Abstract
Background
Benign paroxysmal positional vertigo (BPPV) is the most frequent vestibular disorder with significant morbidity, psychosocial impact, and medical costs. This multi-center study work aimed to review BPPV clinical features, treatment, and outcomes.
Methods
After a detailed history, clinical examination, audiological assessment, and position provocation tests to diagnose BPPV type, the suitable repositioning maneuver was done. BPPV was diagnosed according to the criteria developed for this study through piloting and validation in a specialized dizziness clinic. The main outcome measures were patient demographics, comorbidities, canal involvement, response to treatment, and incidence of recurrence.
Results
Within included 114 patients, the affected canal was 93% posterior semicircular canal, 3.5% horizontal semicircular canal, and 3.5% anterior semicircular canal. The response after repositioning maneuver was (86%) after one session and 100% after the second session.
Conclusion
Meticulous BBPV assessment with choosing appropriated provocation test help to diagnose and identify the type of BPPV and so applying appropriated suitable repositioning maneuver.
Similar content being viewed by others
Background
Benign paroxysmal positional vertigo (BPPV) is a common vestibular disorder leads to significant morbidity, psycho-social impact, and medical costs. It is the most frequent cause of a vestibular disorder and represents about 20–30% of the vestibular vertigo with a lifetime prevalence reaches up to 2.4% in the general population [1].
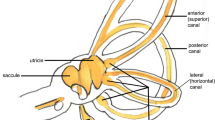
It is believed to be attributed to dislodged otoliths from utricular macula into any of the semicircular canals, which results canalithiasis, or cupulolithiasis, if otoliths adhere to the cupula of the semicircular canal [2]. This results in bending and stimulation of the cupula and provoking vertigo and nystagmus in the plane of the affected canal [3].
The time course of BPPV is characterized by spontaneous remissions that occur typically after days to weeks and recurrences that occur in about 50% of patients [4, 5]. Although BPPV is usually self-limiting, it inflicts a considerable personal and socioeconomic burden [1].
BPPV is categorized according to its cause into primary which is usually idiopathic and secondary. The primary type is the commonest type. The chief causes of secondary BPPV are after ear surgery, trauma to the head, vestibular neuronitis, insufficient blood supply of the vestibulobassilar system, and metabolic disorders [5, 6].
There is a paucity of literature on the epidemiology of BPPV otorhinolaryngology practice in the Arab population. Thus, this study aimed to review the clinical features, treatment, and outcomes of BPPV in tertiary university hospitals in Arab population. Specifically, we sought to determine if BPPV presents differently in Arab population versus world records to better guide recognition and treatment of this disorder.
Patients and methods
This study was conducted in the Otorhinolaryngology Department, Zagazig University, Egypt, and Alazhar University, Egypt, in collaboration with the Audiovestibular Department, Menoufia University, Egypt.
This is a prospective study which involved 114 patients in the period from January 2019 to March 2021. The institutional review board (IRB) approved the study methods, and detailed consents were gained prior to inclusion in the research.
All the patients were subjected to a full and detailed history, general and clinical ENT examination, position provocation tests (Dix-Hallpike and supine roll test), and audiological assessment (tympanometry and pure tone audiometry). Patients with congenital ear anomalies or ear malignancies are excluded from the study.
The symptoms were clearly documented using the same criteria of Brevern et al. [1] to diagnose the vestibular vertigo and BPPV.
In vestibular vertigo (one criterion must be fulfilled):
-
(1)
Self-generated rotational vertigo.
-
(2)
Positional vertigo.
-
(3)
Repeated dizziness with nausea and either imbalance or oscillopsia.
In Benign paroxysmal positional vertigo (A–D has to be fulfilled):
-
(A)
Recurrent vestibular vertigo.
-
(B)
Duration of the attack is less than 1 min.
-
(C)
Symptoms always evoked by change of head position as turning over in the supine position, lying down, recline the head, rising from supine position, or leaning forward.
-
(D)
Not another disorder.
BPPV in all patients was diagnosed by the above symptoms plus at least one positive test of Dix–Hallpike test, supine roll test, and deep midline head-hang test.
The test was considered positive when subjective vertigo was reported by the patient, and objective nystagmus was observed by the examiner. Nystagmus observed with the aid of videonystagmography (Visual Eyes by Micromedical Technologies, Chatham, IL) or Frenzel goggles (ICS-FL15, Otometrics, Denmark) in most of the cases.
