Abstract
Background
Sinonasal inverted papilloma or Schneiderian papilloma is a rare benign tumor of paranasal sinuses and nasal cavities. It can cause bone remodeling and has a significant malignant potential. Hence, it is very important to diagnose and treat the tumor at the earliest. Recurrence can occur even after surgical extensive resection.
Case presentation
This case report highlights a case of a 36-year-old male patient who presented with right-sided reduced vision, nasal blockage, headache, and occasional blood-tinged nasal discharge.
CT scan of paranasal sinuses revealed chronic sinonasal polyposis with secondary fungal colonization. MRI of the brain with orbit and PNS was suspicious for aggressive neoplastic disease with encasement of the cavernous sinuses and involvement of orbital fissure. The patient was operated for extended functional endoscopic sinus surgery. Histopathology revealed moderately differentiated invasive squamous cell carcinoma associated with Schneiderian (inverted) papilloma. Post-operatively, the patient received radiation for 4 weeks. Post-operative check nasal endoscopy was done 3 and 6 months after completion of radiotherapy which showed no evidence of recurrent disease with good healing and mucosalization of all the sinuses.
Conclusions
Sinonasal inverted papilloma, though a benign tumor, may turn malignant. Diagnosis is based on radiological investigations (in order to know the extent of the disease) and biopsy (to check if it is benign or additional malignancy present). Staging of the tumor helps in outlining the treatment protocol in each case. Post-surgery radiotherapy is indicated in cases where there is malignancy or complete resection of the tumor cannot be achieved. Meticulous follow-up of the post-operative patients is vital to check for recurrence.
Similar content being viewed by others
Background
Sinonasal inverted papilloma also called Schneiderian papilloma is a benign tumor of paranasal sinuses and nasal cavities. It has a high propensity of bone remodeling and destruction. Complete surgical resection may not be always possible; hence, recurrence is a possibility. Sinonasal inverted papilloma, although benign, can become malignant with time [1]. The factor that is responsible for this formation is yet unknown, although allergy, occupational pollutants, chronic inflammation, and infection with human papilloma virus have been postulated [1]. It accounts for 0.5–4.0% of all nasal tumors and 2–3% of all nasal polyps [2].
Case presentation
A 36-year-old, smoker, male patient came to ENT OPD with chief complaints of right-sided reduced vision for 15 days, right-sided nasal blockage with headache, and occasional blood-tinged nasal discharge of 3 months duration. The patient had taken treatment from a local doctor for sinusitis without much relief. Ophthalmic examination revealed 6/18 vision on the right side and 6/6 vision on the left side.
Diagnostic nasal endoscopy showed right-sided polypoidal nasal mass with minimal bleeding on touch. It was painless and extended posteriorly up to the sphenoethmoidal area.
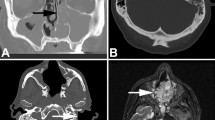
CT scan of paranasal sinuses revealed complete soft tissue opacification of frontal (right > left), right ethmoid and sphenoid sinuses with bony erosion of the sinus walls. Focal bony attenuation of sphenoid sinus was seen especially along its roof with mild elevation of pituitary gland. It was suggestive of sinonasal polyposis with secondary fungal colonization (Fig. 1).
MRI of the brain with orbit and PNS (plain and contrast) revealed right-sided enhancing soft tissue completely occluding the sphenoid sinus with encasement of the cavernous sinuses and involvement of orbital fissure suspicious of a neoplastic disease process. Mucosal thickening and enhancement of right ethmoidal air cells and frontal sinus may be suggestive of inflammatory sinusitis or extension of a similar disease process (Fig. 2).
The patient was operated for extended functional endoscopic sinus surgery under general anesthesia. Uncinectomy, middle meatal antrostomy, posterior ethmoidectomy, and sphenoidotomy were done. The right nasal mass extending from lamina papyracea up to posterior ethmoidal air cells was removed and sent for histopathology. A soft tissue mass, firm in consistency and bleeding on touch, was observed in the sphenoid sinus and was sent separately for histopathology. The soft tissue was cleared; however, it could not be excised totally due to the extension of the soft tissue near the internal carotid artery and optic nerve. Frontal sinusotomy was done and frontal sinus was cleared of any inflammatory mucosa.
First, a biopsy of the right nasal mass revealed Schneiderian (inverted) papilloma. Second, a biopsy of the right sphenoid sinus soft tissue revealed moderately differentiated invasive squamous cell carcinoma (Fig. 3).
