Abstract
Background
Unilateral otitis media with effusion in adult patient is considered alarming finding needing a detailed examination of the nasopharynx. The lesions in this area ranged from benign to more destructive malignant pathologies. Lipoma as a cause of obstruction is an extremely rare entity. We are reporting a case of eustachian tube lipoma presented with refractory otitis media with effusion. This is an extremely rare location of such entity and to the best of our knowledge, this is the third case reported in the world literature of eustachian tube lipoma after 2 cases published in 2011 and 2016 respectively. However, this is the first case reported in the literature of eustachian tube sialolipoma.
Case presentation
We are reporting a 27-year-old male who presented to our outpatient department with a complain of unilateral ear block, hearing loss, and intermittent tinnitus. Clinical evaluation revealed unilateral otitis media with effusion that was confirmed by pure tone audiogram and tympanometry. Computed tomography and magnetic resonance imaging were obtained showed a lesion originating in the eustachian tube area protruding in the nasopharynx. Surgical removal was successful with complete recovery.
Conclusions
Unilateral otitis media with effusion necessitate nasal endoscopic examination to rule-out lesions at the nasopharynx. This is the first case of sialolipoma in eustachian tube in the literature. Endoscopic removal is usually successful with uneventful short recovery period.
Similar content being viewed by others
Background
Unilateral otitis media with effusion is always an alarming entity of eustachian tube obstruction at the level of nasopharynx especially in adult sufferers. The differential diagnosis of a mass lesion in this area ranged from benign to more destructive malignant pathologies. Lipoma as a cause of Eustachian tube obstruction is an extremely rare entity. Muzzi et al., in his systematic review of primary tumors and tumor-like lesions of eustachian tube (ET), searched the literature from 1888 till 2011 with no single reported lipoma case [1]. We are reporting a case of ET lipoma presented with refractory otitis media with effusion (OME). This is an extremely rare location of such entity and to the best of our knowledge this is the third case reported in the world literature of ET lipoma after 2 cases published in 2011 and 2016 respectively [2, 3]. However, this is the first case reported in the literature of ET sialolipoma.
Case presentation
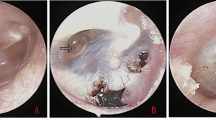
Our patient is a 27-year-old male who was roaming around between primary care facilities and otolaryngology specialists for few months before he showed up in our clinic. His main complaint was left severe ear block sensation associated with hearing loss and intermittent tinnitus. Conservative management with watchful waiting and intranasal corticosteroid sprays were offered to him outside our facility with no successful response. He also had one trial of office-based myringotomy without ventilation tube insertion with fast recurrence of symptoms. Clinical evaluation by otoscope revealed evidence of unilateral left otitis media with effusion. Rinne test showed bone conduction (BC) > air conduction (AC) in the left ear while air conduction (AC) > bone conduction (BC) in the right side. Weber test lateralized to the left ear. Endoscopic nasal examination using 0° rigid endoscope showed deviated nasal septum to the left with a polyp originating from the left ET orifice (Fig. 1A). Pure tone Audiogram with acoustic immittance showed moderate conductive hearing loss in the left ear with normal hearing threshold in the right side. Tympanometry showed type B flat curve in the left side while type A in the right side (Fig. 2A, B). Computed tomography (CT) scan and magnetic resonance imaging (MRI) were obtained to delineate the nature and extent of the pathology prior to any surgical intervention. Computed tomography (CT) scan and magnetic resonance imaging (MRI) were suggestive of benign lesion noted at the nasopharyngeal orifice of the ET measuring 10 × 8 mm with consequent left middle ear effusion. The most likely differential diagnosis was lipoma (Fig. 3A–F) A written consent was obtained from the patient before surgical intervention. The procedure was performed under general anesthesia via transnasal endoscopic approach. At the start of surgery, left myringotomy with insertion of a soft T-tube was performed. Then, because of the presence of evident left septal spur, endoscopic septoplasty was performed with removal of the bony-cartilaginous spur. To acquire a better exposure of the ET pharyngeal orifice, excision of the posterior bulky tail of the left inferior turbinate was done. The polyp was seen bulging and totally blocking the ET orifice. The polyp was grabbed and using sharp dissection complete excision of the polyp from its origin inside the ET was executed. Electrocautery was not used in the area of the ET orifice (Fig. 1A–D). After checking hemostasis, no nasal packing was used. The patient had uneventful postoperative recovery. Histopathology report confirmed the diagnosis of sialolipoma (Fig. 4A, B). T-tube was removed 3 months after the surgery. The choice of soft T-tube enabled easy and painless removal of the tube in the office. Complete healing of the tympanic membrane occurred within the next 2 weeks and patient reported total disappearance of symptoms. Follow-up extended for 3 years after the surgery with no recurrence of symptoms or any signs of effusion.
