Abstract
Background
Lertal® is an oral food supplement containing 80 mg of dry extract of Perilla frutescens, 150 mg of bioflavonoid quercetin, and 5 μg of vitamin D3. The aim of this study was to evaluate the efficacy of Lertal® as a complementary therapy to topical therapy of patients with moderate-to-severe seasonal allergic rhinoconjunctivitis (SAR).
Results
Seventy (n=70) adult patients with moderate-to-severe SAR were included in this prospective study and treated by four different procedures: (1) 21 patients received azelastine intranasal spray for 30 days and, after that, azelastine spray and Lertal® tablets for the next 30 days; (2) 19 patients received combined azelastine with fluticasone intranasal spray for 30 days and azelastine with fluticasone spray and Lertal® tablets for the next 30 days; (3) 15 patients received azelastine spray only for 60 days; (4) 15 patients received combined azelastine with fluticasone spray only for 60 days. Levels of SAR symptoms (sneezing, tearing, ocular itching, rhinorrhea, nasal obstruction, hyposmia, and cough), as well as Total Symptom Scores (TSS), were evaluated at the start of this investigation (visit 0), after 30 days of treatment (visit 1), and after 60 days of treatment (visit 2) using a visual analog scale. After 30 days of treatment, better effects were achieved in groups in which patients were treated with combined (antihistamine with corticosteroid) spray. After 60 days of therapy, we found the best effects in procedure 2 and slightly worse effects in procedure 1. The high differences in the reduction of TSS between the 60th and 30th day were found for procedure 2 (p<0.001) and procedure 1 (p<0.001). The worse improvement of symptoms we found was in procedure 4 (p<0.01), and, for the procedure 3, we found no significant difference (p=0.140). None of the patients reported adverse effects during the therapy.
Conclusion
Our results suggest that addition of food supplement Lertal® to the standard topical therapy of patients with moderate-to-severe SAR increases the effects of intranasal therapy in reducing nasal and ocular symptoms.
Similar content being viewed by others
Background
Allergic rhinitis (AR) is a highly prevalent chronic inflammatory disorder affecting the mucosa of the nasal cavity and, frequently, of conjunctiva. So, the term “allergic rhinitis,” especially for the seasonal form of disease should be replaced with the term “allergic rhinoconjunctivitis”. The main symptoms of seasonal allergic rhinoconjunctivitis (SAR) are sneezing, ocular itching, tearing, rhinorrhea, and, less intensely, nasal obstruction, hyposmia, and cough. It is caused by an allergic response to pollen and other outdoor allergens [1]. SAR is a frequent chronic nasal inflammation with strong influence on quality of life due to the high level of association with asthma and chronic rhinosinusitis [2]. Diagnosis of AR can be done by the presence of specific symptoms, local findings, by allergy skin prick tests, and serological tests [2]. The prevalence of self-reported AR was estimated up to 25% in pediatric and up to 40% in adult population [1, 2]. Clinical practice guideline for AR management has improved the quality of patients’ care over the past 20 years. The ARIA guidelines were initiated in 2001 and updated in 2008. The ARIA 2010 revision was the first evidence-based guideline for the management of AR that followed the GRADE concept [2]. The ARIA 2014 revision was initiated to evaluate the rigor of development and quality of reporting of guidelines regarding the management of AR [2]. Finally, the 2016 revision of the ARIA guidelines provides both the most important updates and new recommendations regarding the medical therapy of AR [2]. The most important change in the ARIA 2008 guideline was the introduction of terms “intermittent” and “persistent” AR. However, previous investigations usually refer to SAR, usually caused by outdoor allergens and perennial AR (PAR), usually caused by indoor allergens (house dust mites, molds, animal dander, and others). Accordingly, ARIA 2016 revision retained and promoted the use of the terms SAR and PAR to enable the interpretation of published evidence. Therefore, the ARIA 2016 recommendations are more applicable to treatment of patients with moderate-to-severe AR and less applicable to therapy of patients with mild AR.
According to the revised ARIA 2016 guideline, the main treatment options for SAR include the use of second-line oral or intranasal antihistamines, intranasal corticosteroid sprays, leukotriene receptor antagonist, and, for the first time in the evidence-based guidelines, the use of combined intranasal antihistamine with corticosteroid sprays [2]. Several herbal compounds have been developed in the last decade for the treatment of acute and chronic upper airway inflammatory disorders. A new combined preparation in tablets has recently appeared for the complementary treatment of SAR. Lertal® is an oral food supplement containing 80 mg of dry extract of the Perilla frutescens seeds, a bioflavonoid quercetin (150 mg), and 5 μg (200 IU) of vitamin D3 [3,4,5,6]. This investigation was organized to evaluate the efficacy of Lertal® as a complementary therapy to standard intranasal therapy of patients with moderate-to-severe SAR.
