Abstract
Background
Accidental falls in elderly represent a major healthcare problem; they are a major cause of accidental death in people above 65 years of age. They result in both physical and psychological trauma, where fear of falling is a major consequence that leads to a vicious cycle that makes elderlies more isolated and dependent, making them more vulnerable to falls. Falls are multifactorial, where dizziness is a common factor in elderlies. Thus, a multi-systemic approach is essential for the assessment of balance functions; it also serves as a guide for treatment planning, either in the presence of a cause-specific pathology or when presbyvestibulopathy is the sole issue. Vestibular rehabilitation is useful in training elderlies to improve their dizziness and balance functions.
Aim
The aim of the study is to assess fall risk in elderly participants and to assess the role of customized vestibular rehabilitation in decreasing dizziness and falls in elderlies identified to be at risk of falling.
Results
All elderlies diagnosed at fall risk showed statistically significant improvement in dizziness handicap inventory, dynamic gait index, and computerized dynamic posturography after vestibular rehabilitation. As for dizziness, handicap inventory participants showed statistically significant improvement in the total score and in each of its three aspects (functional, emotional, and physical) after vestibular rehabilitation. The Dynamic Gait Index showed statistically significant improvement after vestibular rehabilitation, where they all became non-fallers. Subjects improved significantly in sensory organization test, limits of stability, vestibular stimulation test, motor control test, and faller assessment test of computerized dynamic posturography. Performance on the subjective assessment test was not significantly correlated to the objective assessment methods. The Dynamic Gait Index is sensitive in the detection of elderlies at risk of falling.
Conclusions
Falls in elderlies is an important subject that must be taken seriously due to its major consequences. Full balance assessment is crucial for offering customized vestibular rehabilitation, which has proved to be useful in minimizing dizziness and fall risk in elderlies.
Similar content being viewed by others
Background
Fall is an accidental displacement of the body to a level below the current level. When the body’s center of gravity is lost, and no effort or ineffective effort is made to restore balance, the person falls [1, 2]. It can be caused by intrinsic and extrinsic factors. Therefore, this is a challenging condition for physicians, both in terms of diagnostic and therapeutic approach, due to the wide range of underlying conditions [1, 2].
The most common fall-related consequences are pain, bruising, lacerations, fractures including upper extremity and hip fractures, and intracranial bleeding in severe cases. Thirty percent of community-dwelling mature adults aged 65 years and over living in the UK fall at least once in their lifetime [3, 4]. The incidence of falls increases with aging reaching its peak to 51% of elderly people over 85 years [4,5,6].
Falls among the elderly are one of the major causes of morbidity and mortality worldwide. They constitute the most common cause of injuries among elderly and the second leading cause of unintentional deaths/injury after road-traffic accidents, where 40% of traumatic injuries-related hospitalizations are due to falls [7,8,9]. According to Centers for Disease Control (CDC) reports, 2.5 million nonfatal falls among older adults were treated in emergency departments, and more than 734,000 of these patients were hospitalized in 2013 [10]. About 10.2% of adults aged ≥ 65 years reported at least one fall-related injury in the USA [11].
This high prevalence of falls in elderly has a serious impact on their quality of life. It can result in prolonged hospitalization, restriction of physical activities due to injuries or due to fear of falling, changes in balance and postural control, social isolation, anxiety, and depression [12,13,14]. Fear of falling or post-fall syndrome faced by most of the elderlies is a post-traumatic stress syndrome, characterized by high levels of anxiety related to walking [15].
Recurrent falls are common in elderly [6, 16, 17]. WHO in 2011 published “Global Report on Falls Prevention in Older Age,” which stated that individuals at the age of 65 and above fall at least once every year at the rate of 35%, while the frequency of falls in elderly at the age of 70 or above rises by approximately 42%. This high recurrence of falls increases the associated morbidity and mortality; thus, efforts to reduce their incidence are necessary [14, 18].
Aging process is accompanied by physiological alterations in various body systems that may result in the occurrence of diseases and increased frailty in elderly people [1, 19]. This aging induced progressive multimodal impairment of balance, including the loss of vestibular and proprioceptive functions, and impairment of their central integration with other sensory inputs is called presbyvestibulopathy [20, 21]. The ability to respond to a stimulus and reflex actions begin to decline [22]. In addition, the skeletal muscle strength and mass are reduced with aging, decreasing elderly people’s functional capacity, thus increasing their risk of fall-related injuries [1, 19, 23]. All this results in alteration to the dynamic posture keeping system, decreasing its ability to maintain balance while facing unexpected disturbances during movement, ending in a vicious cycle of dizziness, falls, and fear of falling in elderly [24].
Falls are multifactorial, where dizziness is an important risk factor especially in elderly since it affects individual’s balance. The major reported cause of falls in elderlies is vestibular dysfunction [25]. Its prevalence increases with age, reaching 30% in those above 60 years of age [26, 27] and 50% in those above 85 years [27]. Its presence in the elderly is a strong predictor of falls. Thus, an approach based on the cause of dizziness is needed to lower the risk of falls in elderly.
Dizziness has a relevant effect on elderly’s quality of life, as it affects their social, functional, and psychological well-being, leading to psychological insecurity, loss of self-confidence, fear of going out alone, restriction of physical and social activities, anxiety, depression, panic, and depersonalization due to the consequences of fall or the fear of falling [19, 28].
The key point in the prevention of falls is the identification of risk factors, adequate diagnosis, and tailored management. Rehabilitation programs are used to achieve better postural stability and thus improve quality of life [29, 30].