Posterior semicircular canal BPPV (PSC-BPPV) was diagnosed by Dix–Hallpike test when a geotropic, torsional, upbeat nystagmus was observed associated with subjective vertigo while the affected ear down. Horizontal semicircular canal BPPV (HSC-0BPPV) was diagnosed by supine roll test when horizontal nystagmus was observed associated with subjective vertigo. It was considered geotropic if nystagmus beat toward the ground while the affected ear down and apogeotropic if nystagmus beat away from the ground while the affected ear up. Laterality was decided based on which side elicited more robust nystagmus and vertigo symptoms in cases where nystagmus and vertigo were present while either ear down. Anterior semicircular canal BPPV (ASC-BPPV) was diagnosed if apogeotropic, torsional, downbeat nystagmus was noticed while the affected ear up during the Dix–Hallpike test and/or downbeat nystagmus was noticed in the deep midline head-hang position.
Secondary BPPV was identified when a patient informs a history of acute unilateral vestibular loss or trauma to the head or surgery to the ear within 6 months of the onset of BPPV or intubation for general anesthesia within 3 days earlier.
All the patients are subjected to repositioning maneuver (Epley maneuver in cases of PSC-BPPV, barbeque maneuver in HSC-BPPV, and deep midline head-hang maneuver in ASC-BPPV) according to the affected canal.
After 2 weeks, if any of these patients is still complaining from vertigo, the patient subjected to the 2nd repositioning maneuver while using the oscillation on the mastoid. There are fixed instructions which are instructed to the patients to be followed in the first week after doing the repositioning maneuver either in the first or in the second attempt.
The patient has to avoid any trigger action which can allocate the otoconia again to any canal:
-
a)
Avoid head shaking movement.
-
b)
Avoid any exercises or any daily practice associated with angular head movement.
-
c)
In daytime, try to stay with your head in a vertical position.
-
d)
In sleep time, sleep with the upper half of the body in semi-upright position.
-
e)
Avoid sleep in the affected ear.
The patient is considered not responding to the rehabilitation if after 6 weeks the patient is still having vertigo as well as a positive provocation test with the characteristic nystagmus (the same inclusion criteria).
All data were shown as means and standard deviation (SD). All statistical data were analyzed with the SPSS program version 25 (Chicago, Illinois, USA). When the P value < 0.05, it was reported as statistically significant.
Results
This study included 114 patients who were diagnosed as BPPV: 54 (47.4%) females and 60 (52.6%) males. Their age ranged from 26 to 64 years; mean ± SD (43.2 ± 11.36) years (Table 1). Fourteen patients were single (12.3%), and 100 patients were married (87.7%).
The main complaint was false rotation sensation (vertigo) in 110 patients (96.5%) while 4 patients complained of imbalance (3.5%). Vertigo was associated with nausea ± vomiting in 36 patients (31.6%). Tinnitus was complained in 30 patients (26.3%), diminution of hearing in 26 patients (22.8%), otalgia in 4 patients (3.5%) and headache in 2 patients (1.8%) (Table 1).
Associated diseases that were documented with BPPV were reported in 24 patients (21%) including diabetes mellitus in 12 patients (10.5%), hypertension in 6 patients (5.26%), diabetes and hypertension in 5 patients (4.3.9%), hypothyroidism in 2 patients (1.75%), cataract in 2 patients (1.75%), and head trauma in 2 patients (1.75%) (Table 1).
Recurrent BPPV was reported in 22 patients (19.3%) and duration from previous attaches ranged from 1 month to 10 years. The duration of the symptoms ranged from 1 day to 6 months with a mean of 22.8 ± 26.8 days.
Otoscopic examination showed normal tympanic membrane (TM) in 100 patients (87.7%) while TM appeared dull in 10 patients (8.8%), retracted in 2 patients (1.75%), and perforated in 2 patients (1.75%) (Table 2).
Audiological examination by pure tone audiometry (PTA) revealed normal hearing in 84 patients (73.7%%), while 24 patients had a high-frequency sensorineural hearing loss (SNHL) (21%), 2 patients had mid-frequency mixed hearing loss (1.75%), and 4 patients had severed SNHL (3.5%) (Table 2).
The tympanometry was found type A in 108 patients (94.7%), type B in 4 patients (3.5%), and perforated in 2 patients (1.75%) (Table 2).
Dix Hall Pike gave up beating torsional nystagmus in 106 (93%) patients and down beating nystagmus in 4 (3.5%) patients and negative in 4 (3.5%) patients. Supine roll test was negative in 110 (96.5%) patients and left geotropic nystagmus in 4 (3.5%) patients where the Dix Hall Pike was negative. Deep midline head-hang position shows downbeat nystagmus in 4 (3.5%) patients (Table 2).
The canal affected was the posterior canal in 106 (93%) and the horizontal canal in 4 (3.5%) patients and the anterior canal in 4 (3.5%) patients (Table 3).
