Abstract
Background
The diffuse sclerosing variant of papillary thyroid carcinoma is a rare pathologic entity. It is characterized by a tendency for rapid growth and a higher incidence of cervical lymph node and distant metastases.
We report an unusual presentation of diffuse sclerosing variant of papillary thyroid carcinoma presented as a single thyroid mass of a small size.
Case presentation
We experienced a case of a diffuse sclerosing variant of papillary thyroid carcinoma in a 30-year-old woman. The preoperative findings on the cytology and ultrasound were suggestive of a malignant thyroid nodule. This case was confirmed by surgical excision. The management included surgery, radioiodine ablation, and suppressive levothyroxine therapy.
Conclusions
We would like to highlight that an early diagnosis associated with an appropriate management leads to a good prognosis.
Similar content being viewed by others
Background
Papillary thyroid carcinoma (PTC) is the most common type of thyroid carcinoma accounting for approximately 80% of all thyroid gland malignancies.
The diffuse sclerosing variant (DSV) is a rare subtype of papillary thyroid carcinoma [1]. It was first described in 1985 by Vickery et al. as an unusual form of PTC, for which they proposed the term “diffuse sclerosis variant” [2, 3]. According to the World Health Organization classification, DSV occurs in young female adults and less commonly in children [1, 2]. It is characterized by an aggressive clinical behavior with a higher frequency of cervical lymph nodes and distant metastasis [4]. Histologically, it presents as a usually diffuse involvement of one or both thyroid lobes, without the formation of a dominant mass. In addition to classic nuclear features of PTC, extensive squamous metaplasia, numerous psammoma bodies, patchy to dense lymphocytic infiltrates, and small papillary structures within dilated lympho-vascular spaces and stromal fibrosis lead to the diagnosis of DSV [3, 4].
Herein we report an unusual presentation of diffuse sclerosing variant of papillary thyroid carcinoma presented as a single thyroid mass of a small size.
Case presentation
A 30-year-old female presented to our department with a 1-month history of a cervical mass. She had not experienced hoarseness, dysphagia, odynophagia, or breathing difficulty. Her past medical history was free from prior radiation therapy and a family history of thyroid diseases. She was clinically euthyroid. At physical examination, we found a single mass of the right thyroid lobe, small-sized (off 1 cm), without palpable cervical lymph nodes.
Cervical ultrasound examination revealed an ill-defined hypo-echogenic mass of the thyroid gland right lobe, measuring 1.5 cm in diameter, with diffused micro-calcifications without extra capsular extension associated with an enlarged right cervical lymph node of 1 cm in sector IIa (Fig. 1).
Thyroid function tests were normal. Fine needle aspiration of this nodule indicated Bethesda IV anomalies which is associated with malignancy in 15–30% of case. The patient underwent a right lobectomy. Per-operatively, we noticed a mal limited indurated nodule of the right thyroid lobe with adherence and enlarged central lymph nodes. Due to the preoperative findings, a frozen section examination of the nodule was indicated to label the histological type of the thyroid malignancy. It confirmed the diagnosis of papillary carcinoma; then, a total thyroidectomy, a bilateral central lymph node dissection, and a right lateral lymph node dissection were performed. The postoperative course was uneventful.
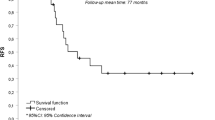
Macroscopic examination showed a white firm, ill-defined nodule, measuring 1.4 cm in greatest diameter with a rubbery cut surface. The surgical specimens were included and examined histologically. There was a diffuse involvement of the thyroid by a widely invasive tumor associated with dense fibrous stroma. The tumor had a papillary pattern with solid cribriform areas and extensive squamous metaplasia (Fig. 2). Tumor cells showed a characteristic nuclear atypia of papillary thyroid carcinoma. Numerous psammoma bodies were observed in addition to a marked lymphocytic infiltration with the formation of germinal centers within the fibrous stroma. Vascular invasion by tumor cells was seen (Figs. 3 and 4). Microscopic examination revealed multiple metastatic cervical lymph nodes, either. The final diagnosis was the DSV of PTC. She underwent radio ablative therapy followed by suppressive levothyroxine therapy. There was no residual uptake on subsequent 123-Iodine isotope scanning. There was no evidence of recurrence after 5 years follow-up.
Discussion
DSV is an uncommon variant of PTC accounting for 1.8% of all PTCs [1]. Compared with classical PTC, it is characterized by younger patient age and larger mean size of the tumor with a higher tendency for cervical lymph node metastasis and distant metastasis [5].
Definitive diagnosis is made on the basis of the presence of several pathological features including a diffuse firm enlargement of the thyroid gland with scattered islands of papillary carcinoma, extensive lymphatic permeation, and lymphocytic infiltration, extensive squamous metaplasia, a large number of psammoma bodies, and a prominent fibrosis. These histological features are essential in distinguishing PTC from benign pathologies such as Riedel’s and Hashimoto’s thyroiditis [6, 7]. The preoperative diagnosis of DSV remains difficult, and it can be diagnosed preoperatively based on a combination of typical imaging findings and careful cytological examination [8, 9].