Vestibular rehabilitation therapy (VRT) is an exercise-based treatment program designed to enhance gaze stability, enhance postural stability, improve vertigo, and improve activities of daily living. VRT facilitates vestibular recovery mechanisms: vestibular adaptation, substitution by the other eye-movement systems, substitution by vision, somatosensory cues, other postural strategies, and habituation. Customized VRT is indicated in presbyastasis according to each one’s deficits to effectively reduce patients’ disability perception and improve their quality of life [29, 31, 32].
As aging is an emerging theme, considering the demographic transition process that is happening, where the proportion of elderlies around the world is increasing, managing falls in elderlies is of great importance [33]. Identifying elderly persons at risk of falling and assessing their balance functions using reliable tools to design a customized rehabilitation program suitable for their age and physical abilities, to address their needs, is of great importance to decrease future falls and their associated morbidity and mortality.
Aim of the work
The aim of the study is to assess fall risk in elderly participants and to assess the role of customized vestibular rehabilitation in decreasing dizziness and falls in elderlies identified to be at risk of falling.
Materials
A pre- and post-study was conducted on a sample of thirty elderlies. All subjects included in the study signed an informed consent form to participate in the study. A detailed history of dizziness and previous falls was taken from each participant.
The dropouts and non-compliant elderly people were not included in the study group.
Inclusion criteria
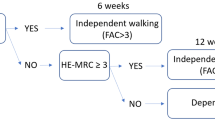
The inclusion criteria are as follows: (1) age 65 years or more; (2) ability to walk without support; (3) normal VNG findings (presbyvestibulopathy was taken into consideration as regards reduced caloric response: sum of bithermal maximum peak SPV on each side between 6 and 25°/s) [34]; (4) identified to be at fall risk by computerized dynamic posturography (CDP) and/or dynamic gait index (DGI); and (5) we also considered patients with benign paroxysmal positional vertigo (BPPV) that previously benefited from canalith repositioning procedures (i.e., with complete resolution of symptoms and signs).
Exclusion criteria
The exclusion criteria is as follows: (1) elderly with neurological disorders (e.g., dementia, Parkinson’s disease major sequelae after a stroke), psychiatric disorders, known cognitive problems, visual disturbances, and diabetics with peripheral neuropathy; (2) those receiving neuroleptics, sedatives, antiepileptics, and antidepressants; (3) those with chronic middle ear problems, Meniere’s disease, and previous vestibular neuritis; and (4) those with severe orthopedic dysfunction and arthrosis of the ankle, hip, and knee.
Methods
The study was conducted during the period from February 2019 to December 2021. All participants passed through the three stages of the study at the Audio-Vestibular Medicine Clinic of Alexandria Main University Hospital:
-
First stage: Pre-vestibular rehabilitation assessment
-
Second stage: Vestibular rehabilitation
-
Third stage: Post-vestibular rehabilitation assessment
The pre-vestibular rehabilitation assessment included:
-
1)
Videonystagmography (VNG): It was done utilizing Difra (Difra instrumentation, Belgium) equipment searching for spontaneous, gaze-evoked, positional, and positioning nystagmus. The oculomotor test battery (tracking, saccades, and optokinetic tests) and bithermal caloric test were all done to exclude any peripheral or central vestibular disorders. Canalith repositioning maneuvers were done to cases with BPPV; follow-up was done to them until their symptoms and signs were completely resolved; and then fall assessment was done to them by the Dynamic Gait Index (DGI) and computerized dynamic posturography (CDP); only those diagnosed to be at fall risk were included in the study (they were two cases).
-
2)
Dizziness Handicap Inventory (DHI): A self-report questionnaire aiming to measure the effects of dizziness on physical, emotional, and functional sub-domains [35]. It is a 25-item self-report questionnaire that quantifies the impact of dizziness on daily life by measuring self-perceived handicap. Item scores are summed. There is a maximum score of 100 (28 points for physical, 36 points for emotional and 36 points for functional) and a minimum score of 0.
-
3)
Dynamic Gait Index (DGI): It is designed to test eight facets of gait, including gait on even surface, gait with changing speed, gait with head turns in vertical and horizontal planes, stepping over or around obstacles, gait with pivot turns, and stair ascent and descent [36, 37]. Scoring is a four-point ordinal scale, ranging from 0 to 3. “0” indicates the lowest level of function and “3” the highest level of function. The best possible score on the DGI is a 24. Scores less than or equal 19/24 are predictive of falls in the elderly, while scores greater than 22/24 reflect safe ambulators.
-
4)
Computerized dynamic posturography (CDP): It was done using Synapsys Posturography System (SPS, SYNAPSYS, Marseille, France). Static and dynamic tests were done. Static tests include sensory organization test, limits of stability test, and vestibular stimulation test [38,39,40]. Dynamic assessment includes the motor control test and the faller assessment. The goal during posturography tests is to remain as stable as possible. In static posturography, the following parameters were measured: base of support with eyes open (mm2) which is equivalent to the stability limit; the motion parameters of center of gravity in the x-axis (mediolateral) and y-axis (anteroposterior) (mm); a statokinesigram (SKG), which is a graph of successive positions of center of pressure recorded by the platform; and the Romberg’s quotient (RQ) [41]. In dynamic posturography, the responses designed to restore balance are assessed based on measurements of pressure center displacements [40, 42].
-
I)
Static posturography:
-
i)
Sensory organization test (SOT): The subject stands on the platform (standard and foam), with his/her feet aligned to previously determined markings, corresponding to foot size. It includes six conditions: (1) eyes open and stable support, (2) eyes closed and stable support, (3) deceptive vision and stable support, (4) eyes open and foam platform, (5) eyes closed and foam platform, and (6) deceptive vision and foam platform.