A Transnasal intraoperative view of a polyp-like lesion protruding through the left ET orifice measuring (1 × 1 × 0.5 cm). B View of the polyp after removing the bulky tail of the left inferior turbinate to improve exposure. C Grabbing the polyp during surgery visualizing its origin from inside the lumen of the ET. D After complete excision of the polyp and the ET orifice looks widely open
A Axial cut contrast-enhanced CT head and neck showing hypodense non-enhancing well circumscribed lesion measuring (1 × 1 × 0.5 cm) at the nasopharyngeal opening of left ET. B Reconstructed sagittal CT scan head and neck showing the lesion at the level of the left ET orifice protruding into the nasopharynx (arrow). C Axial T1-weighted MRI without contrast with fat suppression showing hypointense density, homogeneous to fat signal, lesion at the nasopharyngeal orifice of the ET. D Axial T2-weighted MRI without fat suppression showing the fluid signal in the left mastoid area suggesting severe middle ear effusion and the lesion showing hyperintense signal at the nasopharyngeal opening of the left ET (arrow). Notice the bulky tail of the inferior turbinate. E Coronal T1-weighted MRI without contrast without fat suppression showing hyperintense signal lesion at the nasopharyngeal opening of the left ET. F Sagittal T1-weighted MRI without contrast without fat suppression showing hyperintense signal lesion at the nasopharyngeal opening of the left ET protruding into the nasopharynx (arrow)
A Microscopic pictures of the received specimen reveals a fragment focally lined by pseudostratified ciliated columnar epithelium resting on a fibrous layer of variable thickness with mild inflammatory infiltrate. B Higher magnification showing the underlying tissue composed of well-circumscribed benign growth composed of mature adipocytes with intervening fibrovascular septae. Seromucous (salivary gland type) glands arranged in a lobule with surrounding delicate fibrosis and inflammatory infiltrates is seen at the periphery of the lesion. Pictures suggestive of sialolipoma
Discussion
Finding a tumor or a lesion mimicking tumors originating from eustachian tube (ET) area is extremely rare [1,2,3]. The symptoms arising from an obstruction at the level of ET range from unilateral ear pressure or fullness to the extreme of hearing loss and referred otalgia. Such presentation warrants a comprehensive head and neck clinical examination including nasal endoscopy. Imaging are very helpful in evaluation of any suspicious fullness or identified lesion in the same area. Furthermore, it can provide an important information about the nature and extent of such pathology. The primary pathology of isolated ET lesion might be benign like teratoma, dermoid, leiomyoma, chondroma, and lipoma, or a malignant entity such as squamous cell carcinoma, lymphoma, and sarcoma [1, 4]. Head and neck lipoma as an entity constitute about 13–17% of soft tissue tumors [5, 6]. The incidence of lipoma in ET area particularly is not reported in the literature [3]. Sialolipoma is a very rare variant of salivary gland lipomatous lesions characterized histologically by entrapment of ducts and acini originated from salivary gland tissues into adipocytes [7, 8]. Nagao et al. were the first to use the term “Sialolipoma” by reporting 7 cases in 2001 [9]. In 2009, Yang et al. reported that the mean age of sialolipoma is 52 years with equal ratio between both genders [10]. Our patient was only 27 years old when he presented to our clinic. The picture that he presented with is one that makes any otolaryngologist want to rule out a mass in the nasopharynx. This is because one should always stress and keep in mind that malignancy is to be ruled out in any adult patient with unilateral OME. The differential diagnosis in mind would be of an antro-choanal polyp, inverted papilloma, or nasopharyngeal carcinoma. It is unlikely to see a pathology originating inside the ET causing OME in daily clinical practice. Our clinical examination, however, revealed a polyp that was originating in the left ET explaining the symptoms of the patient. Hearing evaluation in the clinic by audiometry and tympanometry confirmed a conductive hearing loss supporting the clinical findings. Imaging modality of the choice in this case would be a high-resolution CT scan with contrast extending from base of skull to the thoracic inlet evaluating the nature and extent of the lesion. MRI scan can be of a great help as well in evaluating the soft tissue. The findings on the CT scan were suggestive of a localized smooth well circumscribed lesion in the left ET area with no bony erosion around it. This finding is usually suggestive of benign lesion. MRI supported the diagnosis of ET lipoma. Surgical excision is the management of such lesion. The ideal approach is endoscopic transnasal approach under general anesthesia. We were able to excise the lesion in-toto with minimal bleeding. Histopathology examination revealed the unusual rare variant of lipoma in the ET. The recovery was fast after the procedure and as originally anticipated, the T-tube was removed 3 months postoperative. The choice of soft T-tube made its office removal easier and painless compared to the standard grommet’s tube. Follow-up showed complete resolution of symptoms with no recurrence up to 3 years after the surgery.
