Abstract
Background
Vertigo and dizziness are very common complaints that may be related to epilepsy. The purpose of this study was to assess vestibulo-spinal and linear vestibulo-ocular function in epileptic patients in the inter ictal period. The current observational study was carried out in audio-vestibular unit Menoufia University. Subjects in the current study were divided into two groups: The control group included 30 normal individuals not complaining from any dizzy symptoms and the epileptic cases group included 30 epileptic patients. All subjects in the study were submitted to cervical and ocular vestibular evoked myogenic potential.
Results
There was no significant difference between the control and epileptic group regarding the age and sex distribution. Sixty-seven percent of epileptic cases had dizzy symptoms. There was statistically significant difference in the latency and amplitude of c and o VEMP between the control and the epileptic group, 39/60 ears (65%) in the study group had cVEMP abnormalities, 32/60 ears (53%) had oVEMP abnormalities. Abnormal c and o VEMP were reported in 28/60 ears (46.7%). There was statistically significant relationship between VEMP abnormalities and duration of seizures, frequency of epileptic attacks, and type of therapy.
Conclusion
Vestibular abnormalities were frequently reported in epileptic patients in the current study which may be related to the severity and control of epilepsy.
Similar content being viewed by others
Background
Epilepsy is a brain dysfunction characterized by recurrent disturbances in the normal electrical activity of the brain that results in seizures [1]. Vertigo and dizziness are very common complaints that occur either due to peripheral vestibular or central nervous causes. Among the latter, epilepsy should be taken into consideration [2]. Vestibular symptoms are common accompanying symptoms in seizure but it is rare to be the sole symptoms [3]. If vestibular symptoms occurred predominantly in seizure, this condition is called vestibular epilepsy, vestibulogenic seizure epileptic vertigo, and vertiginous epilepsy [4].
Vestibular evoked myogenic potentials (VEMP) is a short latency electromyographic response to sound stimuli that is used to assess ipsilateral saccular and inferior vestibular nerve functions (cervical: c VEMP), as well as contralateral utricular and superior vestibular nerve functions (ocular: o VEMP) [5].
VEMP also reflect functions of the central otolithic pathways and can be applied for the diagnosis of central nervous system disorders [6].
Many studies previously assessed the semicircular canals (SCCs) and vestibulo ocular function in these patients, but to our knowledge no studies assessed vestibulo spinal and otolith function in those patients. So, this study aimed at assessment of vestibulo spinal and linear vestibule-ocular functions in epileptic patients using c and o VEMP in the inter ictal period.
Methods
The current observational study was carried out in audio-vestibular unit (tertiary referral center), ENT department from April 2019 to May 2020.
Ethical approval from the hospital committee (according to Helsinki Declaration) and written consent from all the patients were obtained. Epileptic patients were recruited from outpatient neurology clinic.
Subjects in the current study were divided into two groups:
Control group
Included 30 normal individuals not complaining from any dizzy symptoms with age range between 20 and 40 years.
Cases group
Included 30 subjects with confirmed diagnosis of epilepsy through neurology specialist according to the criteria of international league against epilepsy (7), with age range between 20 and 40 years with exclusion of patients suffering from other neurological disorders, systemic diseases, history of otovestibular disorder, e.g., Meniere’s disease, conductive hearing loss, and cervical spine problems.
Equipment
The following equipment was used; two channel audiometer model (Madsen, orbiter 922), middle ear analyzer (Interacoustic AT235), and vestibular evoked myogenic potential (Eclipse/EP25 system, Interacoustics Inc., Middlefart, Denmark).
Methods
All subjects in the study group were submitted to full history taking (duration and frequency of epileptic attack, treatment, and audiovestibular symptoms), neurological examination, otoscopic, and basic audiological evaluation in the form of pure tone audiometry in the frequency range of 250 to 8000 HZ for air conduction and 500-4000 Hz for bone conduction, speech reception threshold (SRT), word discrimination score (WD) [7], and immittancemetry to exclude conductive hearing loss before VEMP testing.
VEMP
Electrode montage
The skin was cleaned carefully to ensure impedance less than 5kohm. For cVEMP, active surface electrode was placed on the upper half of sternocleidomastoid muscle (SCM) of the stimulated side, the reference electrodes were placed over mastoid bone ipsilateral to stimulation side. For oVEMP, active electrodes were placed on the face just inferior to eye contralateral to the stimulated side, reference electrodes were placed 2-3 cm below active electrode, and the ground electrode was placed on the forehead for c and o VEMP.