Scores calculated from SOT include somatosensory score (condition 2/condition 1), visual score (condition 4/condition 1), vestibular score (condition5/condition 1), preferential score (condition 3 + condition 6/condition 2 + condition 5) which evaluates the subject’s ability to ignore the erroneous visual information to maintain his/her balance, the global score which is an overall score that takes into account all the conditions, assessing the subject’s ability to use its sensory input to keep his/her balance, and Romberg’s quotient (RQ) which is the ratio, expressed by a percentage, of the surface of the SKG with eyes closed (in static) on the surface of the SKG with eyes open (in static). It assesses the role of the visual afferent systems in postural control.
-
ii)
Limits of stability: It refers to the outmost range in any direction a person can lean from the vertical position, without changing the original base of support. The subject is asked to sway as far as possible in all directions while keeping their body straight and without moving their feet or falling, i.e., moving the body voluntarily en bloc using the ankle strategy. It is a measure of functional stability [43].
-
iii)
Vestibular stimulation test: Head movements are done in sagittal, frontal, and horizontal planes, while standing still on standard and foam platforms with eyes closed. It compares condition 2 and 5 of SOT with condition 2 and 5 with head movements. The head movements further stimulate the vestibular system against conditions 2 and 5 where the vestibular system is solicited only by the patient’s postural oscillations. The ratio of the conditions with head movement or without head movement indicates the patient’s ability to control his balance despite a significant vestibular solicitation, on a static and dynamic platform.
-
i)
-
II)
Dynamic posturography:
-
i)
Motor control test: The platform serves to induce destabilizing perturbations. Responses designed to restore balance are assessed based on measurements of center of pressure displacements.
-
a)
RAMP translator movement: The platform moves forward and backward in random order with eyes open and eyes closed. Mean energy expended by the patient to stabilize following a translational stimulation in the anteroposterior (AP) and the mediolateral (ML) planes, in addition to recovery time, which is the time necessary for the patient to retrieve a stable position following a translational stimulation in both AP and ML planes, are assessed.
-
b)
Sinus translator movement: The platform performs a slow and oscillatory movement in the anteroposterior plane, with eyes open and eyes closed. Gain and phase lag are assessed. Gain is the ratio between the postural response of the patient (AP and ML planes) and the translational stimulation. Phase lag is the lag between the stabilogram and the translational stimulation (by assimilating the postural response to a sinusoid). It investigates adaptation, stimulus anticipation, and feed-forward postural control mechanisms.
-
a)
-
ii)
Faller assessment test: It is an indicator of the risk of falls for the elderly. The tests of the assessment provide four evaluation criteria for the risk of fall. It depends on performance in motor control test and limits of stability. Getting 3 or 4 positive criteria is considered at risk for falls. It is a relevant index, which identifies the fallers with a responsiveness of 97% and the non-fallers with a specificity of 77% [44].
-
i)
-
I)
Vestibular rehabilitation
It includes adaptation, substitution, and habituation including optokinetic training for visual desensitization [45,46,47,48]. In addition to exercises specifically focused to the vestibular system, balance exercises under challenging sensory and dynamic conditions were included as part of vestibular rehabilitation, including strengthening exercises for ankle and hip strategies [49, 50]. Training was customized to each subject according to his/her capabilities, needs and value of VOR gain as measured by peak SPV in bithermal calorics (presbyvestibulopathy is considered when the sum of bithermal maximum peak SPV on each side is between 6 and 25°/s) [34]. Exercises are targeted to the deficits and symptoms of the patient [51]. VRT program consisted of two weekly 1-h supervised sessions. Subjects were advised to continue home-based exercises on the rest of the weekdays (repetitions of exercises done at the clinic if they are safe to be done at home alone). Safety measures were followed at the clinic and advised to be followed at home by giving the elderly a detailed description of how to maintain safety at home while performing the exercises. Progression of exercises was tailored to each subject as their performance improves; it was done by adding more challenges such as standing on foam, shifting from standing to walking, increasing the speed of walking, doing head turns, adding visual challenges to the background, and by adding cognitive tasks [52,53,54]. Maximum allowed duration of regular VRT exercises was 3 months.
Post- vestibular rehabilitation assessment
To assess the benefit of VRT on dizziness, postural control, and thus fall risk, the following were repeated at the end of the total period of vestibular rehabilitation to assess the benefit from VRT.
-
1)
Dizziness Handicap Inventory (DHI)
-
2)
Dynamic Gait Index (DGI)
-
3)
Computerized dynamic posturography (CDP)
Statistical analysis of the data
Data was analyzed using the IBM SPSS software package version 20.0 (Armonk, NY: IBM Corp). Qualitative data were described using number and percent. The Kolmogorov-Smirnov test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, and standard deviation. Significance of the obtained results was judged at the 5% level.
The used tests were paired t-test for normally distributed quantitative variables, to compare between two periods, and Wilcoxon signed ranks test for abnormally distributed quantitative variables, to compare between two periods.
Results
Sixty percent (18) of the study group were males, and 40% (12) were females. As for their age, 60% of them were below 80 years of age, and the remaining 40% were 80 years and above, where the mean age is 78.13 ± 4.11.
Dizziness Handicap Inventory (DHI)
There is statistically significant improvement in the total score and in each of its three aspects (functional, emotional, and physical) after vestibular rehabilitation, as seen in Table 1.
