Abstract
Neuroleptic malignant syndrome is a rare, life-threatening neurologic emergency characterized by fever, rigidity, autonomic instability, mental status changes, and an elevated creatine kinase level. It often occurs shortly after the initiation of neuroleptic treatment, or after a dose increase. The management of patients with NMS is based upon clinical severity and includes supportive care and withdrawal of antipsychotic agents and agents like bromocriptine and dantrolene. Complications include acute renal failure associated with rhabdomyolysis, respiratory failure, electrolyte imbalance, hepatic failure, seizures from hyperthermia, metabolic derangements, etc.
Similar content being viewed by others
Introduction
NMS is a life-threatening neurologic emergency associated with the use of dopamine antagonists, and less commonly with dopamine agonist withdrawal [1, 2]. First-generation antipsychotic agents (e.g., haloperidol, fluphenazine) are most commonly implicated but NMS can occur with any antipsychotic agent including second-generation drugs ( e.g., clozapine, risperidone, olanzapine) and also with antiemetic drugs (e.g., metoclopramide, promethazine, and levosulpride). Incidence rates for NMS range from 0.02 to 3% among patients taking antipsychotics [3]. Case–control studies implicate recent or rapid dose escalation, a switch from one agent to another, and parenteral administration as risk factors [4]. Clinical features include tetrad of typical symptoms including fever (typically above 38 °C), rigidity (generalized, lead pipe rigidity), mental status changes, and dysautonomia manifesting as tachycardia, labile blood pressure, tachypnea, arrhythmias. Elevated creatine kinase, typically more than 1000 international units /L. An international multispeciality consensus group published diagnostic criteria for NMS in 2011 [3]. Differential diagnoses include meningitis, encephalitis, serotonin syndrome, malignant hyperthermia, malignant catatonia, and other drug-related syndromes (withdrawal of intrathecal baclofen therapy, acute intoxication with cocaine, MDMA, etc.) A case is described that highlights the challenges met in making the diagnosis, treatment, and final outcome of the patient.
Case
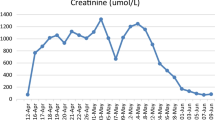
A 67-year-old female with a history of BPAD for the last 30 years, Parkinson’s disease, and drug-induced, hypothyroidism sought psychiatry consultation for altered behavior in the form of restlessness, decreased response to conversation and pacing around purposelessly which was noticed by her family. A provisional diagnosis of exacerbation of psychosis was made as she had received polypharmacy [Inj Haloperidol, Inj Phenergan (promethazine), Inj Lorazepam, Tab Olanzapine, Tab Venlafaxine (75 mg OD), Tab Divalproex-500 mg, Tab Lamotrigene (100), Tab Paroxetine, Tab Cariprazine, Tab Trihexyphenidyl, Tab Syndopa Plus, Tab Donepezil, Tab Thyroxine (25 mcg)]. Two days after admission to a psychiatric ward, the patient developed agitation, decreased responsiveness, and anuria with high-colored urine (Fig. 1) for which she presented to our hospital for further treatment. On examination her urine output was 100 ml for 2 days, although normotensive (BP 110/70 mmHg) she had tachycardia (heart rate 110 beats/min) and exhibited parkinsonian features including rigidity (lead pipe rigidity). An electrocardiogram revealed no acute ischemic changes. Cardiovascular, respiratory, and abdominal examinations were unremarkable. Six hours after admission she developed fever (temperature 102 °F) and Diaphoresis. Laboratory investigations (Table 1) revealed markedly elevated CK levels 168,593 U/L, raised LDH levels 3243 U/L, elevated SGOT/PT levels 1836/128 U/L, alkaline phosphatase 82 U/L, raised neutrophil count 90%, urine R/E showed albuminuria (+ + + +), elevated serum creatinine level 8.4 mg/dl, raised urea level 116 mg/dl. Serum electrolytes showed potassium 4.4 meq/L, sodium 136 meq/L, calcium 8.4 mg/dl, serum uric acid 8.8 mg/dl. ABG was done which revealed metabolic acidosis (Ph 7.2, HCO3-18 mEq, PCO2 46 mmHg, PO2 88 mmHg). NCCT head (Fig. 2) revealed cerebral atrophy. CSF study was normal.