Conclusions
Unilateral otitis media with effusion as a complaint in adult patient necessitate detailed and thorough clinical examination including rigid nasal endoscopy to rule-out lesions at the level of nasopharynx. This presentation should always raise concern of malignancy especially in older candidates. However, there are few reported cases of benign lesions in ET area. To the best of our knowledge, this is the first case of sialolipoma reported in this location originating from inside the ET orifice in the literature. Endoscopic removal of these lesions is usually successful and straight forward with uneventful short recovery period. One should keep this diagnosis in mind when evaluating an adult patient with such presentation.
Availability of data and materials
Not applicable for this manuscript.
Abbreviations
- ET:
-
Eustachian tube
- OME:
-
Otitis media with effusion
- AC:
-
Air conduction
- BC:
-
Bone conduction
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
References
Muzzi E, Cama E, Boscolo-Rizzo P, Trabalzini F, Arslan E (2012) Primary tumors and tumor-like lesions of the eustachian tube: a systematic review of an emerging entity. Eur Arch Otorhinolaryngol 269(7):1723–1732. https://doi.org/10.1007/s00405-011-1846-x
Dabiri J, Choufani G, Delpierre I, Hassid S (2016) A case of lipoma arising in the eustachian tube. Ear Nose Throat J 95(1):E5–E7. https://doi.org/10.1177/014556131609500102
Liu Z, Wang D, Liu Q (2011) The presence of a lipoma in the Eustachian tube: a case report. J Med Case Rep 5:436
Shim WS, Kim YS, Shin DK, Jung HJ (2020) A case of otitis media with effusion due to leiomyoma of the Eustachian tube. Braz J Otorhinolaryngol 86:S51–S54
Bree ED, Karatzanis A, Hunt JL, Strojan P, Rinaldo A, Takes RP, Ferlito A, Bree RD (2014) Lipomatous tumors of the hrad and neck: a spectrum of biological behavior. Eur Arch Otorhinolaryngol. https://doi.org/10.1007/s00405-014-3065-8
Aydin U, Asik MB, Karakoc O, Kurt B (2016) Uncommon variant of lipoma of eustachian tube as a cause of middle ear effusion. Gulhane Tip Derg 58:186–189
Subramaniam S, Johan S, Hayati F, Ng CY, Azizan N, Chuah JA, Mohamed I (2020) Giant submandibular sialolipoma masquerading as huge goiter: a case report. BMC Surg 20:130
Zahrani, A. A., Qannam, A., Al Sadhan, R., & Bello, I. O. (2021). Sialolipoma of the floor of the mouth with immunohistological analysis. Case Rep Dentistry, 2021, 6623045. https://doi.org/https://doi.org/10.1155/2021/6623045
Nagao T, Sugano I, Ishida Y et al (2001) Sialolipoma: a report of seven cases of a new variant of salivary gland lipoma. Histopathology 38(1):30–36
Jang YW, Kim SG, Pai H, Park JW, Lee YC, Rotaru H (2009) Sialolipoma: case report and review of 27 cases. Oral Maxillofacial Surg 13(2):109–113
Acknowledgements
Not applicable for this manuscript
Funding
Authors did not receive any funding for this work.
Author information
Authors and Affiliations
Contributions
KZ is the first author who contributed to the manuscript via collecting data, performing literature review and writing up the manuscript. MB is the senior author who supervised the whole scheme of work and revised the final manuscript before submission. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval is not applicable for this manuscript. A written informed consent was obtained from the patient to use his data in this manuscript.
Consent for publication
A written informed consent was obtained from the patient to publish his data including graphs and investigations images in this manuscript
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al Zaabi, K., Badr-El-Dine, M.M.K. Refractory otitis media with effusion due to eustachian tube sialolipoma inform consistent with eustachian tube inflammatory polyp: rare case presentation and literature review. Egypt J Otolaryngol 38, 29 (2022). https://doi.org/10.1186/s43163-022-00218-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00218-w