The side affected was the 56 canal in the right side (54 PSC and 2 ASC), and 58 canal was affected on the left side (52 PSC, 4 HSC, and 2 ASC). No bilateral canal affection was recorded (Table 3). The side affected in the four horizontal canal patients was left side, where the side affected in four anterior canal patients were two left sides and two right sides.
Regarding the severity, vertigo was severe in 24 patients (21%), moderate in 50 patients (43.9%), and mild in 40 patients (35,1%). The four affected horizontal canals showed a severe form while in the affected 4 anterior canals, two were mild and the other two were moderate.
Response to repositioning maneuver (Epley maneuver in cases of PSC-BPPV, Barbeque maneuver in HSC-BPPV, and deep midline head-hang maneuver in ASC-BPPV); 98 patients (86%) respond after one session (20 patient with co-morbidity and 78 without co-morbidity) and 16 patients (14%) (4 with co-morbidity and 12 without) (10 has posterior canal and 6 other canal affection) improved after 2 sessions (Table 4).
Discussion
Although the term “benign paroxysmal positional vertigo” (BPPV) was described for the first time in 1952 by Dix and Hallpike [7]; however, there is rarity in the literature on the epidemiology of BPPV.
The first study which estimate the prevalence and incidence of BPPV in the general adult population was performed by Brevern et al. in 2007 in Germany [1]. That study relied on telephone interview of the participants so it has many limitations as remote episodes can be easily forgotten, the diagnosis of BPPV depended on the analysis of the symptoms and not confirmed by positioning tests, and it could not differentiate between BPPV of the posterior canal and variants involving other canals.
In the current study, we tried to solve these limitations by doing a full study with full history-taking and positional provocation tests for BPPV not only to confirm the BPPV diagnosis but also to assess which canal is affected and hence apply the appropriate repositioning maneuver according to the affected canal and then assess the results. Complete physical and audiological examination has been done for all the patients to rule out any associated co-morbidity. To the best of our knowledge, this is the first such study in the Arab population.
This study involved 114 patients which is relatively larger than other similar studies; 60 patients in Panuganti et al. study [8], 75 patients in Babac and Arsović study [9], and 62 patients in Khatri et al. study [10].
In this study, the patients age ranged from 26 to 64 year (mean 43.2 ± 11.36) with nearly equal presentation in males (52.6%) and females (47.4%) like studies of Suarez et al. [11] and Sacco et al. [12]; however, in the study of Brevern et al. [1], there was a female predominance. Only 1.75% (2 patients) are secondary BPPV, and the remaining 98.25% (112 patients) are primary idiopathic. The associated diseases with BPPV were reported in 24 patients (21%); diabetes mellitus in 12 patients (10.5%), hypertension in 6 patients (5.26%), diabetes and hypertension in 5 patients (4.3.9%), hypothyroidism in 2 patients (1.75%), cataract in 2 patients (1.75%), and head trauma in 2 patients (1.75%) (Table 1).
The left side showed slightly more affection than the right while previous studies have found that BBPV affects predominantly the right labyrinth more than the left [13]. From the preceding study, it has been noticed that most of the patients sleep on their right side [14]. It has also been documented that a significant correlation has been found between position of the head during sleep and the affected side by BPPV [15].
In the study of Babac and Arsović [9], the result of initial Epley maneuver was 90.7% after first Epley maneuver, and 96% after the second. In the study of Panuganti et al. [8], 68% patient showed an improvement in symptoms after first Epleys maneuver, and 88% after the 2nd time. In the study of Korres et al. [16], the canalith repositioning procedure was immediately successful in 80.9% patients in a second session, resulting in a total success rate of 92.1%.
However, in this study, the success rate after the first repositioning maneuver was 86% and after the second repositioning maneuver the success rate was 100% and this is mostly due to the accuracy in diagnosing which canal is affected and hence choosing the appropriate repositioning maneuver. Epley maneuver was used in cases of PSC-BPPV, barbeque maneuver was used in HSC-BPPV, and deep midline head-hang maneuver was used in ASC-BPPV. Also, in this study, we consider the cases response to the maneuver if the provocation test was negative after 4 weeks from the last repositioning maneuver.