Level of change in the Dizziness Handicap Inventory (DHI) subscores after vestibular rehabilitation
Comparing the DHI subscores before and after vestibular rehabilitation (delta = Δ) showed that the largest improvement was in the functional subscore followed by the emotional then the physical subscore, as seen in Table 2.
Dynamic Gait Index (DGI)
There was statistically significant improvement in the DGI score after vestibular rehabilitation, where they all became non-fallers (Table 3).
Computerized dynamic posturography (CDP)
-
(i)
Sensory organization test (SOT): There is statistically significant improvement in the somatosensory, visual, vestibular, and global scores, both in anteroposterior and mediolateral planes. The Global Score is an overall score that considers all the conditions. This is a general assessment of the patient’s ability to use its sensory input to keep his/her balance.
In addition, there is statistically significant improvement in preferential anteroposterior and mediolateral scores (Table 4). This score evaluates patient’s ability to ignore the erroneous visual information to maintain his/her balance.
Distribution of cases studied by sensory organization test (SOT) performance
Using the limit values of Synapsys CDP to pass each sensory condition, subjects were divided into five groups. Three subjects (10%) passed only the somatosensory assessment, five (16.7%) passed only the visual assessment, none of them passed the vestibular assessment, twelve (40%) have passed both the somatosensory and the visual assessment, and finally ten subjects (33.3%) did not pass somatosensory, visual, and vestibular assessments (Table 5).
Percentage change (%Δ) in sensory organization test components after rehabilitation
Table 6 shows the %Δ (% improvement) of the SOT components, by comparing the values after VRT to the values before VRT. The results indicate that the greatest improvement is in the vestibular AP and ML scores.
-
(ii)
Romberg’s quotient (RQ): There is statistically significant decrease in its value post-vestibular rehabilitation, reflecting decrease in visual dependence to maintain body’s postural control, as seen in Table 7. RQ is the ratio, expressed by a percentage, of the surface of the SKG with eyes closed (in static) on the surface of the SKG with eyes open (in static).
-
(iii)
Limits of stability:
Elderlies showed statistically significant improvement in their limits of stability in static eyes open condition in all four directions (anterior, posterior, right and left) and in the total area, as seen in Table 8.
-
(iv)
Vestibular stimulation test: Tables 9, 10, and 11 show results with head movement in sagittal, frontal, and horizontal planes respectively, both on standard and foam platforms. Patients’ scores improved significantly, reflecting better ability to control balance despite a significant vestibular solicitation, on a static and dynamic platform.
-
(v)
RAMP translator movement, with eyes open and eyes closed; Tables 12 and 13, respectively, show statistically significant decrease in the mean energy expended by the patient to stabilize. In addition, there is statistically significant decrease in recovery time to retrieve a stable position.
-
(vi)
Sinus translator movement: Tables 14 and 15 show statistically significant decrease in gain and phase lag in both AP and ML planes during translator, sinus, eyes open, and eyes closed conditions respectively
-
(vii)
Faller assessment test: Elderlies showed statistically significant decrease in the number of faller assessment criteria, reflecting decrease in the fall risk, where all the candidates became non-fallers (Table 16).
Correlation between subjective and objective outcome measures
DHI total score which is the subjective assessment is not significantly correlated to the objective assessments DHI and faller assessment test, as seen in Table 17.
Relation between DGI and faller assessment test of CDP
In the pre-vestibular rehabilitation assessment, the faller assessment test diagnosed 2 subjects as non-fallers and the remaining 28 subjects as fallers, while the DGI diagnosed the 30 cases as fallers. In the post-rehabilitation assessment, both faller assessment test and DGI classified the 30 subjects as non-fallers (Table 18). This shows that the DGI is sensitive in detecting those at risk of falling.
Comparison of the performance on DHI, DGI, and faller assessment test among the four subgroups of the subjects
Performance improved in all four subgroups without a statistically significant difference in %Δ (% change) between them, as seen in Table 19. This suggests that profiling of elderlies according to their SOT performance cannot be used as a prognostic factor of benefit from VRT.
Discussion
The studied subjects showed a significant improvement in the subjective (DHI) and the objective (DGI and CDP) outcome measures, reflecting that the customized VRT program tailored to address their functional deficits proved to be effective in improving their postural control and balance functions. This was recommended by the American Geriatrics Society and the American Academy of Orthopedic Surgery for elderly with gait and balance disorders [55]. Improved balance functions decrease their risk of future falls and their serious consequences. It also reduces their feeling of dizziness and fear of engaging in activities of daily living by giving them more self-confidence in their new physical abilities.
Supervised vestibular rehabilitation exercises seem superior to home exercises, where they provide better patient compliance. Furthermore, it allows the therapist to regularly assess patients’ progress and provide them with feedback on their performance [56,57,58].
Elderly subjects at risk of falling were divided into 5 groups based on their performance in the SOT of CDP. Groups are as follows: passed only visual assessment, passed only somatosensory assessment, passed only vestibular assessment, passed both visual and somatosensory assessments, and failed visual, somatosensory, and vestibular assessments. Comparison of the percentage improvement in the performance of the DHI, DGI, and faller assessment test of CDP across the 4 groups showed no significant difference. Concluding that the subject’s performance on the SOT is not a prognostic factor of the benefit acquired from the VRT.
Elderlies showed a significant decrease in oscillations of the center of pressure in both anteroposterior and mediolateral planes while standing on firm and foam platforms with their eyes open and closed, which is important in elderlies’ daily lives, during activities such as getting out of bed at night. This significant improvement of displacement in the anteroposterior plane with open and closed eyes reflects the improved plantar flexor and dorsiflexor muscle action, which are part of the ankle’s strategy for maintaining postural control in case of anterolateral balance disturbance while standing upright. Similar findings have been documented in other studies [51, 57, 59, 60]; Rossi-Izquierdo et al. reported that the improvement in the balance assessment of the sensory organization test of CDP persisted during the 6 to 12 months follow-up [61].
