Abstract
Background
Chronic rhinosinusitis represents an important health care problem in the world. Deviated nasal septum leads to increased chance of impaired mucociliary clearance, osteomeatal complex obstruction, and development of rhinosinusitis. Studies have revealed the role of septoplasty in curing chronic rhinosinusitis in patients with significant septal deviation. The purpose of this study is to reveal the role of septoplasty alone or combined with functional endoscopic sinus surgery in improving the outcome of chronic rhinosinusitis in patients with significant septal deviation.
Results
Postoperative computed tomography findings in group A (underwent septoplasty only) were mild opacity of ethmoid (25%), sinus mucosal thickening (15%), and occluded osteomeatal complex with discharge (25%). Postoperative computed tomography findings in group B mild opacity of ethmoid (30%), sinus mucosal thickening (20%), and occluded osteomeatal complex with discharge (30%). The Sino-Nasal Outcome Test score in group A decreased significantly from 85.75 to 28.85 (P < 0.05). In group B (underwent combination of septoplasty and functional endoscopic sinus surgery), the Sino-Nasal Outcome Test score also decreased significantly from 87.75 to 32.55 (P < 0.05). The improvement was 85% in group A and 80% in group B.
Conclusion
The post-operative improvement has no significant difference between the two groups. Hence, we suggest that septoplasty alone can be adequate for the treatment of chronic rhinosinusitis with septal deviation.
Similar content being viewed by others
Background
Chronic rhinosinusitis (CRS) represents an important health care problem in the world [1]. The term sinusitis refers to a group of disorders characterized by inflammation of the mucosa of paranasal sinuses (PNS). The inflammation nearly always involves the nose; therefore, the term rhino-sinusitis (CRS) is used. Chronic rhinosinusitis is defined as two major symptoms/signs (facial pain/pressure, facial congestion/fullness, nasal blockage, nasal discharge, hyposmia/anosmia, purulence on nasal examination) or one major and two minor symptoms/signs (headache, fever, halitosis, fatigue, dental pain, cough, ear pain/pressure/fullness) for more than 12 weeks duration [2]. Anatomic variations can lead to obstruction of osteomeatal complex (OMC), which can be enhanced by inflammation and result in compromised mucocilliary clearance; this may result in chronic or recurrent rhino sinusitis. The most frequent OMC anatomic variation is septal deviation [3]. Deviated nasal septum leads to increased chance of impaired mucociliary clearance, ostiomeatal complex obstruction, and development of rhinosinusitis [2].
Septal deviation is usually classified into seven types. Type 1 is characterized by the vertical septal deflection in the valve area. This deformity does not interfere with the normal function of the valve. Type 2 is characterized by the vertical septal deflection in the valve area. This deformity interferes with the normal valve function. Type 3 is characterized by the vertical septal deflection in the close neighborhood of the head of the middle turbinate. Type 4 is characterized by two vertical septal deflections, one in the valve area on one side and another in the neighborhood of the head of the middle turbinate on the opposite side. Type 5 is characterized by unilateral septal basal crest, and the opposite septal side is almost totally flat. Type 6 is characterized by unilateral, horizontal gutter in the anterior and basal septal parts. Type 7 is very variable and can consist of various combinations and is almost always bizarre [4]. Lately, studies have revealed the role of septoplasty in curing CRS in patients with significant septal deviation. The success rate was higher in patients with Functional Endoscopic Sinus Surgery (FESS) and septoplasty. However, the adequacy of FESS alone in management of deviated nasal septum (DNS) with chronic maxillary sinusitis is not well documented [5].
This study was designed to reveal whether only septal correction is adequate to improve the subjective and objective outcome in patients with CRS and septal deviation.
