Abstract
Background
Hemangioendothelioma is a rare vascular tumor of the head and neck region characterized by proliferation of endothelial cells with epithelioid morphology. This is an indolent tumor known to appear during adult life, with potential for recurrence, but unlikely to metastasize. Although reports of endotheliomas affecting soft tissues, skin, viscera, bone, or lymph nodes have been reported, very few cases of hemangioendothelioma of nasal cavity have come to light, that too in adults only.
Case presentation
Authors here-in present an unusual case of hemangioendothelioma of nasal cavity in a 9-year-old girl with a 6-month history of intermittent epistaxis and nasal obstruction. The tumor was excised endoscopically under general anesthesia and histopathology confirmed the diagnosis.
Conclusions
Wide excision is the treatment of choice. Regular follow-up is advised as potential for recurrence is high.
Similar content being viewed by others
Background
Hemangioendothelioma was first described by Weiss and Zenger in 1982 as a unique vascular tumor of the soft tissue with an indolent clinical course and characterized by presence of ‘epithelioid’ endothelial cells [1]. The clinical course and histologic characteristics of this tumor are intermediate between a hemangioma and a conventional angiosarcoma; hence, the term epithelioid hemangioendothelioma was proposed [1].
The appearance of this tumor in the nasal cavity has been reported in adult patients and none in pediatric age group so far. Occurrence of this tumor in the superficial and deep soft tissues, liver, lung, bone, brain, heart, and lymph nodes have been reported with infrequent involvement of head and neck region [2]. Reports of appearance of this tumor in nasal cavity are scarce.
Histologically, this vascular neoplasm contains endothelial cells with characteristic epithelioid morphology arranged in short cords or strands with majority showing vacuolated eosinophilic cytoplasm [3]. The cells show minimal to modest atypia with few mitotic figures [4, 5].
The management of this tumor entails wide surgical excision of the mass with regular clinical follow-up due to the potential for recurrence [6].
Case presentation
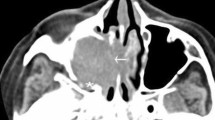
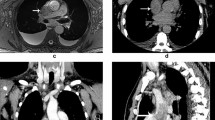
A 9-year-old girl presented with a history of blockage of left nasal cavity with infrequent episodes of left-sided nasal bleeding of small amounts for 6 months associated with a slow growing, painless and firm swelling of cheek with broadening of left nasal bridge (Figs. 1 and 2). No history of pain in nose or over cheek, headache, nasal discharge or trauma were noted. Vision was not affected. Patient had no significant medical history. General examination was within normal limits. There was no lymphadenopathy. On anterior rhinoscopy, a reddish-grey lobular mass covered with slough was seen filling the left nasal cavity, which bled to touch. Posterior rhinoscopy showed blockage of left choana due to the mass. Oral cavity and oropharyngeal examinations were normal. Routine blood investigations including complete hemogram, serum electrolytes and coagulation profile were done. All were within normal limits except hemoglobin which was around 10 gm/dl characterizing mild anemia. Computed tomography of the nose and paranasal sinuses showed a large expansile heterogeneously enhanced mass lesion filling the left nasal cavity up to the choana, thought to originate from the lateral wall and pushing the septum to the right, with no intra-orbital or intracranial extension (Fig. 3A–C). Patient was planned for endoscopic excision under general anesthesia. Using 0° wide-angled telescope tumor was visualized and its extensions and attachments were identified. The tumor seemed to be arising from the left middle turbinate and adjoining areas pushing the septum towards right side without any evidence of destruction of nasal septum. The tumor was excised completely from its attachments using straight and angled Blakesley nasal forceps. The tumor excision was followed by brisk hemorrhage which was controlled using nasal packs. After achievement of hemostasis, the nasal cavity was inspected for any residual tumor. Following complete excision of tumor, nasal cavity was packed using merocele, which was removed after 24 h. Due to profuse bleeding intra-operatively, one unit of packed blood was transfused. Tissue was sent for histopathology. Grossly, the excised mass was globular and greyish white in appearance. Microscopic examination showed tumor tissue lined by pseudostratified ciliated columnar epithelium and composed of anastomosing channels of capillary sized vessels lined by endothelial cells with abundant vacuolated cytoplasm; in some cells, cytoplasm was eosinophilic as well (Fig. 4). The nuclei were round, vesicular and indentations were also seen in some. Pleomorphism, mitosis, and necrosis were not prominent. The stroma was scanty with lymphomononuclear inflammation in some areas. This histomorphology was consistent with hemangioendothelioma. Patient was called for regular follow-ups after every 2 weeks for first 3 months. On follow-up, nasal endoscopy did not reveal any lesion. Repeat computed tomography was done after 3 months post-operatively, which showed complete resolution of the lesion (Fig. 5A, B). Patient has been asymptomatic since then and is being followed-up on a regular basis every 3 months. So far, no recurrence has been observed.
Section shows lining pseudostratified ciliated columnar epithelium displaying squamous metaplasia with a lobular tumor in submucosal area in (A H&E × 40). Tumor composed of anastomosing channels of capillary sized vessels lined by endothelial cells with abundant vacuolated cytoplasm, the stroma is scanty with lymphomononuclear inflammation in some areas. (B H&E × 100); The nucleus is round, vesicular and indentations are also seen in some nuclei highlighted by an arrow (C H&E × 400)
Discussion
Hemangioendothelioma is quiet an uncommon tumor of the head and neck region and more-so of the nasal cavity, given by the fact that only sporadic cases have been reported in literature till date. Cases involving the submandibular and parotid gland, parapharyngeal space, maxilla and maxillary sinus, larynx and thyroid have been reported [7].