Post-operative period was uneventful, and the patients’ right eye vision improved from 6/18 to 6/9 and was corrected to acceptable levels by spectacles. Saline irrigations twice daily for 1 month was administered given to clear any debris, mucopus, blood clots, and other diseased tissue.
The patient underwent a PET-CT scan for further evaluation and the extent of the disease which showed local suspicious tissue. The patient underwent post-operative intensity-modulated radiation therapy, a total dose of 64 Grays with onboard image guidance in 34 fractions in a span of 1 month.
Post-operative CT scan of PNS was done 3 months after completion of radiotherapy which showed minimal heterogeneously enhancing soft tissue in the base of sphenoid sinus on the left side medial to left petrous apex. All other post-operative areas were clear of disease.
Post-operative check nasal endoscopy was done 3 and 6 months after completion of radiotherapy which showed no evidence of recurrent disease with good healing and mucosalization of all the sinuses. Check biopsy taken from various soft tissue sites of the nasal cavity which was negative for any recurrent or active disease (Fig. 4).
Right vision remained stable at 6/9 with refractive correction. The patient is still under regular follow-up.
Discussion
Sinonasal inverted papilloma is a benign tumor predominately seen in white males in the age group of 50 years [1]. Clinically patients present with nasal obstruction, rhinorrhea, epistaxis, and facial pain or pressure [1]. In our study, the patient presented with right-sided reduced vision and right-sided nasal blockage with headache and with occasional blood-tinged nasal discharge.
Radiographically, inverted papilloma shows opacification of paranasal sinuses with or without bone destruction. It should be kept in mind that these features are also seen in nasal polyps, mucoceles of maxillary sinuses, or cholesterol granuloma [2]. The nasal columnar epithelium initially changes to a transitional epithelium, then it undergoes squamous metaplasia, followed by epithelial dysplasia and carcinoma in situ and finally invasive squamous cell carcinoma [2]. Thus, carcinomas with inverted papilloma can co-exist together. Combined lesions of inverted papilloma and carcinoma can be classified into three histological categories. In group I, the carcinoma and the inverted papilloma are present in the same anatomical region but inverted papilloma has not given rise to this carcinoma. In group II, inverted papilloma is seen along with invasive carcinoma. In group III, here, patients underwent treatment for an inverted papilloma but after the treatment, the patient develops invasive cancer without any evidence of papillomas [3]. Our case could be classified in the second group.
Treatment of inverted papilloma depends on the Krouse classification, which is as follows [4]:
-
T1 - Tumor totally confined to the nasal cavity, without extension into the sinuses. There must be no concurrent malignancy.
-
T2 - Tumor involving the ostiomeatal complex and ethmoid sinuses, and/or the medial portion of the maxillary sinus, with or without the involvement of the nasal cavity. There must be no concurrent malignancy.
-
T3 - Tumor involving the lateral, inferior, superior, anterior, or posterior walls of the maxillary sinus, the sphenoid sinus, and/or the frontal sinus, with or without the involvement of the medial portion of the maxillary sinus, the ethmoid sinuses, or the nasal cavity. There must be no concurrent malignancy.
-
T4 - All tumors with any extranasal/extrasinus extension involve adjacent, contiguous structures such as the orbit, the intracranial compartment, or the pterygomaxillary space. All tumors are associated with malignancy.
In our study, the patient had right-sided enhancing soft tissue occluding the sphenoid sinus with encasement of the cavernous sinuses and involvement of orbital fissure consistent with an aggressive neoplastic disease process. So it is classified as stage T4 according to Krouse classification.
Treatment of inverted papilloma is mainly surgical. The various surgical approaches include [5] (Table 1):
Radiation therapy in inverted papilloma is given in two circumstances [6]:
-
Associated carcinoma.
-
Suspected incomplete removal due to extension in anatomically inaccessible or inoperable cases.
For post-operative patients, radiotherapy is given in a dose of 56 Grays approximately, irrespective of whether resection was microscopically complete or not. For non-operable patients, the mean dose of radiotherapy is 61 Grays. In cases of carcinoma preferred treatment is surgery followed by Radiotherapy [7].
Our patient underwent complete Functional Endoscopic Sinus Surgery with complete removal of soft tissues except for the tissue that was encasing the internal carotid artery and the optic nerve, in order to preserve or improve the vision of the patient. Hence the patient received intensity-modulated radiation therapy of 64 Grays in 34 fractions in a span of 1 month.