Instruction to the patient
For cVEMP, the subjects were asked to turn their head to the opposite side of recording with slight head flexion approximately 30 degrees to contract the SCM. For oVEMP, the subject was asked to look upward at distant target in the midline and the patient eye position was kept at a vertical visual angle of approximately 30-35° above horizontal.
Stimulus and recording parameters
Two hundred sweeps of 500 Hz tone burst (2:1:2 cycle) were delivered to the subjects via insert earphones at a rate of 5.1 Hz and intensity of 95 dBnHL. The filter was adjusted to be 10-750 Hz at a time window: −20 to 80 ms.
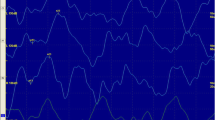
Wave analysis
The equipment system was monitoring the electromyography (EMG) levels throughout the testing. EMG scaling was done to compensate for the uneven contraction of SCM that may occur in both sides to allow for more accurate comparison between the individual right and left VEMP response. For all the recorded traces (in c and o VEMPs), the positive and negative peaks were identified according to their latencies followed by measuring of base to peak rectified amplitude of each wave. At least two traces were taken to ensure wave reproducibility.
Interaural amplitude ratio was also calculated for each type of VEMPs recording. The AR (asymmetry ratio) value was calculated as follows: (Amplitude of unaffected side − Amplitude of affected side/(Amplitude of un affected side + Amplitude of affected side) × 100, ratio more than 34% was considered pathological [8].
Statistical analysis
Results were analyzed using SPSS statistical package version 20. Two types of statistics were done: descriptive statistics, e.g., number (no.), percent (%) for qualitative data, mean (x), and standard deviation (SD) for quantitative data. Analytic statistics, comparison between quantitative data in two groups was done using Student’s t test (parametric test) and Mann-Whitney test (non-parametric test). Chi-squared test (χ2) was used to study association between two qualitative variables. P value of <0.05 was considered statistically significant.
Results
There was no significant difference between the control and study groups regarding the age and sex distribution (Table 1).
Audiovestibular symptoms
Vestibular symptoms were evident in 20/30 patients (67%), 11/30 (37%) of epileptic cases had imbalance (3 cases had sense of imbalance as an aura symptom and 8 cases had imbalance which was represented on starting administration of antiepileptic drugs). 9/30 (30%) of cases had vertigo that occurred spontaneously as aura symptoms in 4 patients and was related to starting administration antiepileptic therapy in 5 patients. Aural fullness was reported in 2 patients. The mean duration of seizures was 12.33±4.30 min. Frequency of attacks was as follows: one attack per week in 12/30 cases (40%), once per month in 11/30 cases (37%), and more than once per month in 7/30 cases (23%). 17/30 cases (57%) received only one drug and 13/30 cases (43%) received more than one drug. All subjects in the control and study groups had normal otoscopic examination, pure tone audiometry, speech discrimination, tympanometry and neurological assessment. VEMP Results: results of the amplitude or the latency beyond mean ± 2 SD of the normal values for the same age group in our laboratory were considered abnormal. All subjects in the control group had normal c and o VEMP results. There was statistically significant difference in the latency and amplitude of c and o VEMP between the control group and the study group (Table 2).
The current study showed that 39/60 ears (65%) in the study group had cVEMP abnormalities either prolonged latencies in 22/60 ears (37%), high amplitude in 28/60 ears (47%), low amplitude in 9/60 ears (15%), and amplitude asymmetry in 5/30 patient (17%). In oVEMP, 32/60 ears (53%) had abnormalities either prolonged latency in 19/60 ears (32%), high amplitude 14/60 ears (23%), low amplitude in 3/60 ears (5%), and amplitude asymmetry in 3/60 ears (10%). Abnormal c and o VEMP was reported in 28/60 ears (46.7%). All patients with vestibular symptoms had also abnormal VEMP results either ocular or cervical potentials. There was no statistically significant relationship between c and o VEMP abnormalities and age, gender (p > 0.05). Table 3 demonstrates relationship between abnormal VEMP results and duration of seizure, frequency of attacks, and type of therapy among the epileptic cases.