Measuring the value of change (improvement) in SOT, vestibular subscores showed the highest level of improvement after VRT.
As for the Romberg’s quotient (RQ), elderly subjects showed a significant reduction in RQ after vestibular rehabilitation, reflecting a better ability to maintain the body’s balance in the absence of visual input or in the presence of complex or moving visual stimuli. This decreased visual dependence is important in everyday life. Similar results have been reported by other studies [41, 62].
As for the limits of stability, elderly subjects were able to maintain a balanced posture while moving their body over a larger area in all directions, en bloc using the ankle strategy, following vestibular rehabilitation and balance retraining therapy. Other authors have documented a similar improvement in limits of stability after vestibular rehabilitation [63, 64].
As for dynamic balance, its significant improvement reflects better defensive postural responses and feed-forward postural control mechanisms, even with eyes closed, thereby reflecting improved postural control and fall avoidance skills gained after vestibular rehabilitation, which are important in daily life as while using public transportation or while moving to reach an object, moving up or down stairs, and stepping over or around obstacles on the street [65]. Alfieri et al. reported a similar improvement [40].
Contrary to this study, other studies could not prove a statistically significant effect of vestibular rehabilitation on balance measures. No statistically significant improvements in the Timed Up and Go test (TUG) and the Guralnik test battery was observed, where the TUG test performance time did not decrease significantly after the rehabilitation. This may be due to the short duration of rehabilitation, or to the characteristics of the study sample (which had many associated diseases), which may have influenced the outcome of rehabilitation [40, 64]. On the other hand, other studies of elderly persons with instability present defects that make it difficult to reach a definitive conclusion. These studies do not focus on imbalance due to aging; they include patients with peripheral vestibular and/or central nervous system disorders, they use indirect measures to assess the risk of falling, and they do not solely study elderly patients [66,67,68,69]. In addition, an old study used only home-based rehabilitation exercises without a therapist’s supervision [70].
Reviews show that including two or more types of exercises, such as strength, balance, flexibility, or resistance, can reduce fall rates among elderlies [71,72,73].
Whitney et al. reported similar improvements in DHI and DGI, in addition to Activities-specific Balance Confidence Scale (ABC Scale), as a result of vestibular rehabilitation [74]. Studies assessing the quality of life of elderly people at risk of falling have shown a similar significant improvement in the functional, physical, and emotional scores of DHI following vestibular rehabilitation [32, 75,76,77].
As for the DHI subscores, the functional scores showed the highest change (improvement) followed by emotional and then physical scores. Other studies reported the highest level of improvement in the functional score like our study, but it was followed by the physical then the emotional scores [77,78,79]. In contrast, another study including elderlies showed the highest improvement in the physical score, which reflects dizziness due to changes in head position; this is especially more common in cases of BPPV which were excluded in our study, thus explaining the difference in results [80].
Studying the correlation between subjective (DHI) and objective assessments (DGI and faller assessment test of CDP) showed that performance on the DHI is not significantly correlated with performance scores of the DGI and the faller assessment test of CDP. Consequently, the DHI (subjective) cannot substitute the DGI and the CDP (objective). Another study showed that there is no correlation between the DHI and the SOT assessment; the explanation for this was that in daily life activities, these patients do not usually face the most complex conditions of the SOT (moving surface or visual surround); thus, they are not correlated with their disability [81, 82]. However, they found a correlation between the number of falls and the emotional scale of the DHI, confirming the psychological consequences of such falls [81]. This reflects that subjective assessment (DHI) is complementary to the objective tests, where it reflects the subject’s functional and physical abilities and emotional condition. However, it cannot be used alone in the assessment of falls due to the subject’s bias.
As regards the objective fall assessments used, the DGI and CDP, this study showed that the DGI is sensitive to detection of those at risk of falling as compared to the faller assessment test of CDP. This means that DGI can be reliably used to detect fallers, with the advantage of being less expensive, more feasible, easier to perform, and less time-consuming. Whitney et al. stated that DGI is a sensitive assessment tool to identify those at risk of falls due to vestibular disorders [83, 84]. The study by Herman et al. reported that DGI had good sensitivity for detecting fallers (91%) but poor specificity (3%) (based on reported falls) [85]. Shumway-Cook et al. reported that DGI had inter-rater reliability of 96% and test-retest reliability of 98%, but the threshold score of 19 or less correctly classified 59% of fallers [36].
Conclusion
Postural responses of elderly subjects to destabilizing events are significantly affected, and this has been reflected in static and dynamic posturography tests.
Tailored vestibular rehabilitation and balance training significantly improved their balance, neuromuscular coordination, and quality of life. It is recommended to use DGI as a screening tool for elderlies to identify those at risk of falls (even if they had not fallen before). Those at risk of falling should do CDP which provides an accurate and detailed analysis of the subjects’ balance strategies, to customize an appropriate rehabilitation program.