Conclusion
This study shows the clinical feature of BPPV in the Arab population and showed that careful and meticulous history with full clinical and audiological assessment of BPPV patients as well as choosing the appropriated provocation test which help not only the diagnosis but also identify the type of BPPV, and so applying the appropriated suitable repositioning maneuver will help in management of BPPV.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BBPV:
-
Benign paroxysmal positional vertigo
- PSC-BPPV:
-
Posterior semicircular canal BPPV
- HSC-BPPV:
-
Horizontal semicircular canal BPPV
- ASC-BPPV:
-
Anterior semicircular canal BPPV
References
Von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, Neuhauser H (2007) Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry 78(7):710–715
Parnes LS, Mcclure JA (1992) Free-floating endolymph particles: a new operative finding during posterior semicircular canal occlusion. Laryngoscope 102(9):988–992
Kim JS, Zee DS (2014) Benign paroxysmal positional vertigo. N Engl J Med 370(12):1138–1147
Imai T, Ito M, Takeda N, Uno A, Matsunaga T, Sekine K, Kubo T (2005) Natural course of the remission of vertigo in patients with benign paroxysmal positional vertigo. Neurology 64(5):920–921
Moreno NS, André AP (2009) Number of maneuvers need to get a negative Dix-Hallpike test. Braz J Otorhinolaryngol 75(5):650–653
Caldas MA, Ganança CF, Ganança FF, Ganança MM, Caovilla HH (2009) Clinical features of benign paroxysmal positional vertigo. Braz J Otorhinolaryngol 75:502–506
Dix M, Hallpike CS (1952) LXXVIII The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann Otol Rhinol Laryngol 61(4):987–1016
Panuganti A, Loka SR, Tati S, Punga AK (2019) Comparative study of management of BPPV (Benign Paroxysmal Positional Vertigo) with only drugs versus drugs plus Epley manoeuvre. Indian J Otolaryngol Head Neck Surg 71(2):1183–1186
Babac S, Arsović N (2012) Efficacy of Epley maneuver in treatment of benign paroxysmal positional vertigo of the posterior semicircular canal. Vojnosanit Pregl 69(8):669–674
Khatri M, Raizada RM, Puttewar MP (2005) Epley’s canalith-repositioning manoeuvre for benign paroxysmal positional vertigo. Indian J Otolaryngol Head Neck Surg 57(4):315
Suarez H, Alonso R, Arocena M, Suarez A, Geisinger D (2011) Clinical characteristics of positional vertigo after mild head trauma. Acta Otolaryngol 131(4):377–381
Sacco RR, Burmeister DB, Rupp VA, Greenberg MR (2014) Management of benign paroxysmal positional vertigo: a randomized controlled trial. J Emerg Med 46(4):575–581
von Brevern M, Seelig T, Neuhauser H, Lempert T (2004) Benign paroxysmal positional vertigo predominantly affects the right labyrinth. J Neurol Neurosurg Psychiatry 75(10):1487–1488
Sato G, Sekine K, Matsuda K, Takeda N (2012) Effects of sleep position on time course in remission of positional vertigo in patients with benign paroxysmal positional vertigo. Acta Otolaryngol 132(6):614–617
Shim DB, Kim JH, Park KC, Song MH, Park HJ (2012) Correlation between the head-lying side during sleep and the affected side by benign paroxysmal positional vertigo involving the posterior or horizontal semicircular canal. Laryngoscope 122(4):873–876
Korres SG, Balatsouras DG, Papouliakos S, Ferekidis E (2007) Benign paroxysmal positional vertigo and its management. Med Sci Monit 13(6):C275-82
Acknowledgements
None.
Funding
The authors declare no financial support or interest in this study.
Author information
Authors and Affiliations
Contributions
MWE: suggested and developed the research idea; reviewed literature; interpretation, and analysis of collected data; tabulated data, wrote the manuscript; assisted in preparing the tables and approved the submitted version. RMKMM: perform the vestibular tests, perform the canal repositioning maneuvers, kept the record of patients’ information;, interpretation, and analysis of collected data; assisted in writing methods and revising the written manuscript; prepared the tables, and approved the submitted version. MAM: developed the research idea; reviewed literature; assisted in interpretation, and analysis of collected data; assisted in preparing the tables and approved the submitted version. MH: reviewed the written manuscript, assist in preparing tables, revised the manuscript critically for important intellectual content, and approved the submitted version. AM: reviewed the written manuscript, assist in preparing tables, revised the manuscript critically for important intellectual content, and approved the submitted version. AAN: modify the research idea, review the literature, interpret the collected data, assist in writing the manuscript, assist in preparing tables, revise the written manuscript, revised the manuscript critically for important intellectual content. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed written consent was signed by all subjects to share in the study after an explanation of its purposes. Zagazig University Hospital IRB approval was obtained.
Consent for publication
The patients included in this research gave written informed consent to publish the data contained within this study. No patients less than 16 years old were included in this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Anwar, M.W., Mesriga, R.M.K.M., Mobasher, M.A. et al. Benign paroxysmal positional vertigo: a multi-center study. Egypt J Otolaryngol 38, 98 (2022). https://doi.org/10.1186/s43163-022-00295-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00295-x