Cervical ultrasonography (US) is generally considered as the most accurate imaging modality for the characterization of the thyroid gland pathologies. The US features of DSV are heterogeneous echotexture, solid composition, ill-defined margins, and scattered microcalcifications [6, 8, 10].
In our case, cervical ultrasound examination revealed an ill-defined mass of the thyroid gland right lobe with diffused micro-calcifications associated.
However, the diffuse nature of DSV often mimics chronic thyroiditis particularly in the absence of a focal solid mass [6]. The preoperative neck US may help detect intrathyroidal extension and lymph node metastases in DSV patients [6, 9]. The mean incidence of distant metastasis reported in DSV is 14.9% [5, 8], and the most common site is the lung. Early studies suggested that DSV had a poorer prognosis than classical PTC [10, 11]. It had also been reported that eradication required a more aggressive therapeutic approach.
In our case, a total thyroidectomy, a bilateral central lymph node dissection, and a right lateral lymph node dissection were performed. More recent studies revealed that DSV has a similar prognosis to patients with classical PTC [1, 8], and then the treatment should be the same radical surgery including total thyroidectomy and extensive lymph node dissection, radio-iodine ablation, and suppressive hormonotherapy [12, 13].
Conclusion
DSV is one of the most aggressive forms of papillary thyroid cancer. Therefore, it is important to diagnose this as quickly as possible to ensure appropriate treatment. The management includes total thyroidectomy associated with lymph node dissection and postoperative radioiodine therapy. A close follow-up is necessary.
Availability of data and materials
Not applicable.
References
Lam AK-Y, Lo C-Y, Lam KS-L (2005) Papillary carcinoma of the thyroid: a 30- yr clinicopathological review of the histological variants. EndocrPathol 16(4):323–30
Hedinger C, Williams ED, Sobin LH (1989) The WHO histological classification of thyroid tumors: a commentary on the second edition. Cancer 63(5):908–11
Vickery AL, Carcangiu ML, Johannessen JV, Sobrinho-Simoes M (1985) Papillary carcinoma. Semin Diagn Pathol 2(2):90–100
Vuong HG (2017) Prognostic significance of diffuse sclerosing variant papillary thyroid carcinoma: a systematic review and meta-analysis. Eur J Endocrinol. 176(4):433–41
Imamura Y, Kasahara Y, Fukuda M (2000) Multiple brain metastases from a diffuse sclerosing variant of papillary carcinoma of the thyroid. EndocrPathol 11(1):97–108
Jeong SH, Hong HS, Lee EH, Kwak JJ (2016) The diffuse sclerosing variant of papillary thyroid cancer presenting as innumerable diffuse microcalcifications in underlying adolescent Hashimoto’s thyroiditis: a case report. Medicine (Baltimore) 95(12):e3141
Walsh J, Griffin TP, Ryan CB, Fitzgibbon J, Sheahan P, Murphy MS (2015) A case report demonstrating how the clinical presentation of the diffuse sclerosing variant of papillary thyroid carcinoma can mimic benign Riedel’s thyroiditis. Case Rep Endocrinol 2015:686085
Akaishi J, Sugino K, Kameyama K, Masaki C, Matsuzu K, Suzuki A et al (2015) Clinicopathologic features and outcomes in patients with diffuse sclerosing variant of papillary thyroid carcinoma. World J Surg 39(7):1728–1735
Marshall CB (2015) Diffuse sclerosing variant of papillary thyroid carcinoma preoperative diagnosis through imaging and cytology allows for optimal patient care. AJSP Rev Rep 20(3):125
Kim HS, Han B-K, Shin JH, Ko EY, Sung CO, Oh YL et al (2010) Papillary thyroid carcinoma of a diffuse sclerosing variant: ultrasonographic monitoring from a normal thyroid gland to mass formation. Korean J Radiol 11(5):579–582
Falvo L, Giacomelli L, D’Andrea V, Marzullo A, Guerriero G, de Antoni E (2006) Prognostic importance of sclerosing variant in papillary thyroid carcinoma. Am Surg 72(5):438–444
Malandrino P, Russo M, Regalbuto C, Pellegriti G, Moleti M, Caff A et al (2016) Outcome of the diffuse sclerosing variant of papillary thyroid cancer: a meta-analysis. Thyroid Off J Am Thyroid Assoc 26(9):1285–1292
Chereau N, Giudicelli X, Pattou F, Lifante J-C, Triponez F, Mirallié E et al (2016) Diffuse sclerosing variant of papillary thyroid carcinoma is associated with aggressive histopathological features and a poor outcome: results of a large multicentric study. J Clin Endocrinol Metab 101(12):4603–4610
Acknowledgements
Not applicable
Funding
None.
Author information
Authors and Affiliations
Contributions
Authors' Contributions: MG: data analysis and interpretation and final approval of the version to be published. JH: conception of the work, data collection and drafting the article. LC: data collection. NA: Analysis and interpretation of the data and drafting of the article. ME and MA: data collection. MB, KW and MA: critical revision of the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
A written informed consent to publish this information was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Houas, J., Ghammam, M., Chouchane, L. et al. An unusual presentation of diffuse sclerosing variant of papillary thyroid carcinoma. Egypt J Otolaryngol 38, 78 (2022). https://doi.org/10.1186/s43163-022-00269-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00269-z