Methods
This prospective study was conducted to compare between the results of combination or not of septoplasty with FESS. It involved 40 patients with both CRS and significant septum deviation who were operated upon between September 2017 and January 2019 at Otorhinolaryngology Department of Al-Zahraa University Hospital. Their age ranged from 18 to 40 years. Patients were randomly divided into two groups: group A included 20 patients who underwent only septoplasty. Group B included 20 patients who underwent septoplasty and FESS.
While selecting patients with CRS (as demonstrated in the CT scan as isolated or unilateral diffuse mucosal thickening, bone changes, or air-fluid level with ongoing symptoms consistent with CRS) for the study the following criteria was observed: all patients involved in the study had significant septum deviation, defined as deformities involving cartilaginous and/or bony parts that affect OMC as regards radiologic evaluation, had medically resistant CRS at the time of surgery that is failed maximal medical therapy for CRS to provide improvement, deviated septum associated with chronic frontal, maxillary or ethmoid sinusitis, aged from 18 to 40 years old. Any patients with mild septal deviations such as septal spurs or isolated anterior cartilaginous or posterior bony deviations, allergy and/or asthma, nasal polyps, systemic disease such as tuberculosis, sarcoidosis or Wegner granulomatosis, Revision FESS or submucous resection were excluded from the study.
Endoscopic examinations were performed by 2.7- or 4.0-mm rigid 0° or wide angle 30° endoscopes using topical decongestant.
The patients were subjected to high-resolution computed tomography (HRCT) nose and PNS without using contrast material (coronal and axial views) for anatomy and disease of sinuses in which Lund and Mackey radiological staging system was applied [6].
Sinonasal outcome was assessed using the change in 20-Item Sino-Nasal Outcome Test (SNOT-20), which is a validated, self-administered, quality of life instrument specific for patients with symptoms of rhinosinusitis [7]. Awad et al. (2014) translated the questionnaire into an Arabic one, and the filling of the questionnaires was performed by every patient assisted by the research team [8]. The questionnaire was completed by every patient at the two time points of the study (immediately before the operation and then at 3 months follow-up visits). Patients rate the severity of their condition on each of the 20 items using a 0–5 category rating system:
-
0 = not present/no problem.
-
1 = very mild problem.
-
2 = mild or slight problem.
-
3 = moderate problem.
-
4 = severe problem.
-
5 = problem as ‘bad as it can be’.
Septoplasty was performed in all patients under general anesthesia using the Cottle technique [9]. This technique respects the dorsum nasi and allows more natural correction by respecting the osteo-cartilaginous nasal bridge. In addition, the Cottle technique improves the nasal mucosal congestion and avoids surgical reduction of anterior end of inferior turbinate [8].
FESS was performed only in group B under general anesthesia. The extent of the surgery was determined by the extent of disease but always included uncinectomy, anterior ethmoidectomy, and middle meatal antrostomy. Surgeries in both groups were performed by well-trained rhinology surgeons [10].
Two days of nasal packing was applied in all patients with 2 weeks of postoperative antibiotics as well as topical buffered saline solution.
Three months post-operatively, all patients were evaluated by CT scan and SNOT-20 questionnaire. We compared the subjective and objective improvement for the two groups at 3 months postoperative visits.
Recorded data were analyzed using the statistical package for social sciences, version 20.0 (SPSS Inc., Chicago, IL, USA). Quantitative data were expressed as mean ± standard deviation (SD). Independent-samples t test of significance was used when comparing between two means. Paired sample t test of significance was used when comparing between related samples. Chi-square (χ2) test of significance was used in order to compare proportions between qualitative parameters. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the P value was considered significant as the following, P value < 0.05 was considered significant, P value < 0.001 was considered as highly significant, and P value > 0.05 was considered insignificant. Qualitative data were expressed as frequency and percentage.
Results
Forty patients were included in the study. Twenty patients were in the septoplasty-only group (group A) and 20 were in the septoplasty and FESS group (group B). Group A included 9 female (45%) and 11 male (55%) with average age of 26.10 ± 7.11 years. Group B included 8 female (40%) and 12 male (60%) with average age of 29.70 ± 6.44 years. There was no significant difference between both groups with respect to sex and age.