Methods
Study design and participants
The adult participants suffering from SAR were included in this prospective, open-label study with analysis of data collected from five medical centers. This investigation was approved by the ethics committee of our university hospital (MMA 05/2019) and realized between March 1st and September 30th 2020, according to the Declaration of Helsinki. All the patients approved their participation in the study by informed consent.
Eighty patients (n = 80) with moderate-to-severe SAR were involved in the study. Seven (n = 7) refused to participate while three (n = 3) patients did not meet inclusion criteria. Seventy (n = 70) patients were thus recruited and assigned to one of four therapy procedures. We used a simple computer-generated randomization procedure to allocate the participants into different treatment regimens.
The inclusion criteria were age range 18–65 years and diagnosis of SAR, based on ARIA and AAO-HNS [2, 7]. The patients had symptoms (sneezing, tearing, ocular itching, rhinorrhea, nasal obstruction, hyposmia, and cough), rhinoscopic/endoscopic findings of AR, as well as sensitization to outdoor allergens. Only patients with moderate-to-severe SAR were included.
Exclusion criteria were the patients with mild SAR, PAR, chronic rhinosinusitis (CRS) with or without nasal polyps, bronchial asthma, aspirin sensitivity, and systemic diseases which affect the nasal cavity. Also, the patients with severe septal deformation, severe hypertrophy of the nasal conchae, acute respiratory tract infections, and with use of antihistamines and glucocorticoids within the 3 weeks before the start of this study were excluded.
Allergy determination
All participants were evaluated for allergies, according to the medical histories, complaints, skin-prick tests, and blood testing for total serum immunoglobulin E (IgE). Skin-prick tests were performed using commercial package of aeroallergens, including birch, cat, dog, horse, London planetree, mite, molds, mugwort, olive tree, ribwort plantain, spreading pellitory, and timothy (Soluprick, ALK-Abelló A/S, Hørsholm, Denmark). We included negative (0.9% sodium chloride) and positive (histamine dihydrochloride) controls for all tests. The test was considered positive if the diameter of the protrusion on the skin was greater than 3 mm relative to the control. For the measurement of IgE serum concentration on the ELISA reader (Spectra III, Austria), we used the human commercial ELISA kit (Elitech Diagnostics, Salon-de-Provence, France). The patients with total serum IgE levels higher than 100 IU/ml were considered as atopic.
Treatment
To evaluate the efficacy of Lertal® as a complementary treatment of SAR patients, we performed four different treatment procedures. The patients were informed about the therapy.
-
Procedure 1 (A–A+L): azelastine hydrochloride antihistamine (137 μg in a dose, 2 times/day) intranasal spray for 30 days and azelastine spray (137 μg in a dose, 2 times/day) and Lertal®, tablets, 2 times/day for the next 30 days.
-
Procedure 2 (A+C–A+C+L): combined azelastine hydrochloride antihistamine (137 μg in a dose) with fluticasone propionate corticosteroid (50 μg in a dose) intranasal spray, 2 times/day for 30 days, and combined azelastine with fluticasone spray, 2 times/day, and Lertal®, tablets, 2 times/day for the next 30 days.
-
Procedure 3 (A–A): azelastine hydrochloride (137 μg in a dose) spray only, 2 times/day for 60 days.
-
Procedure 4 (A+C–A+C): combined azelastine hydrochloride (137 μg in a dose) with fluticasone propionate (50 μg in a dose) spray only, 2 times/day for 60 days.
For each subject, the researchers checked the patency of the nasal cavity, as well as whether they were familiar with the proper use of the sprays.
Clinical evaluation
Levels of SAR symptoms (sneezing, tearing, ocular itching, rhinorrhea, nasal obstruction, hyposmia, and cough) were evaluated at the start of this investigation (visit 0), after 30 days of treatment (visit 1), and after 60 days of treatment (visit 2). Patients themselves assessed the intensity of their symptoms using a visual analog scale (VAS) (0–10 cm; from 0 = lack of symptoms to 10 = the highest intensity of symptoms). Previously, the proper use of VAS in patients was explained in detail. The patients noted the therapy use and the levels of complaints on their therapy cards, after the medication use. At visits 1 and 2, researchers evaluated the treatment compliance by insight into the cards. The severity of SAR was assessed according to Bousquet et al. [8] into “mild SAR” (VAS of 5 and under 5) and “moderate-to-severe SAR” (VAS of 6 and over 6).