Weiss et al. [1] have described the appearance of this tumor during adult life, with no predilection for skin and superficial soft tissues and lack of large well-formed vascular channels on microscopic examination. Here, we have reported the case in a pediatric patient which has not been described in literature so far.
This is a low-grade neoplasm with equal predilection in both sexes [6]. Etiology is not yet completely understood, nor predisposing factors rightly identified. Trauma, radiation and hormonal factors have shown some association [1].
Among the vascular tumors of nasal cavity, lobular hemangioma, angiosarcoma, pyogenic granuloma, nasopharyngeal angiofibroma, angiomyoma, hamartoma, sinonasal hemangiopericytoma, or arteriovenous malformations can be considered in the differential diagnoses [6, 8]. The tumor can be differentiated from nasopharyngeal angiofibroma on the basis of age and gender of our patient, infrequent episodes of nasal bleed in small amounts, and lack of involvement of nasopharynx. Definitive diagnosis has to be made on the basis of histopathology and immunohistochemistry.
Histology of these neoplasms predominantly shows endothelial cells of epithelioid morphology with eosinophilic cytoplasm and intracellular vascular lumina producing cytoplasmic vacuolations [8]. The tumor can be differentiated from a carcinoma on the basis of lack of necrosis, nuclear pleomorphism and atypia with occasional mitosis [8]. Our reported case showed capillary sized vessels lined by endothelial cells with abundant vacuolated cytoplasm and scanty stroma. Pleomorphism, mitosis, and necrosis were not evident.
While prognosis of hemangioendothelioma in the head and neck region is not established yet, factors such as multiple recurrences or metastasis and high cellular atypia with increased mitotic activity and presence of necrosis on histology generally indicate a poor prognosis [6].
Surgery should always include a wide excision of the mass with negative margins. Incompletely or inadequately excised tumors exhibiting multiple recurrences, or tumors with regional lymph node metastasis can be treated additionally with chemotherapy or radiation therapy [8,9,10]. In our case, we did not plan for any add-on therapy because the surgical margins were free of tumor following excision, and moreover the patient belonged to pediatric age group. This tumor entails long-term follow-up due to its propensity for recurrence [2].
Conclusion
Hemangioendothelioma being a rare vascular tumor is not usually considered in the differential diagnosis of mass nasal cavity in regular clinical practice especially in pediatric population. The presentation tends to be more favorable towards a lobular hemangioma or an angiosarcoma. Only histology with/without immunohistochemistry can save the diagnosis, aided by clinical examination and imaging. Familiarity with its characteristic histologic pattern will lead to a more accurate diagnosis and hence greater incidence of reporting of cases.
Availability of data and materials
NA.
References
Weiss SW, Enzinger FM (1982) Epithelioid hemangioendothelioma a vascular tumor often mistaken for a carcinoma. Cancer 50(5):970–981
Tseng C-C, Tsay S-H, Tsai T-L, Shu C-H (2005) Epithelioid hemangioendothelioma of the nasal cavity. J Chin Med Assoc 68(1):45–48
Flucke U, Vogels RJC, de Saint AubainSomerhausen N, Creytens DH, Riedl RG, van Gorp JM et al (2014) Epithelioid hemangioendothelioma: Clinicopathologic, immunhistochemical, and molecular genetic analysis of 39 cases. Diagn Pathol 9(1):1
Billings SD, Folpe AL, Weiss SW (2003) Epithelioid sarcoma-like Hemangioendothelioma. Am J Surg Pathol 27(1):48–57
Girolamo AD, Giacomini PG, Coli A, Castri F, de Padova A, Bigotti G (2003) Epithelioid haemangioendothelioma arising in the nasal cavity. J Laryngol Otol 117(1):75–77
Hanege FM, Uzun L, Yavuz C, Ozkanli S, Kurtgoz S (2016) Epithelioid hemangioendothelioma of the nasal septum. B-ENT 12(2):155–157
Robinson AA, Tolentino LF, Uyanne J, Melrose R, Calhoun CC (2014) Malignant epithelioid hemangioendothelioma of the lip: a case report and comprehensive literature review. J Oral Maxillofac Surg 72(4):695–701
Patnayak R, Jena A, Reddy MK, Chowhan Akumar, Rao LMC, Rukhamangadha N (2010) Epithelioid hemangioendothelioma of nasal cavity. J Lab Phys 2(02):111–3
Naqvi J, Ordonez NG, Luna MA, Williams MD, Weber RS, El-Naggar AK (2007) Epithelioid hemangioendothelioma of the head and neck: Role of Podoplanin in the differential diagnosis. Head Neck Pathol 2(1):25–30
Parajón A, Vaquero J (2008) Meningel intracranial epithelioid hemangioendothelioma: Case report and literature review. J Neurooncol 88(2):169–173
Acknowledgements
None.
Funding
NA.
Author information
Authors and Affiliations
Contributions
MP have assisted in the surgery and written the first draft of manuscript. HP is the lead surgeon and prepared the final draft of the manuscript in consultation of PA, who also did the HPE examination of the excised specimen. JS assisted PA in HPE examination of specimen and during finalization of manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Obtained from Institutional ethics committee, King George’s Medical University. Reference no.- not applicable.
Consent for publication
Written informed consent obtained from parents.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Patnaik, M., Singh, H.P., Agarwal, P. et al. Hemangioendothelioma of the nasal cavity: a rare case report and review of literature. Egypt J Otolaryngol 39, 56 (2023). https://doi.org/10.1186/s43163-023-00422-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-023-00422-2