Discussion
Vestibular symptoms in epileptic patients may occur as an aura symptom or as a side effect of anti-epileptic drugs (AEDs) or may be related to a second comorbid disease (e.g., migranous vertigo) [9]. Focal intermittent epileptic discharge may cause episodic vestibular symptoms which are called epileptic vertigo [10]. Cortical stimulation of the vestibular cortex, e.g., superior lip of intraparietal sulcus may be the cause of epileptic vertigo [11]. Vertigo which may occur as aura symptoms reflects central vestibular dysfunction due to epilepsy [12]. AEDs modulate the activity of cerebral neurons so dizziness may occur as side effect of these drugs [13]. Dizziness is one of the most frequently reported side effects of AEDs [14].
The vestibular system consists of SCCs and otoloith organs (Utricle and Saccule) that respond to angular and linear velocity changes. The VOR is a reflex that generates eye movement matching the head movement; the angular VOR receives sensory input from the SCCs and compensate for rotation, the linear VOR receives sensory input from the otolith and compensate for translation. The vestibular spinal reflex (VSR) also receives otolith input, in response to linear motion changes [15]. The current study assessed the vestibulospinal function using cVEMP and linear VOR using oVEMP in epileptic patients. VEMP are useful tools in detecting central vestibular dysfunction when combined with oculomotor test of the VNG [16].
The auditory symptoms as hearing impairment and tinnitus may be reported as side effects of AEDs [17]. But in the current study, most of patients had no auditory complaints. Epilepsy can be controlled by one drug or combination of many drugs however one drug is preferred, if it fails, it is replaced by another one. If the second drug fail to control the seizures, another drug is added [18]. In the current study, more than half of the patients receive only one drug for management of epilepsy.
Hamed [19] reported that vestibular manifestations, including dizziness (62.22%) and sense of imbalance (44.44%) are frequent in patients with epilepsy, (24.44%) suffering from central vestibular dysfunction, 9 (20%) suffering from combined vestibular dysfunction and one (2.22%) had peripheral vestibular dysfunction. Gandelman-Marton et al. [20] also reported that dizziness and unsteadiness are common complaints in epilepsy patients. Also, epileptic patients may experience attacks of benign paroxysmal positional vertigo (BPPV) [21]. Fohner et al. [18] reported that long-term treatment with some antiepileptic drugs (AEDs) may cause dizziness, ataxia, imbalance, nystagmus, abnormalities in oculomotor functions, and their study revealed delayed conduction within auditory pathway (cochlea, auditory nerve, and brainstem) evidenced by abnormalities in the auditory brainstem response and nystagmography recordings indicating central and/or peripheral vestibular dysfunctions. In the current study, the vestibular symptoms (imbalance or vertigo) were reported in more than two-thirds of the epileptic cases, these symptoms may be related to the attack itself or starting the administration of AEDs.
VEMP responses are not only affected by peripheral vestibular end-organ dysfunction or vestibular nerve pathology but also can be affected by central neurological disorders [6]. The otolith organs are cortically represented in both hemispheres. The input from the SCCs and the otolith is converged at the vestibular nuclei within the brain stem and integrated through the vestibular cortical areas [16]. Lesions affecting the vestibular nuclei can cause abnormalities of both c and o VEMPs [16]. Abnormal ocular and cervical VEMP (which reflects vestibular affection in epilepsy) was reported in near than half of the epileptic patients in the current study.
Sixty-five percent of the ears in the epileptic group had abnormal cVEMP either prolonged latency (36.7%), high amplitude (46.7%), and low amplitude (15%). Prolonged latencies are signs of central disorders [22]. Also brainstem lesions, especially those in the vestibulospinal tract may cause prolongation of p13 [23]. Some studies have shown that brainstem involvement in epilepsy is related to generalized seizures; however, it is possible to have focal epilepsy with brainstem disorders [24, 25]. The effect of epilepsy on brain stem and vestibulo-spinal tract may be because of demyelination [26]. Slinger et al. [27] reported significant white mater changes in corticospinal tract, vestibulo-spinal tract in epilepsy. The AEDs may cause vestibular abnormalities through the delayed conduction in the brain stem pathway due to inhibitory GABA neurotransmitter and channel blockage which interfere with the firing of CNS neurons [28]. So, brain stem involvement and vestibulospinal tract affection may be the cause of abnormalities in cVEMP in the current study.
