomegaly with liver lesions that may represent cysts or micro-abscesses. Overall imaging features were suggestive of generalized fungal infections.
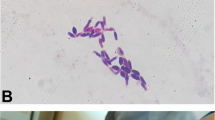
Biopsy of skin lesion, nasal cavities mass, left inferior turbinate, left frontal recess mass, nasopharynx, and bilateral inguinal lymph node suggestive of fungal infection which is morphologically consistent with Cryptococcus species. The specimen was sent to the Institute of Medical Research (IMR), and the final result was revealed as Sporothrix schenckii infection (Fig. 5).
The patient was treated with intravenous Amphotericin B for a month, then oral Voriconazole 200 mg twice daily for another month subsequently continued with oral Itraconazole for 6 months. She was asymptomatic upon the last clinic follow-up after 1 year of completed treatment and given 6 monthly outpatient visit appointments.
Discussion
Sporotrichosis was first described by Benjamin Schenck in 1898 as a chronic cutaneous and subcutaneous infection caused by the dimorphic fungus Sporothrix schenckii [4, 5]. S. schenckii is a common saprophyte found in the soil, straw, wheat grain, fruits, tree bark, wood, shrubs, thorns, rose shrubs, decaying vegetation, and timber [2]. Animals like cats, rodents, birds, and armadillos have been known to spread the infection [6]. Traumatic inoculation of the pathogenic fungus into the skin causing an infection, but pulmonary infection can occur following inhalation of spores [7].
Studies showed that sporotrichosis infection affects all age groups and both genders [5]. Male preponderance was reported in some studies which was possibly related to occupational environmental exposure to a contaminated source [8, 9] but in contrast to other studies from India [10] and Japan [11], reported that women were more frequently affected due to their active participation in outdoor activities such as gardening, agricultural work, and other outdoor activities [5]. However, a study by Tang et al. done in Malaysia shows that the gender ratio was comparable as the risk is associated with participation in daily activities that predispose to the infection [5]. Most of the cases infected by traumatic inoculation of S. schenckii were related to cat scratches or bites by the fact that in Malaysia, and cats are the most popular domestic pets [5]. Our patient also revealed a similar history of cat scratches before the presentation.
Sporotrichosis is classified into four clinical categories: (i) lymphocutaneous, (ii) fixed cutaneous, (iii) multifocal or disseminated, and (iv) extra-cutaneous. Lymphocutaneous sporotrichosis is the most common entity while disseminated cutaneous sporotrichosis is an uncommon entity. It is usually present only in the immunosuppressed patient including HIV infection, malignancies, organ transplantation, alcoholism, diabetes mellitus, sarcoidosis, tuberculosis, the use of immunosuppressive agents, and the administration of tumor necrosis factor-alpha antagonists [3]. It occurs very rarely in immunocompetent patients [12]. In the current case, it is postulated that the patient’s advanced age allowed for the dissemination and spread of the cutaneous lesions.
Disseminated sporotrichosis can be a difficult disease to diagnose and treat. We have encountered a difficulty to establish the diagnosis as the case of sporotrichosis in our center is rare and the presentation mimics malignancy and tuberculosis. In the head and neck region, sporotrichosis in the facial skin is most often seen [13]. However, only a few cases of laryngeal sporotrichosis have been reported. Khabie et al. reported a case of stridor in a young child caused by sporotrichosis of the larynx and had completed the resolution of her symptoms after being treated with a systemic antifungal [13]. Another case was reported in a woman who worked in a sphagnum moss plant and developed long-standing hoarseness due to the infection of the vocal cord. She was successfully treated with potassium iodide [13].
Disseminated cutaneous sporotrichosis can be acquired from various modes of transmission like skin inoculation or inhalation of the fungus which subsequently spreads to the lymphatics and bloodstream [12]. In the current case, she might acquire the infection through the cat scratches and disseminated disease was suspected since the patient had involvement in multiple sites such as the face, limb, trunk, larynx, and nasal cavity.
Definitive diagnosis is made by the demonstration of fungal spores, hyphae, or pseudohyphae either by tissue biopsy or fungal potassium hydroxide (KOH) smear and culture. Incubation is performed at 25 °C with Sabouraud dextrose agar, producing creamy-white colonies within 5 days, which later turn into the characteristic black-brown colonies [14]. The conversion of mold to yeast in vitro confirms the diagnosis [14]. Similar findings were found in our patient.
Prompt treatment and appropriate measures will prevent morbidity. It is treated by antifungal drugs and the elimination of risk factors. Initial treatment of disseminated sporotrichosis consists of intravenous Amphotericin B, followed by oral Itraconazole. While other alternative treatment would be oral Terbinafine, saturated solution of potassium iodide (SSKI), oral fluconazole, or thermal treatment [12]. A study by Tang et al. showed localized subtypes of sporotrichosis was successfully treated with oral itraconazole (68.3%) for a mean duration of 15.6 weeks while the patient with disseminated cutaneous sporotrichosis was treated with intravenous amphotericin B [5]. Our patient was treated with intravenous Amphotericin B for a month, then oral Voriconazole 200 mg twice daily for another month, and subsequently with oral Itraconazole for 6 months. She had clinical improvement after starting these types of medications and had no serious adverse effects of the medications.