The main endpoints for treatment efficacy were mean Total Symptom Score (TSS; sum of the all seven symptoms), as well as individual scores for each complaint at visits 0, 1, and 2.
We performed the monitoring of adverse events, potentially reported by patients. Previously, the patients were informed on possible side effects. Also, evaluation of vital signs and laboratory tests was organized during visits 1 and 2.
Statistical analysis
The parameters were presented as mean ± standard deviation. We used a Kruskal-Wallis test to compare the parameters between groups of participants. As we had more than two groups of patients, we continued the analysis by the Mann-Whitney U test. Dunn’s correction test was used for the assessment of the levels of statistical differences. For paired comparison within a group, Wilcoxon’s test was used. For calculation of relative changes for all clinical parameters, we used the formula: posttherapeutic value − pretherapeutic value/pretherapeutic value × 100. P values < 0.05 were considered significant. The analysis was performed by using the SPSS software, version 17.0 (IBM SPSS Statistic, Chicago, USA).
Results
Demographic data are presented in Table 1. In total, seventy (n=70) adult patients, aged from 18 to 65 years, with diagnosis of SAR were included. There were 38 male and 32 female participants with mean age of 39.4±12.4 years. In 21 patients, we performed procedure 1, in 19 procedure 2, in 15 procedure 3, and in 15 patients, we used procedure 4 of therapy.
The average symptom scores before (V0), after 30 days (V1), and after 60 days (V2) of therapy are presented in Table 2. At baseline, patients from all 4 treatment procedures were equalized according to the intensity of symptoms and the TSS. After 30 days of treatment, better effects were achieved in groups in which the patients were treated with combined (antihistamine with corticosteroid) spray. After 60 days of therapy, the best effects were achieved in procedure 2, where patients, in adition to the combined spray, also received Lertal®. Slightly worse effects were achieved in procedure 1, in which patients received Lertal® in addition to the intranasal antihistamine.
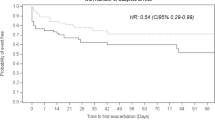
Numerical presentation of differences in the relative improvement in TSS (day 30 vs day 0; day 60 vs day 30) are presented in Table 3. Graphical presentation of the same parameters are presented in Fig. 1. The high differences were achieved for procedure 2 (p<0.001) and procedure 1 (p<0.001). The worse difference we found was in procedure 4 (p<0.01), and for procedure 3, we found no significant difference (p=0.140). Statistical significances of differences in the percents of improvement in nasal and ocular symptoms (V2 vs V1–V1 vs V0) are presented in Table 4. The addition of Lertal® to standard combined therapy (azelastine with fluticasone) significantly reduced the scores of all SAR symptoms. In patients who took only an antihistamine until the 30th day, after the addition of Lertal®, there was a significant improvement in all symptoms, except hyposmia. In patients who were only on antihistamine therapy, on day 60, there were significant improvements only for sneezing, nasal obstruction, hyposmia, and cough. In patients on combined antihistamine with corticosteroid therapy only, on day 60, there were significant improvements for sneezing, tearing, ocular itching, rhinorrhea, nasal obstruction, and cough. None of the participants reported adverse effects during the therapy.
Discussion
Antihistamines are frequently prescribed in patients suffering from SAR as they are effective and quickly relieve symptoms. Previous investigations showed that topical antihistamine azelastine hydrochloride reduces the intensity of AR symptoms faster and more effectively than most oral antihistamines [9]. This drug is thought to be as effective in supressing immune-mediated inflammation as neurogenic inflammation in AR [9]. A major step forward in the treatment of AR is the development of a combined preparation of azelastine hydrochloride and fluticasone propionate (MP29-02) in a nasal spray. Studies have shown significantly better effects of this preparation in the treatment of moderate-to-severe AR in comparison to the effects of therapy with azelastine spray and fluticasone spray, separately [10,11,12].