Inverted papilloma cases need to be follow-up for a minimum duration of 3 – 5 years or even lifetime [7].
In our study, post-operative scans and check nasal endoscopy were done 3 months and 6 months after completion of radiotherapy. It showed no evidence of recurrent disease, no distant or lymphatic metastasis with good healing, and mucosalization of all the sinuses. Check biopsy was taken from various soft tissue sites of the nasal cavity which was negative for any recurrent or active disease. The patient is still under regular follow-up.
Conclusions
Sinonasal inverted papilloma is although a benign tumor, but it may transform into malignancy. Clinical diagnosis, radiological investigations, and histopathology biopsy are mandatary for the staging of the tumor, which in turn helps in outlining the treatment protocol (surgery and or radiotherapy). Meticulous follow-up of the post-operative patients is vital to check for recurrence.
Availability of data and materials
This case report highlights a case of a 36-year-old male patient who presented with right-sided reduced vision, nasal blockage, headache, and occasional blood-tinged nasal discharge. CT scan of paranasal sinuses, MRI of the brain with orbit and PNS, and histopathological report from tissue taken during functional endoscopic sinus surgery revealed moderately differentiated invasive squamous cell carcinoma associated with Schneiderian (inverted) papilloma.
Abbreviations
- CT scan:
-
Computerized tomography scan
- MRI:
-
Magnetic resonance imaging
- PNS:
-
Paranasal sinus
- PET:
-
Positron emission tomography
References
Buchwald C, Franzmann MB, Tos M (1995) Sinonasal papillomas: a report of 82 cases in Copenhagen County, including a longitudinal epidemiological and clinical study. Laryngoscope. 105(1):72–79. https://doi.org/10.1288/00005537-199501000-00016 PMID: 7837917
Myers EN, Fernau JL, Johnson JT, Tabet JC, Barnes EL (1990) Management of inverted papilloma. Laryngoscope. 100(5):481–490. https://doi.org/10.1288/00005537-199005000-00008 PMID: 2184303
Saha SN, Ghosh A, Sen S, Chandra S, Biswas D (2010) Inverted papilloma: a clinico-pathological dilemma with special reference to recurrence and malignant transformation. Indian J Otolaryngol Head Neck Surg 62(4):354–359. Published online 2011 Jan 1. https://doi.org/10.1007/s12070-010-0056-y
Krouse JH (2000) Development of a staging system for inverted papilloma. Laryngoscope. 110(6):965–968. https://doi.org/10.1097/00005537-200006000-00015 PMID: 10852514
Carta F, Blancal JP, Verillaud B, Tran H, Sauvaget E, Kania R, Herman P (2013) Surgical management of inverted papilloma: approaching a new standard for surgery. Head Neck. 35(10):1415–1420. https://doi.org/10.1002/hed.23159 Epub 2012 Sep 24. PMID: 23002029
Strojan P, Jereb S, Borsos I, But-Hadzic J, Zidar N (2013) Radiotherapy for inverted papilloma: a case report and review of the literature. Radiol Oncol. 47(1):71–76. https://doi.org/10.2478/v10019-012-0045-8
Yu H-X, Liu G (2014) Malignant transformation of sinonasal inverted papilloma: A retrospective analysis of 32 cases. Oncol Lett 8(6):2637–2641. https://doi.org/10.3892/ol.2014.2539 Epub 2014 Sep 16. PMID: 25360173; PMCID: PMC4214400
Acknowledgements
We would like to thank the helpful collaboration of Dr N G Huilgol and the Radiation Department Team, Department of Radiation Oncology, Dr. B. N. Hospital, Mumbai, Maharashtra, India.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MJ collected patients’ details and followed up. BS analyzed and interpreted the patient data. Both the authors contributed in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
All authors hereby declare that there is no financial or personal relationship that could cause a conflict of interest regarding this article. There are no financial or personal relationships with people or organizations that could inappropriately bias employment, consultancies, stock ownership, honoraria, paid expert testimony, patent applications/registrations, and grants or other funding.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent to publish this information was obtained from the study participant.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Juvekar, M., Sarkar, B. Squamous cell carcinoma arising from inverted Schneiderian papilloma: a case report. Egypt J Otolaryngol 37, 46 (2021). https://doi.org/10.1186/s43163-021-00113-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-021-00113-w