NCCT head on admission [5]
A firm diagnosis of NMS with AKI with rhabdomyolysis was made. The patient was taken for hemodialysis on the same day of admission in view of AKI due to rhabdomyolysis, dialysis was done for 3 h with 1500 ml ultrafiltration. The patient was kept in the intensive care unit. Tablet Bromocriptine was started (2.5 mg TDS) which was tapered over the course of 14 days and then stopped. For her agitation Inj. Lorazepam in the dose 1 mg iv/im every 6 h was given. Inj. Diazepam (10 mg i/v slowly) single dose was also helpful. The patient underwent regular hemodialysis for her ATN due to rhabdomyolysis; however, her other lab parameters showed a decreasing trend (Table 1). After a few days, she developed a focal seizure in one episode. NCCT Head (Fig. 3) was repeated and subsequently, an MRI brain (Fig. 4) was done which revealed increased hypodense areas in B/L cerebral and cerebellar hemispheres. MRI Brain was suggestive of encephalopathy. Her GCS dropped in view of the same. We continued the supportive therapy and she has started steroids (Inj Dexamethasone 4 mg i/v, 6hrly and gradually tapered). The patient’s clinical status and GCS improved significantly afterward and she was discharged in a hemodynamically stable state after 20 days.
Repeat NCCT head [5]
MRI brain [5]
Discussion
This case illustrates one of the many clinical presentations possible with the depot use of potent antipsychotic drugs and the many difficulties faced during her treatment due to complications of NMS. The diagnosis of NMS was established based on the typical history of depot drug administration and other characteristic features including markedly raised serum CPK levels, worsening mental status, muscle rigidity, and diaphoresis. Our patient developed rhabdomyolysis and landed into acute kidney injury. Even with more sensitive criteria, a high index of suspicion is still necessary for clinicians to make a prompt diagnosis based on clinical history [6].
Comments
Neuroleptic malignant syndrome (NMS) is a life-threatening neurologic emergency associated with the use of antipsychotic (neuroleptic) agents and is characterized by a distinctive clinical syndrome of mental status change, rigidity, fever, and dysautonomia. Incidence rates for NMS range from 0.02 to 3% among patients taking antipsychotic agents. While most patients with NMS are young adults, the syndrome has been described in all age groups from 9 to 78 years. In most studies, males outnumber females twofold. This was a rare case where a female was affected with many complications of NMS. A rapid loading schedule, especially with potent neuroleptics like haloperidol is considered to be the principal contributing factor in the development of NMS, by causing a sudden and massive down-regulation of dopaminergic transmission. This could have occurred in our patient [7].
Message
Polypharmacy in the case of neuropsychiatric diseases should always be avoided to prevent dreadful conditions like NMS with ARF leading to rhabdomyolysis.
Availability of data and materials
Yes.
References
Szota AM, Radajewskal I, Grudzka P, Araszkiewicz A (2020) Lamotrigine, quetiapine and aripiprazole –induced neuroleptic malignant syndrome in a patient with renal failure caused by lithium: a case report. BMC Psychiatry 20:179
Margetic B, Aukst-Margetic B (2010) Neuroleptic malignant syndrome and its controversies. Pharmacoepidemiol Drug Saf 19:429
Picard LS, Lindsay S, Strawn JR et al (2008) Atypical neuroleptic malignant syndrome : diagnostic controversies and considerations. Pharmacotherapy 28:530
Modi S, Dhariya D, Schultz L, Varelas P (2016) Neuroleptic malignant syndrome: complications, outcomes, and mortality. Neurocrit Care 24:97
Jain RS, Gupta PK, Gupta ID, Agrawal R, Kumar S, Tejwani S (2015) Reversible magnetic resonance imaging changes in a case of neuroleptic malignant syndrome. Am J Emerg Med 33(8):1113
Eiser AR, Neff MS, Slifkin RF (1982) Acute myoglobinuric renal failure. A conscequence of the neuroleptic malignant syndrome. Arch Intern Med 142:601
Gurrera RJ, Caroff SN, Cohen A et al (2011) An international consensus study of neuroleptic malignant syndrome diagnostic criteria using the Delphi method. J Clin Psychiatry 72:1222
Acknowledgements
None
Funding
None.
Author information
Authors and Affiliations
Contributions
Dr. Sunakshi Sharma contributed to the intellectual content, conception, and design. Dr Sanjay Bhat contributed to writing the manuscript. Dr. Zahoor Ahmed contributed to data collection and computer work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Yes.
Consent for publication
None.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sharma, S., Bhat, S. & Ahmed, Z. Neuroleptic malignant syndrome with acute renal failure associated with rhabdomyolysis: a case report. Egypt J Intern Med 36, 57 (2024). https://doi.org/10.1186/s43162-024-00324-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43162-024-00324-6