However, in cases of intense allergen exposure, both intranasal antistamine and corticosteroid may be unable to completely inhibit allergic inflammation, resulting to the necessity for the use of additional therapy. Lertal® is a combined preparation, formulated in bilayer tablets containing the extract of Perilla frutescens (80 mg), quercetin (150 mg), and vitamin D3 (5 μg). It consists of a fast-releasing layer that enables fast antihistaminic action of Perilla frutescens, and a slow-releasing layer containing quercetin and vitamin D3, which provides high bioavailability and prolonged anti-allergic effect of these substances [3,4,5,6]. The dry extract of Perilla frutescens seeds contains rosmarinic acid and bioflavonoids, such as luteolin, chrysoeriol and apigenin, and all of these compounds have well-documented immunomodulatory and anti-allergic activities. They suppress the release of histamine, decrease the expression of pro-inflammatory cytokine interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), and increase the expression of interferon-gamma (IFN-γ) [13]. The extract of Perilla also has strong inhibitory activity against both 5-lipoxygenase and 12-lipoxygenase, the most important enzymes in allergic inflammation [13]. Quercetin is a bioflavonoid with a strong antioxidant activity found in grapefruit, onions, apples, green vegetables, and beans. It has an affinity for binding to the cell membranes of mast cells and basophils, tending to stabilize their membranes and block degranulation and release of histamine, leukotrienes, as well as IL-6, IL-8, and TNF-α [3,4,5,6]. Quercetin significantly increases transepithelial chloride ion transport to the nasal secretions, enhances the ciliary beat frequency, and stimulates the mucociliary clearance [14]. Vitamin D3 is an important factor for the normal function of the immune system. It has been reported that vitamin D3 serum level is inversely correlated with levels of cytokines IL-6 and IL-10 [15]. Vitamin D3 decreases the expression of the major histocompatibility complex (MHC) class 2 molecule on the membrane of antigen-presenting cells [15]. Finally, it has been demonstrated higher incidence for AR and CRS morbidity in patients with lower serum levels of vitamin D3 [16]. So, addition of vitamin D3 can be considered as an adjuvant therapy against allergic inflammations in the airways.
Previous investigations demonstrated a very good action of Lertal® in the reduction of nasal and/or ocular complaints of SAR [3,4,5]. Use of Lertal® as a complementary therapy reduces the use of antihistamines in children and adult patients with SAR [3,4,5]. Marseglia et al. [6] found that Lertal® assumption for the long-time was without side effects in children. This supplement significantly reduces the risk of exacerbation of SAR symptoms, duration of symptoms, and the need for symptomatic medications in children with SAR [6]. No adverse events of Lertal® were noted in the previous studies, in both adult and pediatric patients.
Our results showed better effects of the first 30-day therapy in adult patients treated with combined (antihistamine with corticosteroid) spray. After the next 30 days of therapy, the best effects were achieved in regimen where patients received Lertal® in adition to the combined antihistamine-corticosteroid spray. Slightly worse effects were achieved in procedure where patients received Lertal® in addition to the intranasal antihistamine. Therefore, according to our results, supplementation of Lertal® to the standard azelastine with fluticasone therapy decreases the TSS for about 37% in comparison to the status before the Lertal® addition. Slightly worse decrease in the TSS, about 30%, was achieved when we added Lertal® to the intranasal antihistamine treatment. When we continued with standard therapy of AR (procedures 3 and 4), after 60 days, an improvement of about 10% occured in group treated by combined antihistamine with corticosteroid spray. This finding could suggest the presence of a cumulative effect of long-term combined azelastine with fluticasone therapy. The addition of Lertal® to standard combined therapy (azelastine with fluticasone) significantly reduces the scores of all SAR symptoms. In patients who took only an antihistamine until the 30th day, after the addition of Lertal®, there is a significant improvement in all symptoms, except hyposmia. Therefore, according to our results (Table 4), reduction in nasal obstruction is better in patients who used Lertal® with combined intranasal antihistamine and corticosteroid spray. This finding suggests the presence of synergistic anti-edematous and anti-inflammatory effects of corticosteroid fluticasone-propionate, antihistamine azelastine hydrochloride, and Lertal®. So, the reduction of edema and inflammation in the olfactory cleft is better in patients who added Lertal® to topical antihistamine with corticosteroid therapy, resulting in the improvement of the sense of smell. Previous investigations suggested that Lertal potentiates the antiallergic effects of antihistamines [3,4,5,6]. Our results suggest that Lertal® potentiates the anti-inflammatory, antiallergic and immunomodulatory effects of both antihistamines and corticosteroids and, accordingly, reduces the nasal and ocular symptoms of SAR.
