Abstract
Background
Head injury most commonly occur following road traffic accidents. Often hearing loss and other otological injuries are missed in view of serious head injury or other visible bodily injuries, leading to delayed recognition of problems. There is a need for early clinical and radiological indicators which can predict adverse outcome. Early diagnosis of otological injury during initial evaluation of the head injury has given some clues regarding the severity of hearing outcomes and such correlation has been attempted in this study. Two-year cross-sectional study involving head injury patients with radiological evidence of temporal bone fracture were assessed for hearing impairment.
Results
Thirty-seven patients who satisfied the inclusion criteria were assessed. Fifty-one percent patients had conductive hearing loss. 35.14% of the patients had involvement of mastoid, external auditory canal, and middle ear involvement. A weakly positive correlation was noted between otic capsule sparing fracture and hearing loss. (R value + 0.2064).
Conclusion
Weak correlation was observed between temporal bone sub-site classification and severity of hearing loss in otic capsule sparing temporal bone fractures.
Similar content being viewed by others
Background
Road traffic accidents are the leading cause of head injury [1]. Otological injuries are often missed in view of complex presentation of head injury and other visible bodily injuries. Altered state of consciousness further worsens clinical evaluation of these patients. Otological injuries vary from simple injury to the pinna to complex fractures of the temporal bone. Blood clots in the external auditory canal, impinged fracture segments of the bony canal wall, stenotic external auditory canal, rupture of the tympanic membrane, ossicular disruption, middle ear hematoma leads to conductive hearing loss. Disruption of round window, CSF leak, cochlear disruption, and loss of vascularity to the cochlea leads to sensory neural hearing loss [2].
Identification of hearing loss in the emergency setting is challenging. Though signs of temporal bone fracture can be clinically made out by visible signs such as haemotympanum, Battle sign and Raccoon sign [3] exact extent and severity can be assessed only by radiological means. Radiological evaluation plays a key role in evaluating these patients with head injury as it provides valuable inputs into the altered neurological status. This evaluation tool can be made use of in identifying, the nature and extent of involvement of temporal bone fractures. As direct evaluation of hearing is not possible in emergency/casualty settings, radiological findings can be taken into consideration while predicting the severity of hearing impairment.
Traditionally for descriptive purposes, temporal bone fractures were classified into longitudinal, transverse, and mixed based on the alignment of fracture line in relation to long axis of the temporal bone and is of anatomical significance. Attempt to classify temporal bone fractures for prognostic purposes was made by Ishman [4] based on petrous apex involvement. Facial nerve injury, cerebrospinal fluid (CSF) leak, and sensorineural hearing loss (SNHL) were commonly seen in patients with petrous apex involvement. A newer classification system utilizes otic capsule involvement as predictor of sensory neural hearing loss. But this classification system fails to predict the severity of conductive hearing loss in otic capsule sparing temporal bone fractures [5]. So Young Kim et al. studied various audiometric patterns in otic capsule sparing fractures and proposed a sub-site classification system to predict the severity of the hearing loss [6]. In this study, an attempt is being made to correlate the severity of the hearing loss in otic capsule sparing fracture patients based on the sub-site classification system.
Methods
A cross-sectional study was conducted between October 2018 and September 2020 in a tertiary care center, after obtaining institutional ethical committee clearance. Head injury patients with otological symptoms attending the emergency department were screened. Patients with radiographically (computed tomography CT) proven otic capsule sparing temporal bone fracture who were able to participate in audiological evaluation (8 h to 4 days of injury) were enrolled for the study. Patients with poor Glasgow Coma Scale score (GCS), less than 6 years old, pre-existing ear diseases and documented history of hearing loss prior to this event, were excluded from the study. Patients with Otic capsule sparing temporal bone fractures were subdivided into groups in increasing number of sub-site involvement based on sub-site classification. (M—mastoid, EAC—external auditory canal, ME—middle ear, O—ossicular chain disruption) group I: isolated mastoid fractures, group II: isolated EAC involvement, group III: mastoid and EAC involvement, group IV: mastoid and middle ear involvement, group V: mastoid, EAC, and middle ear involvement, group VI: mastoid, middle ear, and ossicular involvement, and group VII: mastoid, middle ear, EAC, and ossicular involvement. Only pure tone audiometry (PTA) was carried out using MAICO MA 42 Audiometer.
Numerical data was expressed in percentage and frequency. Comparative analysis of hearing loss in various groups was made. Pearson ‘R’ correlation test was used to test the correlation between sub-site involvement and severity of hearing loss.