VOR is processed via the brain stem and cortical vestibular circuits especially parietal-vestibular nuclei circuits. Cortical control of the VOR has been demonstrated in electrical stimulation and behavioral studies, additionally cortical disorders affect the vestibulo-ocular function [29]. So, cortical stimulation of the vestibular cortex in epilepsy may interfere with VOR. Fifty-three percent of the ears, in the epileptic group in this study, had abnormal oVEMP either prolonged latency (31.7%), high amplitude (23.3%), and low amplitude (5%). oVEMP reflects the function of the vestibular nuclei and the crossed VOR circuits in the medial longitudinal fasciculus (MLF) [16]. Brainstem disorders that may occur in epilepsy can affect the VOR due to involvement of the vestibular nucleus, nucleus prepositus hypoglossi [30]. MLF can be responsible for the fast-epileptic propagation to lateral temporal area, reported audiovestibular symptoms like tinnitus; dizziness can be due to the epileptic spread to the superior temporal gyrus through the MLF fibers [30]. Lesions involving MLF can present abnormalities of both c and oVEMPs [16].
In the current study, high amplitude of o and c VEMP response was frequently reported finding which represent vestibular hyperexcitability and hyperactive response from the otolith organs, The AEDs have side effects on the vestibular system, AED therapy for long time may cause vestibular symptoms due to central or peripheral vestibular affection [28].
Abnormal vestibular function among epileptic patients may be also attributed to the presence of a common cerebral disorder responsible for both seizures and vestibular dysfunction [31]. Gandelman-Marton et al. [20] evaluated balance function in epileptic patients (generalized tonic clonic seizure) using computerized dynamic platform posturography (CDPP) and revealed poorer Sway Index (SI) in the epileptic patients than the controls. Also, El-Gohary et al. [13] assessed vestibular functions in epileptic patients using videonystagmography (VNG); they reported abnormal saccadic testing, central vestibular affection with focal EEG activity, and peripheral vestibular affection with generalized EEG activity.
In the current study, there was no significant statistical relationship between VEMP abnormalities (ocular and cervical) and age, gender among the epileptic cases, but these abnormalities were increased with higher frequency of the seizure as frequent attacks may represent lack of control of the disease with associated increase in the vestibular abnormalities (Table 3). There was significant statistical relationship between VEMP abnormalities and the duration of seizure, the increase in seizure duration is related to the severity of the disease (Table 3) [32]. So, vestibular abnormalities may be related to the severity of the disease.
Co-administration of two or more AEDs may cause adverse effects like dizziness through blockage of sodium channels [33]. These side effects depend on the type and the dose of the drugs [15]. In the current study, the vestibular abnormalities were more in patients who received polytherapy than who received monotherapy (Table 3). This may be due to more side effects reported in polytherapy than monotherapy. Further studies should be conducted on the relation between vestibular dysfunction and different types and doses of AEDs, also studies comparing oculmotor test and VEMP to detect which is more sensitive in detecting central vestibular dysfunction.
The authors concluded that abnormal VEMP results (which reflect vestibular affection in epilepsy) were frequently reported in epileptic patients which may be interpreted by the effect of epilepsy on vestibular cortex and brainstem or as adverse effects of antiepileptic drugs. Vestibular abnormalities may be related to the severity and control of epilepsy.