The present study has limitations because the number of patients was relatively small. The assessment of the intensity of nasal and ocular symptoms depended on the subjective experience that the patients had, and not on the objective parameters. In our study, we did not strictly follow the ARIA 2016 and AAO-HNS 2015 guidelines for the therapy of AR, as we treated one number of patients with moderate-to-severe SAR with azelastine hydrochloride spray alone or in combination with Lertal®. Both guidelines recommend the use of combined azelastine with fluticasone spray as one of the main treatment options in therapy of moderate-to-severe SAR [2, 7]. During the designation of our study, we took into account the fact that some patients with AR cannot use intranasal corticosteroid therapy due to recent nasal problems (injury, ulcers, surgery), infections (tuberculosis, herpes nose, and eye infection), certain eye problems (glaucoma, cataract), arterial hypertension, and liver disease. We wanted to show that combined therapy with intranasal azelastine and Lertal® can also be very effective in reducing the symptoms of moderate-to-severe SAR and that this treatment regimen could be a good alternative to standard therapy in patients with those comorbidities.
Conclusion
In this study, we proposed two options for successful therapy of SAR: intranasal antihistamine azelastine with addition of herbal compound Lertal® and combined azelastine with fluticasone spray with addition of Lertal®. Our results suggest that addition of food supplement Lertal® to the standard topical therapy of patients with moderate-to-severe SAR increases the effects of intranasal therapy in reducing nasal and ocular symptoms. The addition of Lertal® to intranasal azelastine is especially important in patients with moderate-to-severe SAR who cannot use intranasal corticosteroid therapy due to the presence of comorbidities. Food supplements will play an important role in the future treatment of AR, but their use cannot be separated from the objective confirmation of their efficacy and safety.
Availability of data and materials
The details used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AR:
-
Allergic rhinitis
- ARIA:
-
Allergic Rhinitis and its Impact on Asthma
- AAO-HNS:
-
American Academy of Otolaryngology–Head and Neck Surgery Foundation
- GRADE:
-
Grading of Recommendations, Assessment, Development, and Evaluation
- SAR:
-
Seasonal allergic rhinoconjunctivitis
- PAR:
-
Perennial allergic rhinitis
- CRS:
-
Chronic rhinosinusitis
- ELISA:
-
Enzyme-linked immunosorbent assay
- VAS:
-
Visual analog score
- TSS:
-
Total symptom score
- A–A+L:
-
Antihistamine–antihistamine+Lertal®
- A+C–A+C+L:
-
Antihistamine+corticosteroid–antihistamine+corticosteroid+Lertal®
References
Zittoon RF, Ahmed DI, Iskander NM, Madian YT (2021) Allergic rhinitis patients associated with migraine: effect of treatment of allergic rhinitis on migrainous attack. Egypt J Otolaryngol 37(1):14. https://doi.org/10.1186/s43163-021-00077-x
Brožek JL, Bousquet J, Agache I, Agrawal A, Bachert C, Bosnic-Anticevich S et al (2016) Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines – 2016 revision. J Allergy Clin Immunol 140:950–958
Ariano R (2015) Efficacy of a novel food supplement in the relief of the signs and symptoms of seasonal allergic rhinitis and in the reduction of the consumption of anti-allergic drugs. Acta Biomed 86(1):53–58
Marseglia G, Licari A, Ciprandi G (2020) Complementary treatment of allergic rhinoconjunctivitis: the role of the nutraceutical Lertal®. Acta Biomed 91(1):97–106. https://doi.org/10.23750/abm.v91i1.9275
Tosca MA, Olcese R, Marinelli G, Papale M, Zicari AM, Marseglia G, Ciprandi G (2020) Lertal®, a multicomponent nutraceutical, could reduce the use of antihistamines in children with allergic rhinitis. Acta Biomed 91(2):356–359. https://doi.org/10.23750/abm.v91i2.9719
Marseglia G, Licari A, Leonardi S, Papale M, Zicari AM, Schiavi L et al (2019) A polycentric, randomized, parallel-group, study on Lertal®, a multicomponent nutraceutical, as preventive treatment in children with allergic rhinoconjunctivitis: phase II. Ital J Pediatr 45(1):84. https://doi.org/10.1186/s13052-019-0678-y