Post-operative CT finding according to the Lund and Mackey score in group A decreased significantly from (8.1 ± 2.19) to (1 ± 1.2139). In group B, post-operative CT finding according to the Lund and Mackey score also decreased significantly from 7.3 ± 1.49 to 1.05 ± 1.234.
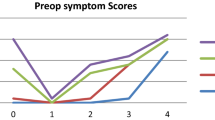
The SNOT score in group A decreased significantly from 85.75 ± 7.48 to 28.85 ± 16.94), and group B also decreased significantly from 87.75 ± 9.39 to 32.55 ± 19.58.
There is no statistically significant difference between both groups as regards post-operative CT findings (Figs. 1 and 2 and Supplementary Figure 1) according to the Lund and Mackey score (Table 1) and SNOT-20 score (Fig. 3, Table 2).
Discussion
Chronic rhinosinusitis is one of the most common diseases in many parts of the world. CRS is a clinical diagnosis and imaging is only indicated after adequate medical treatment; therefore, imaging should be interpreted considering history, examination, and response to medical treatment [2].
Nasal septum deviation can disturb nasal physiology, and it can be combined with conchal hypertrophy or other anatomical variations. Nasal septum deviation can narrow the middle meatus by pushing the concha laterally leading to obstruction and secondary nasal infection in all sinuses by disturbing normal mucus drainage [11].
This study aimed to find if septoplasty alone without combination with FESS is enough for treatment of patients with CRS and septal deviation.
Post-operative CT finding according to the Lund and Mackey score in both groups decreased with no significant difference. The symptoms measured by SNOT score also decreased in both groups with no significant difference. This means that the use of septoplasty alone or combined with FESS in treatment of patients with CRS and deviated nasal septum gives the same outcome.
Ganjian et al. 1999 have established independent models of nasal obstruction and ostial occlusion in the same animal. Their findings suggested that integrity of nasal airflow seemed to have a significant effect on the maintenance of the aerobic antral environment, essential to the maintenance of normal sinus function [12].
Sarna et al. 2002 found that severe septal deviation had been noted as a contributing factor for sinusitis [13].
Jang et al. concluded that concave-side septal mucosa increases the incidence of chronic rhino-sinusitis due to impaired mucociliary transport, presumably because of ciliary loss, increased inflammation, and decreased density of glandular acini [14].
By using a similar technique, other researcher reported that anatomical and histologic alterations were demonstrated on obstructed side leading to recurrent attacks of rhino-sinusitis [15].
Homsioglou et al. 2007 found that among three kinds of septal deviations, cartilaginous deviation, bony deviation, and high septal deviation, the later had a significant relationship with leading to recurrent rhino-sinusitis [16].
Hatipoglu et al. 2008 found that there was an association between the degree of deviation and the presence of sinusitis [17].
Another study showed that septal deviation is known to be the most common reason for OMC dysfunction, nasal obstruction, and nasal mucocilliary clearance alteration [9].
Aramani et al. 2014 found that deviated nasal septum was the most common anatomical variation encountered in osteomeatal complex obstruction. Deviated nasal septum causes a decrease in the critical area of the osteomeatal unit predisposing to obstruction, chronic rhino sinusitis, and related complications [18].
Madani et al. 2015 said that their study had the most prevalence of septal deviation in CRS patients and revealed there a strong association between nasal septal deviation and CRS [19].
Contrarily in another study, they found that nasal septal deviation of some degree was present in 65% of the cases, and no relationship was present between nasal septal deviation and sinus disease [18].
Kapusuz et al. 2013 found that mild and moderate septal deviations lacked any significant effect on maxillary sinus volumes and sinusitis findings, and severe deviations were found to have significant impact on these parameters [11].