Conclusion
Our study concluded that vestibular abnormalities were frequently reported in epileptic patients in the current study which may be related to the severity and control of epilepsy.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- VEMP:
-
Vestibular evoked myogenic potentials
- SCCs:
-
Semicircular canals
- SCM:
-
Sternocleidomastoid muscle
- EMG:
-
Electromyography
- AR:
-
Asymmetry ratio
- AEDs:
-
Anti-epileptic drugs
- VSR:
-
Vestibular spinal reflex
- MLF:
-
Medial longitudinal fasciculus
References
Kobau R, Zahran H, Thurman DJ et al (2008) Epilepsy surveillance among adults--19 States, Behavioral Risk Factor Surveillance System, 2005. MMWR Surveill Summ 57:1–20
Morano A, Carnì M, Casciato S, Vaudano AE, Fattouch J, Fanella M, Albini M, Basili LM, Lucignani G, Scapeccia M, Tomassi R, di Castro E, Colonnese C, Giallonardo AT, di Bonaventura C (2017) Ictal EEG/fMRI study of vertiginous seizures. Epilepsy Behav 68:51–56. https://doi.org/10.1016/j.yebeh.2016.12.031
Berkovic SF, Crompton DE (2010) The borderland of epilepsy: a clinical and molecular view, 100 years on. Epilepsia 51(Suppl 1):3–4. https://doi.org/10.1111/j.1528-1167.2009.02432.x
Nielsen JM (1959) Tornado epilepsy simulating Meniere’s syndrome: report of 4 cases. Neurology 9(11):794–796. https://doi.org/10.1212/wnl.9.11.794
Colebatch JG, Rosengren SM, Welgampola MS (2016) Vestibular-evoked myogenic potentials. Handb Clin Neurol 137:133–155. https://doi.org/10.1016/b978-0-444-63437-5.00010-8
Venhovens J, Meulstee J, Verhagen WIM (2016) Vestibular evoked myogenic potentials (VEMPs) in central neurological disorders. Clin Neurophysiol 127(1):40–49. https://doi.org/10.1016/j.clinph.2014.12.021
Soliman S (1985) Speech discrimination audiometry using Arabic phonetically balanced words. Ain Shams Med J 27:27–30
Fisher RS, Cross JH, French JA, Higurashi N, Hirsch E, Jansen FE, Lagae L, Moshé SL, Peltola J, Roulet Perez E, Scheffer IE, Zuberi SM (2017) Operational classification of seizure types by the International League Against Epilepsy: position paper of the ILAE Commission for Classification and Terminology. Epilepsia 58(4):522–530. https://doi.org/10.1111/epi.13670
Murofushi T, Kaga K (2009) Vestibular evoked myogenic potential: its basics and clinical applications. Springer Science & Business Media. https://doi.org/10.1007/978-4-431-85908-6
Tarnutzer AA, Lee SH, Robinson KA, Kaplan PW, Newman-Toker DE (2015) Clinical and electrographic findings in epileptic vertigo and dizziness: a systematic review. Neurology 84(15):1595–1604. https://doi.org/10.1212/wnl.0000000000001474
Bisdorff A, Andrée C, Vaillant M, Sándor PS (2010) Headache-associated dizziness in a headache population: prevalence and impact. Cephalalgia 30(7):815–820. https://doi.org/10.1177/0333102409353617
Wiest G, Zimprich F, Prayer D, Czech T, Serles W, Baumgartner C (2004) Vestibular processing in human paramedian precuneus as shown by electrical cortical stimulation. Neurology 62(3):473–475. https://doi.org/10.1212/01.wnl.0000106948.17561.55
El-Gohary M, Elmously M, Esmail N et al (2014) Videonystagmography findings in epileptic children. Adv Arab Acad Audio-Vestibul J 1:26
Salas-Puig J, Serratosa JM, Viteri C, Gil-Nágel-Rein A, del Estudio SKATE GE (2004) Safety of levetiracetam as adjunctive therapy in epilepsy: the SKATE trial in Spain. Rev Neurol 38(12):1117–1122
Perucca P, Gilliam FG (2012) Adverse effects of antiepileptic drugs. Lancet Neurol 11(9):792–802. https://doi.org/10.1016/s1474-4422(12)70153-9
Iversen M, Zhu H, Zhou W et al (2018) Sound abnormally stimulates the vestibular system in canal dehiscence syndrome by generating pathological fluid-mechanical waves. Sci Rep 8:1–12
Oh SY, Kim HJ, Kim JS (2016) Vestibular-evoked myogenic potentials in central vestibular disorders. J Neurol 263(2):210–220. https://doi.org/10.1007/s00415-015-7860-y
Fohner AE, Ranatunga DK, Thai KK, Lawson BL, Risch N, Oni-Orisan A, Jelalian AT, Rettie AE, Liu VX, Schaefer CA (2019) Assessing the clinical impact of CYP2C9 pharmacogenetic variation on phenytoin prescribing practice and patient response in an integrated health system. Pharmacogenet Genomics 29(8):192–199. https://doi.org/10.1097/fpc.0000000000000383