Availability of data and materials
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL, Thompson JH (2018) Interventions to prevent falls in community-dwelling older adults: a systematic review for the US preventive services Task force
Ungar A, Rafanelli M, Iacomelli I, Brunetti MA, Ceccofiglio A, Tesi F et al (2013) Fall prevention in the elderly. Clin Cases Miner Bone Metab 10(2):91
Nazarko L (2015) Modifiable risk factors for falls and minimizing the risk of harm. Nurse Prescribing 13(4):192–198
Al-Faisal W (2006) Falls prevention for older persons: Eastern Mediterranean regional review. World Health Organization, Geneva
Zijlstra G, Van Haastregt J, Van Eijk JTM, van Rossum E, Stalenhoef PA, Kempen GI (2007) Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing 36(3):304–309
Barker W (2014) Assessment and prevention of falls in older people. Nurs Older People 26(6):18–24
Organization WH, Ageing WHO, Unit LC (2008) WHO global report on falls prevention in older age. World Health Organization, Geneva
Bailly S, Haesebaert J, Decullier E, Dargent-Molina P, Annweiler C, Beauchet O et al (2014) Mortality and profiles of community-dwelling fallers. Results from the EPIDOS cohort. Maturitas 79(3):334–339
Alshammari SA, Alhassan AM, Aldawsari MA, Bazuhair FO, Alotaibi FK, Aldakhil AA et al (2018) Falls among elderly and its relation with their health problems and surrounding environmental factors in Riyadh. J Fam Community Med 25(1):29
Prevention CfDCa. Home and recreational safety. Older Adult Falls. http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html2013. Accessed 2013.
Moreland B, Kakara R, Henry A (2020) Trends in nonfatal falls and fall-related injuries among adults aged≥ 65 years—United States, 2012–2018. Morb Mortal Wkly Rep 69(27):875
Malasana G, Brignole M, Daccarett M, Sherwood R, Hamdan MH (2011) The prevalence and cost of the faint and fall problem in the state of Utah. Pacing Clin Electrophysiol 34(3):278–283
Paradela EMP, Lourenço RA, Veras RP (2005) Validation of geriatric depression scale in a general outpatient clinic. Rev Saude Publica 39:918–923
Soriano TA, DeCherrie LV, Thomas DC (2007) Falls in the community-dwelling older adult: a review for primary-care providers. Clin Interv Aging 2(4):545
Bloch F, Blandin M, Ranerison R, Claessens Y, Rigaud A, Kemoun G (2014) Anxiety after a fall in elderly subjects and subsequent risk of developing post traumatic stress disorder at two months. A pilot study. J Nutr Health Aging 18(3):303–306
Goodwin VA, Abbott RA, Whear R, Bethel A, Ukoumunne OC, Thompson-Coon J et al (2014) Multiple component interventions for preventing falls and fall-related injuries among older people: systematic review and meta-analysis. BMC Geriatr 14(1):1–8
Pohl P, Nordin E, Lundquist A, Bergström U, Lundin-Olsson L (2014) Community-dwelling older people with an injurious fall are likely to sustain new injurious falls within 5 years-a prospective long-term follow-up study. BMC Geriatr 14(1):1–7
Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM et al (2009) Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 169(21):1952–1960
Kehler D, Theou O, Rockwood K (2019) Bed rest and accelerated aging in relation to the musculoskeletal and cardiovascular systems and frailty biomarkers: a review. Exp Gerontol 124:110643
Tuunainen E, Jäntti P, Poe D, Rasku J, Toppila E, Pyykkö I (2012) Characterization of presbyequilibrium among institutionalized elderly persons. Auris Nasus Larynx 39(6):577–582
Tuunainen E, Poe D, Jäntti P, Varpa K, Rasku J, Toppila E et al (2011) Presbyequilibrium in the oldest old, a combination of vestibular, oculomotor and postural deficits. Aging Clin Exp Res 23(5):364–371
Sirohi A, Kaur R, Goswami AK, Mani K, Nongkynrih B, Gupta SK (2017) A study of falls among elderly persons in a rural area of Haryana. Indian J Public Health 61(2):99
Melo L, Arreguy-Sena C, Gomes A, Parreira P, Pinto P, Rocha J (2020) Social representations elaborated by elderly people about being elderly or aged: structural and procedural approaches. Revista de Enfermagem da UFSM 10(53):1–20
Teixeira AR, Wender MH, Gonçalves AK, Freitas CLR, Dos Santos AMPV, Soldera CLC (2016) Dizziness, physical exercise, falls, and depression in adults and the elderly. Int Arch Otorhinolaryngol 20(02):124–131
MacIntosh G, Joy J (2007) Assessing falls in older people. Nurs Older People 19(7):33–38
Barin K, Dodson EE (2011) Dizziness in the elderly. Otolaryngol Clin N Am 44(2):437–454
Jönsson R, Sixt E, Landahl S, Rosenhall U (2004) Prevalence of dizziness and vertigo in an urban elderly population. J Vestib Res 14(1):47–52
Vanleerberghe P, De Witte N, Claes C, Verte D (2019) The association between frailty and quality of life when aging in place. Arch Gerontol Geriatr 85:103915
Mira E (2008) Improving the quality of life in patients with vestibular disorders: the role of medical treatments and physical rehabilitation. Int J Clin Pract 62(1):109–114
Ferreira LMBM, Ribeiro KMO, de Lima KC, Júnior JD, Guerra RO, de Vasconcelos Ribeiro AJ et al (2012) Quality of life assessment in elderly with dizziness complain. J Surg Clin Res 3(2):59–67
Deveze A, Bernard-Demanze L, Xavier F, Lavieille J-P, Elziere M (2014) Vestibular compensation and vestibular rehabilitation. Current concepts and new trends. Neurophysiol Clin 44(1):49–57