Jun et al (2009) who found that correction of septal deviation might be more effective in alleviating nasal obstruction by improving the nasal patency. Nasal obstruction, rhinorrhea, and sneezing did significantly improve after surgery [20].
Babu et al. 2017 said that septoplasty with endoscopic osteomeatal clearance is a procedure which is highly efficacious and well tolerated in treating headache due to sinusitis secondary to DNS [21].
Bayiz et al. 2005 who said that septal deviation is a common cause of nasal obstruction. Septoplasty only or septoplasty plus ESS revealed similar results in the treatment of patients with CRS and septal deviation subjectively and objectively [5].
Goel et al. 2012 observed that septoplasty alone was adequate in patients with chronic maxillary sinusitis with hypertrophy of antral mucosa. On the other hand, septoplasty and FESS gave excellent results in expert hands only [22].
Also, Awad et al. 2014 found that septoplasty-only in the treatment of patients with CRS and septal deviation revealed similar results subjectively with septoplasty and FESS. Therefore, they suggested that septoplasty alone can be adequate for treatment of CRS with septal deviation [7].
The study done by Thakur et al. 2017 showed that the success rate was higher in patients with septoplasty alone as compared to those in FESS with septoplasty suggesting adequacy of septoplasty alone in management of chronic maxillary sinusitis with DNS [2].
The limitations of the study are that the number of patients was small and the follow-up was only 3 months. However, long follow-up period is better.
Our study suggests using septoplasty alone instead of using it combined with FESS in management of patients suffering from CRS and deviated nasal septum as it gives the same results and at the same time it is less invasive and results in faster recovery time.
Conclusion
Subjective and objective outcomes of only septoplasty versus FESS plus septoplasty were similar in patients with CRS and septal deviation. In addition, septoplasty alone is considered as minimally invasive technique with short operation time and recovery time. Therefore, our findings suggest that septoplasty can be considered as the first choice in the surgical treatment of patients with CRS and septal deviation.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CRS:
-
Chronic rhinosinusitis
- DNS:
-
Deviated nasal septum
- FESS:
-
Functional endoscopic sinus surgery
- HRCT:
-
High-resolution computed tomography
- OMC:
-
Osteomeatal complex
- PNS:
-
Paranasal sinuses
- SNOT:
-
Sino-Nasal Outcome Test
References
Dursun E, Korkmaz H, Eryýlmaz A et al (2003) Clinical predictors of long-term success after endoscopic sinus surgery. Otolaryngol Head Neck Surg 129:526–531
Thakur K, Gupta VD, Surya M, Ahluwalia A (2017) Comparative evaluation of FESS and septoplasty with FESS in cases of DNS with chronic maxillary sinusitis. International Journal of Research in Medical Sciences 5(8):3523–3529
Gevorgyan A, Fokkens JW (2016) Chronic frontal rhinosinusitis: diagnosis and management. Springer, Berlin Heidelberg, pp 77–104
Eren SB, Tugrul S, Dogan R et al (2014) Objective and subjective evaluation of operation success in patients with nasal septal deviation based on septum type. American journal of rhinology & allergy 28(4):e158–e162
Bayiz U, Dursun E, Islam A et al (2005) Is septoplasty alone adequate for the treatment of chronic rhinosinusitis with septal deviation? Am J Rhinol. 19(6):612–616
Hopkins C, Browne JB, Slack R et al (2007) The Lund-Mackay staging system for chronic rhinosinusitis: How is it used and what does it predict? Otolaryngology–Head and Neck Surgery 137(4):555–561
Browne JB, Hopkins C, Slack R, Cano SJ (2007) The Sino-Nasal Outcome Test (SNOT): can we make it more clinically meaningful? Otolaryngology–Head and Neck Surgery 136(5):736–741