Seidman MD, Gurgel RK, Lin SY, Schwartz SR, Baroody FM, Bonner JR, Dawson DE, Dykewicz MS, Hackell JM, Han JK, Ishman SL, Krouse HJ, Malekzadeh S, Mims JW, Omole FS, Reddy WD, Wallace DV, Walsh SA, Warren BE, Wilson MN, Nnacheta LC, Guideline Otolaryngology Development Group. AAO-HNSF (2015) Clinical practice guideline: allergic rhinitis. Otolaryngol Head Neck Surg 152(1S):S1–S43. https://doi.org/10.1177/0194599814561600
Bousquet PJ, Combescure C, Neukirch F, Klossek JM, Méchin H, Daures JP, Bousquet J (2007) Visual analogue scales can assess the severity of rhinitis graded according to ARIA guidelines. Allergy 62(4):367–372. https://doi.org/10.1111/j.1398-9995.2006.01276.x
Lieberman PL, Settipane RA (2003) Azelastine nasal spray: a review of pharmacology and clinical efficacy in allergic and nonallergic rhinitis. Allergy Asthma Proc 24(2):95–105
Carr W, Bernstein J, Lieberman P, Meltzer E, Bachert C, Price D et al (2012) A novel intranasal therapy of azelastine with fluticasone for the treatment of allergic rhinitis. J Allergy Clin Immunol 129:1282–1289.e10
Kortekaas Krohn I, Callebaut I, Alpizar YA, Steelant B, Van Gerven L, Skov PS et al (2018) MP29-02 reduces nasal hyperreactivity and nasal mediators in patients with house dust mite allergic rhinitis. Allergy 73(5):1084–1093. https://doi.org/10.1111/all.13349
Price D, Shah S, Bhatia S, Bachert C, Berger W, Bousquet J, Carr W, Hellings P, Munzel U, Scadding G, Lieberman P (2013) A new therapy (MP29-02) is effective for the long-term treatment of chronic rhinitis. J Investig Allergol Clin Immunol 23(7):495–503
Takano H, Osakabe N, Sanbongi C, Yanagisawa R, Inoue K, Yasuda A, Natsume M, Baba S, Ichiishi EI, Yoshikawa T (2004) Extract of Perilla frutescens enriched for rosmarinic acid, polyphenolic phytochemical, inhibits seasonal allergic rhinoconjunctivitis in humans. Exp Biol Med 229(3):247–254. https://doi.org/10.1177/153537020422900305
Zhang S, Smith N, Schuster D, Azbell C, Sorscher EJ, Rowe SM, Woodworth BA (2011) Quercetin increases cystic fibrosis transmembrane conductance regulator-mediated chloride transport and ciliary beat frequency: therapeutic implications for chronic rhinosinusitis. Am J Rhinol Allergy 25(5):307–312. https://doi.org/10.2500/ajra.2011.25.3643
Bartley J (2010) Vitamin D, innate immunity and upper respiratory tract infections. J Laryngol Otol 124(5):465–469. https://doi.org/10.1017/S0022215109992684
Stokes PJ, Rimmer J (2016) The relationship between serum vitamin D and chronic rhinosinusitis: a systematic review. Am J Rhinol Allergy 30(1):23–28. https://doi.org/10.2500/ajra.2016.30.4267
Acknowledgements
This investigation was conducted as a part of scientific project of the Military Medical Academy Faculty of Medicine, Belgrade, Serbia (MFVMA 02 /19-21/).
Funding
None.
Author information
Authors and Affiliations
Contributions
AP, MBČ, VN, and NL analyzed and interpreted the patients’ data regarding rhinological examination and scoring system. AP, MBČ, MKV, VGD, and VN collected the data, followed up patients, and printed the results. AP and NL analyzed the statistical section. AP performed discussion and wrote the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics committee approval was received for this study from the Ethics Committee of the Military Medical Academy, Belgrade, Serbia (MMA No 05/2019) on May 13, 2019. Written consent was obtained from all study participants, and all participants included in the study have been informed about the procedures to be done and the expected results.
Consent for publication
Written consent for study publication was obtained from all study participants.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Perić, A., Čupić, M.B., Vuković, M.K. et al. Efficacy of a food supplement Lertal® as an adjuvant therapy of patients with moderate-to-severe seasonal allergic rhinoconjunctivitis. Egypt J Otolaryngol 37, 54 (2021). https://doi.org/10.1186/s43163-021-00117-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-021-00117-6