Hamed SA (2017) The auditory and vestibular toxicities induced by antiepileptic drugs. Expert Opin Drug Saf 16(11):1281–1294. https://doi.org/10.1080/14740338.2017.1372420
Gandelman-Marton R, Arlazoroff A, Dvir Z (2016) Posturography in MS patients treated with high dose methylprednisolone. Neurol Res 38(7):570–574. https://doi.org/10.1080/01616412.2016.1177927
Choung YH, Park K, Moon SK, Kim CH, Ryu SJ (2003) Various causes and clinical characteristics in vertigo in children with normal eardrums. Int J Pediatr Otorhinolaryngol 67(8):889–894. https://doi.org/10.1016/s0165-5876(03)00136-8
Posner EB, Mohamed K, Marson AG (2005) A systematic review of treatment of typical absence seizures in children and adolescents with ethosuximide, sodium valproate or lamotrigine. Seizure 14(2):117–122. https://doi.org/10.1016/j.seizure.2004.12.003
Merchant SN, Velázquez-Villaseñor L, Tsuji K et al (2000) Temporal bone studies of the human peripheral vestibular system. Normative vestibular hair cell data. Ann Otol Rhinol Laryngol Suppl 181(5_suppl):3–13. https://doi.org/10.1177/00034894001090s502
Murofushi T, Shimizu K, Takegoshi H, Cheng PW (2001) Diagnostic value of prolonged latencies in the vestibular evoked myogenic potential. Arch Otolaryngol Head Neck Surg 127(9):1069–1072. https://doi.org/10.1001/archotol.127.9.1069
Mauch E (2001) Hirnstammanfälle. Aktuelle Neurol 28:42–44. https://doi.org/10.1055/s-2001-15336
Otte WM, van Eijsden P, Sander JW, Duncan JS, Dijkhuizen RM, Braun KPJ (2012) A meta-analysis of white matter changes in temporal lobe epilepsy as studied with diffusion tensor imaging. Epilepsia 53(4):659–667. https://doi.org/10.1111/j.1528-1167.2012.03426.x
Slinger G, Sinke MR, Braun KP et al (2016) White matter abnormalities at a regional and voxel level in focal and generalized epilepsy: a systematic review and meta-analysis. Neuroimage Clin 12:902–909. https://doi.org/10.1016/j.nicl.2016.10.025
Bronstein AM, Patel M, Arshad Q (2015) A brief review of the clinical anatomy of the vestibular-ocular connections-how much do we know? Eye (Lond) 29(2):163–170. https://doi.org/10.1038/eye.2014.262
Chin S (2018) Visual vertigo: vertigo of oculomotor origin. Med Hypotheses 116:84–95. https://doi.org/10.1016/j.mehy.2018.04.025
Latini F, Hjortberg M, Aldskogius H et al (2015) The classical pathways of occipital lobe epileptic propagation revised in the light of white matter dissection. Behav Neurol 2015:872645
Tartara A, Manni R, Mira E et al (1984) Polygraphic study of vestibular stimulation in epileptic patients. Rev Electroencephalogr Neurophysiol Clin 14(3):227–234. https://doi.org/10.1016/s0370-4475(84)80009-x
Jenssen S, Gracely EJ, Sperling MR (2006) How long do most seizures last? A systematic comparison of seizures recorded in the epilepsy monitoring unit. Epilepsia 47(9):1499–1503. https://doi.org/10.1111/j.1528-1167.2006.00622.x
Perucca E, Elger C, Halász P, Falcão A, Almeida L, Soares-da-Silva P (2011) Pharmacokinetics of eslicarbazepine acetate at steady-state in adults with partial-onset seizures. Epilepsy Res 96(1-2):132–139. https://doi.org/10.1016/j.eplepsyres.2011.05.013
Acknowledgements
Nil.
Funding
There are no fundings to disclose.
Author information
Authors and Affiliations
Contributions
AHK searched the literature, analyzed, and interpreted the patient data, prepared, and reviewed the manuscript. KHA searched the literature and reviewed the manuscript. SME gathered and analyzed the patient data and prepared the manuscript. ASM reviewed the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval from the Ethical Committee of Faculty of Medicine, Menoufia University (according to Helsinki Declaration) with approval number (1055/9/5/2018) and written consent from all the patients were obtained.
Consent for publication
Not applicable.
Competing interests
There are no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kabel, A.E.M.H., Afifi, K.H., ElFakhrany, S.M. et al. Cervical and ocular vestibular evoked myogenic potentials in epileptic patients. Egypt J Otolaryngol 37, 51 (2021). https://doi.org/10.1186/s43163-021-00114-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-021-00114-9