Conclusion
Sporotrichosis is a fungal infection that may lead to systemic organ involvement if left untreated. This case highlighted to us that disseminated cutaneous sporotrichosis can be seen in immunocompetent individuals, although it is more common in the immunosuppressed individual. Fungal culture should be added as an essential investigation in patients with similar presentations. Combine treatment of oral antifungal and intravenous amphotericin B shown a successful outcome in disseminated cutaneous sporotrichosis.
Availability of data and materials
Not applicable.
References
Hassan K, Turker T, Zangeneh T (2016) Disseminated sporotrichosis in an immunocompetent patient. Case Reports Plast Surg Hand Surg 3:44. https://doi.org/10.3109/23320885.2016.1168703
Pediatric sporotrichosis: background, pathophysiology, epidemiology. Accessed: 5 Dec 2022. https://emedicine.staging.medscape.com/article/968902-overview
Mahajan VK (2014): Sporotrichosis: an overview and therapeutic options. Dermatol Res Pract 2014:272376. https://doi.org/10.1155/2014/272376
Bustamante B, Campos PE (2001) Endemic sporotrichosis. Curr Opin Infect Dis 14:145–149. https://doi.org/10.1097/00001432-200104000-00006
Tang MM, Tang JJ, Gill P, Chang CC, Baba R (2012) Cutaneous sporotrichosis: a six-year review of 19 cases in a tertiary referral center in Malaysia. Int J Dermatol 51:702–708. https://doi.org/10.1111/J.1365-4632.2011.05229.X
Reed KD, Moore FM, Geiger GE, Stemper ME (1993) Zoonotic transmission of sporotrichosis: case report and review. Clin Infect Dis 16:384–387. https://doi.org/10.1093/CLIND/16.3.384
Hardman S, Stephenson I, Jenkins DR, Wiselka MJ, Johnson EM: Disseminated Sporothix schenckii in a patient with AIDS. J Infect. 2005, 51:. https://doi.org/10.1016/J.JINF.2004.07.001
Conias S, Wilson P (1998) Epidemic cutaneous sporotrichosis: report of 16 cases in Queensland due to mouldy hay. Australas J Dermatol 39:34–37. https://doi.org/10.1111/J.1440-0960.1998.TB01239.X
Mohan N, Jayaseelan E, Abraham A, Rajendran SC, Stephen J, Sharief S, Macaden R (2004) Cutaneous sporotrichosis in Bangalore, southern India. Int J Dermatol 43:269–272. https://doi.org/10.1111/J.1365-4632.2004.01661.X
Agarwal S, Gopal K (2008) Umesh, Kumar B: Sporotrichosis in Uttarakhand (India): a report of nine cases. Int J Dermatol 47:367–371. https://doi.org/10.1111/J.1365-4632.2008.03538.X
Itoh M, Okamoto S, Kariya H (1986) Survey of 200 cases of sporotrichosis. Dermatology 172:209–213. https://doi.org/10.1159/000249337
Bin YFB (2011) Disseminated cutaneous sporotrichosis in an immunocompetent individual. Int J Infect Dis 15:e727–e729. https://doi.org/10.1016/J.IJID.2011.05.005
Khabie N, Boyce TG, Roberts GD, Thompson DM (2003) Laryngeal sporotrichosis causing stridor in a young child. Int J Pediatr Otorhinolaryngol 67:819–823. https://doi.org/10.1016/S0165-5876(03)00089-2
Ramos-e-Silva M, Vasconcelos C, Carneiro S, Cestari T (2007) Sporotrichosis. Clin Dermatol 25:181–187. https://doi.org/10.1016/J.CLINDERMATOL.2006.05.006
Acknowledgements
We would like to thank Director-General of Health Malaysia for his permission to publish this article.
Funding
This manuscript has not received any external or industrial support or funding.
Author information
Authors and Affiliations
Contributions
NR was involved in the collection of the data, literature search, writing the original draft, surgical assistance, patient follow-up, and the corresponding author. KB, MAA, and ISS were involved in the patient management, operating surgeon, follow-up, and review of the draft. HS was involved in reviewing the final draft. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for publication of the case report was obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roslle, N., Noh, K.B., Ahmad, M.A. et al. Nasal and laryngeal sporotrichosis in an immunocompetent individual: a case report. Egypt J Otolaryngol 39, 59 (2023). https://doi.org/10.1186/s43163-023-00424-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00424-0