Results
A total of 37 ears (32 patients with 5 bilateral involvement) meeting inclusion and exclusion criteria were included in the study. Study group included age ranging from 8 years to 62 years with mean of 36.54 years. Majority of the patients were aged between 20 and 40 years (19 Patients 51.35%) (Fig. 1). Left-sided ear was affected in 14 patients (43.75%) and right-sided ear was affected in 13 patients (40.63%) and 5 patients (15.63%) had bilateral affliction Table 1.
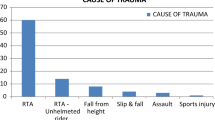
Male to female ratio was 5.2:1. Thirty-one males constituted 83.78% and 6 females (16%) constituted the study group. Figure 1 shows road traffic accident (RTA) was the most common mode of injury (Fig. 2). Three patients had facial palsy; among which 2 had grade 4 and 1 had grade 2 facial function according to House-Brackmann Classification system. Two patients had diabetes and one had epilepsy.
As per sub-site classification, group VI: mastoid, middle ear, and ossicular involvement, and group VII: mastoid, middle ear, EAC, and ossicular involvement, was not seen in any of the patient in the study population (Table 2).
Thirteen patients had type 5, i.e., mastoid, EAC, and middle ear involvement and were the most common with a mean loss of 34.26dB on PTA (Fig. 4). Isolated mastoid bone fracture was noted in 5 patients with mean PTA loss of 30.04 dB, 2 patients had isolated EAC fractures with mean PTA loss of 25.80 dB, 9 patients had mastoid with EAC involvement with mean PTA loss of 29.64 dB and 8 patients had mastoid with middle ear involvement with mean PTA hearing loss of 48.44 dB (Fig. 3)
Pearson correlation coefficient (Fig. 5) was calculated to establish any correlation between grading of otic capsule sparing temporal bone fractures and degree of hearing loss. The value of R was 0.2064, and P value was 0.220 which was not statistically significant at P < 0.05.
Discussion
Temporal bone fractures constitute a significant proportion of basilar skull fractures which in turn are the commonest skull fractures following head injury. The temporal bone, a morphologically complex bone, consists of five fused elements: the styloid process, tympanic ring, squamous, mastoid, and petrous bones [7]. The original classification system for temporal bone fractures describes the fracture orientation relative to the long axis of the petrous ridge [8].
In our study, of 37patients, 19(51.35%) had conductive hearing loss (CHL), 9(24.32%) had SNHL and the rest 9(24.32%) patients had mixed hearing loss (MHL) Table 1. In a similar study done by Honey-brook et al., incidence of 43% CHL, 27% SNHL, and 13% MHL in 129 temporal bone fracture patients was noted [9].
In 1997, Brodie and Thompson classified temporal bone fractures into otic capsule–sparing and otic capsule–violating, otic capsule violating had 4 times more SNHL than otic capsule sparing [10].
As reported by Ishman, it was indicated that ME involvement in non-petrous fracture exhibits a 4-fold stronger correlation with CHL than the traditional classification system (i.e., longitudinal, transverse, or mixed) [4].
A study done by Little SC et al. states that old classification could not predict complications of temporal bone fractures amongst sample population. No statistically significant difference was observed between the three fracture types (transverse, longitudinal, and mixed) in regard to facial nerve injury, SNHL, CHL, or CSF otorrhoea [11].
In a study done by Ishman, it was found that in 94% cases of petrous bone fractures middle ear (ME) involvement was noted and in cases of non-petrous fractures 77% had Mastoid(M) involved while in 35% cases EAC involvement was seen [4]. Kim So Young et al. classified temporal bone fracture based on the sub-site involvement, i.e., ossicular chain, the external auditory canal [EAC], middle ear [ME], and mastoid [M] [6]. Based on the HRCT temporal bone and audiograms of otic capsule-preserving temporal bone fracture patients were reviewed to evaluate the relationship between the temporal bone sub-site involvement and compared the initial and improved air-bone (AB) gap values to their hearing thresholds.
Correlation between hearing loss and otic capsule sparing fracture with temporal bone sub-sites showed very weak positive correlation (R value 0.2064). Study done by Kim So Young, et al. showed CHL that occurred after otic capsule-sparing temporal bone fractures varied in accordance with the temporal bone sub-sites [6].
The predictive value of radiological imaging in determining the hearing outcome is directly related to the otic capsular involvement. Even in otic capsule sparing temporal fractures, sensory neural hearing loss is seen in significant number of patients. Varied mechanisms of hearing loss following temporal bone trauma are described. Direct damage to the cochlea or internal auditory canal and disruption of the ossicular chain are the most obvious mechanisms of hearing loss and are apparent radiographically [12]. Hearing loss can result from injury to the membranes within the cochlea, or by microfractures of the cochlea which are often not apparent on computed tomographic scans. This microfracture can cause mixed or SNHL type of hearing loss. Hemorrhage of the bony labyrinth might seep through the peri- or endo-lymph, resulting in a labyrinthine concussion. In such a case, however, it is unlikely that imaging would detect the lesion, which might later be classed as an idiopathic etiology [13].