Patatas OHG, Ganança CF, Ganança FF (2009) Quality of life of individuals submitted to vestibular rehabilitation. Braz J Otorhinolaryngol 75(3):387–394
United Nations DoE, Social Affairs PD (2020) World population ageing 2019 (ST/ESA/SER. A/444). United Nations, Department of Economic and Social Affairs, Population Division, New York
Agrawal Y, Van de Berg R, Wuyts F, Walther L, Magnusson M, Oh E et al (2019) Presbyvestibulopathy: diagnostic criteria consensus document of the classification committee of the Bárány Society. J Vestib Res 29(4):161–170
Jacobson GP, Newman CW (1990) The development of the dizziness handicap inventory. Arch Otolaryngol Head Neck Surg 116(4):424–427
Shumway-Cook A, Baldwin M, Polissar NL, Gruber W (1997) Predicting the probability for falls in community-dwelling older adults. Phys Ther 77(8):812–819
Woollacott MH, Tang P-F (1997) Balance control during walking in the older adult: research and its implications. Phys Ther 77(6):646–660
Asai M, Watanabe Y, Ohashi N, Mizukoshi K (1993) Evaluation of vestibular function by dynamic posturography and other equilibrium examinations. Acta Otolaryngol 113(sup504):120–124
Musat G, Anghel A, Radu L, Decusara R (2018) Comparative analysis of the data obtained in computerized posturography and videonystagmography for patients with peripheral vestibular deficit. Rom J Rhinol 8(32):225–231
Alfieri FM, Riberto M, Abril-Carreres À, Boldó-Alcaine M, Rusca-Castellet E, Garreta-Figuera R et al (2012) Effectiveness of an exercise program on postural control in frail older adults. Clin Interv Aging 7:593
Howcroft J, Lemaire ED, Kofman J, McIlroy WE (2017) Elderly fall risk prediction using static posturography. PLoS One 12(2):e0172398
Ghulyan V, Paolino M, Lopez C, Dumitrescu M, Lacour M (2005) A new translational platform for evaluating aging or pathology-related postural disorders. Acta Otolaryngol 125(6):607–617
Nashner LM (1993) Computerized dynamic posturography. In: Handbook of balance function testing, pp 208–307
Ghulyan V, Paolino M (2005) Posturography for evaluating risk of falls in elderly unstable patients. French Otorhinolaryngol 88:97–103
Herdman S (1989) Exercise strategies for vestibular disorders. Ear Nose Throat J 68(12):961–964
Pavlou M, Bronstein AM, Davies RA (2013) Randomized trial of supervised versus unsupervised optokinetic exercise in persons with peripheral vestibular disorders. Neurorehabil Neural Repair 27(3):208–218
Pavlou M (2010) The use of optokinetic stimulation in vestibular rehabilitation. J Neurol Phys Ther 34(2):105–110
Gottshall KR, Sessoms PH, Bartlett JL (2012) Vestibular physical therapy intervention: utilizing a computer assisted rehabilitation environment in lieu of traditional physical therapy. In: 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE, San Diego
Sulway S, Whitney SL (2019) Advances in vestibular rehabilitation. Vestib Disord 82:164–169
Klatt B, Carender W, Lin C, Alsubaie S, Kinnaird C, Sienko K et al (2015) A conceptual framework for the progression of balance exercises in persons with balance and vestibular disorders. Phys Med Rehabil Int 2(4):1044
Kristinsdottir EK, Baldursdottir B (2014) Effect of multi-sensory balance training for unsteady elderly people: pilot study of the “Reykjavik model”. Disabil Rehabil 36(14):1211–1218
Dannenbaum E, Loo C, Perroti R, Posthuma R, Weng AJ, Yang XT et al (2019) An innovative visuolocomotor training program for people on waiting list for vestibular rehabilitation. In: 2019 International Conference on Virtual Rehabilitation (ICVR). IEEE, Reykjavik, Iceland
Mosley E (2015) Vestibular rehabilitation for a 17-year old female with post-concussion symptoms: a case report
Register-Mihalik JK, Littleton AC, Guskiewicz KM (2013) Are divided attention tasks useful in the assessment and management of sport-related concussion? Neuropsychol Rev 23(4):300–313
Society AG (2001) Guideline for the prevention of falls in older persons: American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons panel on falls prevention. J Am Geriatr Soc 49:664–672
Pavlou M, Lingeswaran A, Davies RA, Gresty MA, Bronstein AM (2004) Simulator based rehabilitation in refractory dizziness. J Neurol 251(8):983–995
Black FO, Angel CR, Pesznecker SC, Gianna C (2000) Outcome analysis of individualized vestibular rehabilitation protocols. Otol Neurotol 21(4):543–551
Itani M, Koaik Y, Sabri A (2017) The value of close monitoring in vestibular rehabilitation therapy. J Laryngol Otol 131(3):227–231
Nagy E, Feher-Kiss A, Barnai M, Domján-Preszner A, Angyan L, Horvath G (2007) Postural control in elderly subjects participating in balance training. Eur J Appl Physiol 100(1):97–104
Orr R, Raymond J, Singh MF (2008) Efficacy of progressive resistance training on balance performance in older adults. Sports Med 38(4):317–343
Rossi-Izquierdo M, Gayoso-Diz P, Santos-Pérez S, Del-Río-Valeiras M, Faraldo-García A, Vaamonde-Sánchez-Andrade I et al (2018) Vestibular rehabilitation in elderly patients with postural instability: reducing the number of falls—a randomized clinical trial. Aging Clin Exp Res 30(11):1353–1361
Şahin E, Dinç ME, Özker BY, Çöpürgensli C, Konaklıoğlu M, Özçelik T (2017) The value of vestibular rehabilitation in patients with bilateral vestibular dysfunction. J Int Adv Otol 13(3):385–389