Awad OGAN, Abd El-Karim AA, Hamad MS (2014) Role of surgical septal correction in subjective improvement of chronic rhinosinusitis. The Egyptian Journal of Otolaryngology 30:196–200
Amaral OFD, Mizoguchi FM, Freitas RDS et al (2017) A comparative study between universal eclectic septoplasty technique and cottle. International Archives of Otorhinolaryngology 21:281–285
Ramakrishnan VR, Hauser LJ, Feazel ML et al (2015) Sinus microbiota varies among chronic rhinosinusitis phenotypes and predicts surgical outcome. Journal of Allergy and Clinical Immunolgy. In: vol: 136; issue:2; 334 -42
Kapusuz GZ, Ozkiris M, Okur A et al (2013) The effect of nasal septal deviation on maxillary sinus volumes and development of maxillary sinusitis. Eur Arch Otorhinolaryngol 270(12):3069–3073
Ganjian E, Gannon PJ, Fliegelman LJ et al (1999) Nasal obstruction: An alternative to ostiomeatal complex dysfunction in sinus disease. Laryngoscope 109:1848–1851
Sarna A, Hayman LA, Laine FJ, Taber KH (2002) Coronal imaging of the osteomeatal unit: anatomy of 24 variants. J Comput Assist Tomogr 26(1):153–157
Jang Y, Myong N, Park K et al (2002) Mucociliary transport and histologic characteristics of the mucosa of deviated nasal septum. Arch Otolaryngol Head Neck Surg 128:421–424
Shin SH, Heo WW (2005) Effects of unilateral naris closure on the nasal and maxillary sinus mucosa in rabbit. Auris Nasus Larynx 32:139–143
Homsioglou E, Balatsouras DG, Alexopoulos G et al (2007) Pneumatized superior turbinate as a cause of headache. Head Face Med 3:1–5
Hatipoglu HG, Cetin MA, Yuksel E (2008) Nasal septal deviation and concha bullosa coexistence: CT evaluation. B-ENT 4:227–232
Aramani A, Karadi RN, Kumar S (2014) A Study of anatomical variations of osteomeatal complex in chronic rhinosinusitis patients CT findings. In: Journal of Clinical and Diagnostic Research Vol-8(10): KC01-KC04
Madani SA, Hashemi SA, Modanluo M (2015) The incidence of nasal septal deviation and its relation with chronic rhinosinusitis in patients undergoing functional endoscopic sinus surgery. J Pak Med Association Vol. 65. No. 6(612):614
Jun BC, Kim SW, Cho JH et al (2009) Is turbinate surgery necessary when performing a septoplasty? Eur Arch Otorhinolaryngol 266:975–980
Babu B, Reynolds AM, Pillai GN (2017) Efficacy of septoplasty with endoscopic osteomeatal clearance in the management of headaches due to chronic sinusitis secondary to deviated nasal septum. International Journal of Otorhinolaryngology and Head and Neck. Surgery 3(1):25–28
Goel AK, Yadav SPS, Ranga R et al (2012) Comparative study of septoplasty alone and with FESS in maxillary sinusitis with septal deviation. Clin Rhinol Int J. 5(1):19–24
Acknowledgements
Not applicable.
Funding
There is no source of funding.
Author information
Authors and Affiliations
Contributions
SYM contributed to the concept of this work. BAM and ASH designed the work as well as data analysis. FMA interpreted the data, drafted the work, and revised it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consents were obtained from the participants of the study. The consent form and methods of the study were approved by the ethical committee of AFMG-IRB (Central Administration of Research and Development–Egypt Ministry of Health, Registration number: RHBIRB2018122001).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Figure 1: Showing post-operative CT showing Rt ethmoid sinusitis in Group B.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mostafa, S.Y., Abd-Elgaber, F.M., Mohamed, B.A. et al. Impact of septoplasty alone or with endoscopic sinus surgery for treatment of chronic rhinosinusitis with deviated septum. Egypt J Otolaryngol 37, 2 (2021). https://doi.org/10.1186/s43163-020-00066-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-020-00066-6