Early recognition of the type and degree of hearing loss is important to be recognized soon so that long-term follow-up is established, and appropriate hearing rehabilitation efforts initiated. Predictive role of imaging in determining the auditory outcome is not accurate and a low degree of correlation does exist when sub-site classification system is adapted in evaluation of temporal bone classification.
Conclusion
Conductive hearing loss was found to be more common in otic capsule sparing fractures. A very weak positive correlation was seen between temporal bone fracture sub-sites and hearing outcome.
Availability of data and materials
The dataset used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CSF:
-
Cerebro spinal fluid
- SNHL:
-
Sensori neural hearing loss
- GCS:
-
Glasgow Coma Scale
- M:
-
Mastoid
- EAC:
-
External auditory canal
- ME:
-
Middle ear
- O:
-
Ossicular chain disruption
- RTA:
-
Road traffic accident
- PTA:
-
Pure tone audiometry
- CHL:
-
Conductive hearing loss
- MHL:
-
Mixed hearing loss
- dB:
-
Decibels
- AB:
-
Air-bone
References
Amin Z, Sayuti R, Kahairi A et al (2008) Head injury with temporal bone fracture: one year review of case incidence, causes, clinical features and outcome. Med J Malaysia 63(5):373–376
Lyos AT, Marsh MA, Jenkins HA, Coker NJ (1995) Progressive hearing loss after transverse temporal bone fracture. Arch Otolaryngol Head Neck Surg. 121(7):795–799
Patel A, Eli G (2010) Management of temporal bone trauma. Cranio Maxilla Fac Trauma Reconstruct 3:105–113
Ishman SL, Friedland DR (2004) Temporal bone fractures: traditional classification and clinical relevance. Laryngoscope 114:1734–1741
Dahiya R, Keller JD, Litofsky NS, Bankey PE, Bonassar LJ, Megerian CA (1999) Temporal bone fractures: otic capsule sparing versus otic capsule violating clinical and radiographic considerations. J Trauma. 47(6):1079–1083
Kim SO, Kim YJ,·Kim YH, Park MH, Audiologic patterns of otic capsule preserving temporal bone fracture: effects of the affected subsites, Clin Experi Otorhinolaryngol 2016; 9(3): 206-211
Schubl S, Klein T, Robitsek R, Trepeta S, Fretwell K, Seidman D et al (2016) Temporal bone fracture: evaluation in the era of modern computed tomography. Injury. 47(9):1893–1897
Gurdjian ES, Lissner HR (1946) Deformation of the skull in head injury studied by the ‘stresscoat’ technique, quantitative determinations. Surg. Gynecol. Obstet. 73:219–233
Honeybrook A, Patki A, Chapurin N, Woodard C (2017) Hearing and mortality outcomes following temporal bone fractures. Craniomaxillofac Trauma Reconstr. 10:281–285
Brodie HA, Thompson TC (1997) Management of complications from 820 temporal bone fractures. Am J Otol. 18:188
Little SC, Kesser BW (2006) radiographic classification of temporal bone fractures clinical predictability using a new system. Arch Otolaryngol Head Neck Surg. 132(12):1300–1304
Saraiya PV, Aygun N (2009) Temporal bone fractures. Emerg Radiol. 16(4):255–265
Kim JH, Park KC, Shim DB (2011) Sudden sensorineural hearing loss occurring after blunt head trauma. Korea J Audiol 15(2):94–99
Acknowledgements
We would like to acknowledge the department of Audiology, and department of Radiology at our institute for their help and co-operation in data acquisition.
Funding
None
Author information
Authors and Affiliations
Contributions
VBK: conceptualization, analysis and interpretation, drafted, and revised the manuscript. AKM: analysis, interpretation, drafted, and revised the manuscript. NM: data collection, analysis, and drafted the manuscript. RG: data acquisition and drafted the manuscript. SJ: data acquisition and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional Ethics Review Board approval was taken for this study (S.S. Institution of Medical Sciences & Research Centre. Institutional Ethics Review Board, Reference: IERB/O No. 166/2018 dated 03.11.2018 to the reference IERB No. 259-2018). Informed written consent to participate has been taken from all the study participants and has been obtained by parents/guardians of participants less than 16 years old.
Consent for publication
Written Consent for publication has been taken from patients or their guardians when applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Keshavamurthy, V.B., Ajith, K.M., Maradi, N. et al. Correlation of hearing outcome in otic capsule sparing temporal bone fractures using temporal bone sub-site classification: a cross-sectional descriptive study. Egypt J Otolaryngol 38, 138 (2022). https://doi.org/10.1186/s43163-022-00326-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00326-7