Rossi-Izquierdo M, Gayoso-Diz P, Santos-Pérez S, Del-Río-Valeiras M, Faraldo-García A, Vaamonde-Sánchez-Andrade I et al (2017) Short-term effectiveness of vestibular rehabilitation in elderly patients with postural instability: a randomized clinical trial. Eur Arch Otorhinolaryngol 274(6):2395–2403
Soto-Varela A, Rossi-Izquierdo M, del-Río-Valeiras M, Vaamonde-Sánchez-Andrade I, Faraldo-García A, Lirola-Delgado A et al (2020) Vestibular rehabilitation using posturographic system in elderly patients with postural instability: can the number of sessions be reduced? Clin Interv Aging 15:991
Shumway-Cook A, Woollacott MH (1995) Theory and practical applications. Mot. Control 31:51–57
Hansson EE, Månsson N-O, Ringsberg KA, Håkansson A (2008) Falls among dizzy patients in primary healthcare: an intervention study with control group. Int J Rehabil Res 31(1):51–57
Ricci NA, Aratani MC, Doná F, Macedo C, Caovilla HH, Ganança FF (2010) A systematic review about the effects of the vestibular rehabilitation in middle-age and older adults. Braz J Phys Ther 14:361–371
Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M et al (1994) A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med 331(13):821–827
Macias JD, Massingale S, Gerkin RD (2005) Efficacy of vestibular rehabilitation therapy in reducing falls. Otolaryngology—Head and Neck. Surgery. 133(3):323–325
Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM (1997) Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 315(7115):1065–1069
Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C (2011) Exercise for improving balance in older people. Cochrane Database Syst Rev 4(11):4963
Hubbard RE, Fallah N, Searle SD, Mitnitski A, Rockwood K (2009) Impact of exercise in community-dwelling older adults. PLoS One 4(7):e6174
Clemson L, Singh MAF, Bundy A, Cumming RG, Manollaras K, O’Loughlin P et al (2012) Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): randomised parallel trial. BMJ 345:e4547
Whitney SL, Wrisley DM, Marchetti GF, Furman JM (2002) The effect of age on vestibular rehabilitation outcomes. Laryngoscope 112(10):1785–1790
Zanardini FH, Zeigelboim BS, Jurkiewicz AL, Marques JM, Martins-Bassetto J (2007) Vestibular rehabilitation in elderly patients with dizziness. Pró-Fono Revista de Atualização Científica 19:177–184
Gazzola JM, Perracini MR, Ganança MM, Ganança FF (2006) Functional balance associated factors in the elderly with chronic vestibular disorder. Rev Bras Otorrinolaringol 72:683–690
Bayat A, Pourbakht A, Saki N, Zainun Z, Nikakhlagh S, Mirmomeni G (2012) Vestibular rehabilitation outcomes in the elderly with chronic vestibular dysfunction. Iran Red Crescent Med J 14(11):705
Mantello EB, Moriguti JC, Rodrigues-Júnior AL, Ferrioli E (2008) Vestibular rehabilitation’s effect over the quality of life of geriatric patients with labyrinth disease. Braz J Otorhinolaryngol 74(2):172–180
Ganança F, Castro A, Natour J, Branco F (2003) Dizziness Handicap Inventory: cross-cultural adaptation to Brazilian Portuguese, its application, reproducibility and comparison with the vestibular evaluation results. In: Arch for Senso Neuro Sci Prac [periódico online] [citado 2007 Fev 22]
Ganança FF, Castro ASO, Branco FC, Natour J (2004) Impact of dizziness on the quality of life in patients with peripheral vestibular dysfunction. Rev Bras Otorrinolaringol Eng Ed 70(1):94–101
Rossi-Izquierdo M, Santos-Pérez S, Del-Río-Valeiras M, Lirola-Delgado A, Faraldo-García A, Vaamonde-Sánchez-Andrade I et al (2015) Is there a relationship between objective and subjective assessment of balance in elderly patients with instability? Eur Arch Otorhinolaryngol 272(9):2201–2206
Badke MB, Miedaner JA, Grove CR, Shea TA, Pyle GM (2005) Effects of vestibular and balance rehabilitation on sensory organization and dizziness handicap. Ann Otol Rhinol Laryngol 114(1):48–54
Whitney S, Hudak M, Marchetti G (2000) The dynamic gait index relates to self-reported fall history in individuals with vestibular dysfunction. J Vestib Res 10(2):99–105
Whitney S, Wrisley D, Furman J (2003) Concurrent validity of the Berg Balance Scale and the Dynamic Gait Index in people with vestibular dysfunction. Physiother Res Int 8(4):178–186
Herman T, Inbar-Borovsky N, Brozgol M, Giladi N, Hausdorff JM (2009) The Dynamic Gait Index in healthy older adults: the role of stair climbing, fear of falling and gender. Gait Posture 29(2):237–241
Acknowledgements
Not applicable.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
“SF” did the practical part of the research, collected data, did statistical analysis, and wrote the paper. “HK”, “FB,” and “SA” revised the research results and written paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics committee of Faculty of Medicine Alexandria University has evaluated the research in its regular monthly meeting on 17 January 2019. The research has been accepted and approved.
Serial number: 0201203
IRB Number: 00012098 (expires October 6, 2022)
FWA Number: 00018699 (expires January 21, 2026)
As for consent to participate, all subjects included in the study signed an informed consent form to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fawzan, S., Kozou, H., Baki, F. et al. Fall risk assessment and effect of vestibular rehabilitation in the elderly population. Egypt J Otolaryngol 38, 88 (2022). https://doi.org/10.1186/s43163-022-00277-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00277-z