Abstract
Fishbones are frequently swallowed by foreign objects that can penetrate the gastrointestinal tract. Nonetheless, it is quite uncommon for these fishbones to become lodged within the tract, resulting in the formation of foreign body granulomas that resemble submucosal tumors. When encountering this situation, it's important to consider differential diagnoses such as gastric intestinal stromal tumor, gastric leiomyoma, and gastric neurofibroma. We present a case of gastric foreign body granuloma that presents with dull aching epigastric pain. The patient gave a vague history of displaced intrauterine contraceptive devices (IUCD). Contrast CT and PET scan showed a gastric antral mass possibly a gastric cancer or a migrating IUCD. Endoscopic ultrasound (EUS) suggested a perigastric foreign body reaction due to the presence of a linear echogenic structure in between the markedly thickened gastric antral wall and the right lobe of the liver. EUS-guided fine needle biopsy (EUS-FNB) revealed non-specific inflammatory reaction. Afterward, surgical exploration unveiled the cause of the mass as a foreign body granuloma caused by a perforating fishbone.
Similar content being viewed by others
Case presentation
A case of a 61-year-old female patient with no significant family history of malignancy. She has a past medical history of insertion of intrauterine contraceptive device (IUCD) 35 years ago and it was removed with difficulty afterward without documenting the removal of the whole device.
She presented with a dull aching upper abdominal pain for 1 month. This pain developed gradually over the first two weeks and increased in severity over the next 2 weeks. It was radiating to the back and it was not associated with vomiting or weight loss.
Physical examination was unremarkable, and laboratory tests and tumor markers were in the normal range.
The patient underwent upper gastrointestinal endoscopy which showed multiple superficial erosions and a small deep antral ulcer with a clean floor and edematous edges, measuring 0.5 cm in diameter, 2 cm away from the pyloric ring (Fig. 1). It was biopsied and histopathological examination revealed chronic gastritis of moderate activity.
18F-FDG PET/CT scan showed gastric pyloric anterior wall active irregular thickening with a linear hyperdense radio-opaque area within, having exophytic configuration encroaching on the related left hepatic lobe, the lesion measures 4.5 cm and eliciting a high SUVmax of 7.6 (Fig. 2).
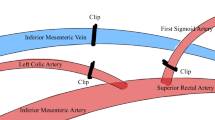
EUS examination showed a significantly (11 mm) thickened posterior antral wall with an oblong soft tissue area between the posterior antral wall and the left hepatic lobe with a linear dense hyperechoic structure inside, 30 mm in length. The picture was impressive of a severe inflammatory foreign body reaction versus a malignant lesion (Fig. 3).
The patient underwent surgical exploration from the left subcostal incision and the antral mass was adherent to the left hepatic lobe by dense adhesions. On dissection, the mass was opened and we found a foreign body in the form of a fish bone inside, confirming the diagnosis of a foreign body granuloma. No pus was discharged from the mass. Excision of the lesion was done with the closure of the antral opening in transverse continuous sutures to avoid stricture of the antral cavity. Abdominal drain was placed and closure of the wound was done in layers. The procedure and postoperative hospital stay were uneventful (Fig. 4).
Discussion
Gastric malignancy is the most common cause of gastric masses including gastric carcinoma, lymphoma, carcinoid tumor, or gastro-intestinal stromal tumor (GIST).
Benign lesions that present as gastric masses include true leiomyoma, schwannoma, lipoma, and ectopic pancreas, this makes up only 5–10% of all stomach tumors. Inflammatory lesions such as chronic gastritis or foreign body granuloma are much less likely possibilities [1].
Ingested foreign bodies mostly cause non-specific symptoms and in most cases, they pass through the gastrointestinal tract without complications [2].
In cases in which complications such as perforations of the stomach occur, patients present in a more insidious manner, which leads to difficulty in reaching the correct diagnosis. This probably occurs due to a thicker wall compared to a small bowel [3].
CT scan is considered the most accurate imaging modality in localizing ingested foreign bodies like fish bone with high sensitivity and specificity [4].
The picture of the intra-gastric bulge in endoscopy or CT picture suggesting a mass with a central hyperdense lesion should raise a high level of suspicion of the possibility of a foreign body even when the history is not clear. This does not exclude the possibility of malignancy as endoscopic biopsy is commonly superficial and small [5].
However, in this case, PET/CT suggested gastric malignancy as the first possibility due to the high SUVmax of 7.6 (Fig. 2); however, this may exceptionally occur in active inflammatory reactions.
EUS is another helpful diagnostic tool in submucosal gastric masses which enables visualization of lesion extensions with added value of possibility of obtaining tissue biopsy. In our case, it revealed the foreign body as a hyperechoic lesion while the biopsy showed chronic inflammation [6]. Up to our knowledge, this is the first reported case of gastric fish bone granuloma described by EUS and also up to our knowledge, no cases of gastric foreign body granulomas mistaken for gastric malignancy have been reported in Egypt.
It would have been almost impossible to remove this foreign body endoluminal by Endoscopy, as the mucosa was completely intact over it and the foreign body was not visualized. Surgery is the preferred method of excision for foreign bodies in the stomach but if the foreign body is visible, removal could be done with mucosal clipping to avoid perforation of the wall [1].
Availability of data and materials
Not applicable.
Abbreviations
- IUCD:
-
Intrauterine contraceptive device
- EUS:
-
Endoscopic ultrasound
- EUS-FNB:
-
EUS guided fine needle biopsy
- GIST:
-
Gastro-intestinal stromal tumor
References
Goh PMY, Lenzi JE (2001) Benign tumors of the duodenum and stomach. In: Holzheimer RG, Mannick JA (eds) Surgical Treatment: Evidence-Based and Problem-Oriented. Zuckschwerdt, Munich. Available from: https://www.ncbi.nlm.nih.gov/books/NBK6948/.
Webb WA (1995) Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc 41(1):39–51. https://doi.org/10.1016/s0016-5107(95)70274-1
Ginsberg GG (1995) Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc 41(1):33–38. https://doi.org/10.1016/s0016-5107(95)70273-3
Tumor S, Case TWO, Medical O (2020) Fishbone as foreign body granuloma of the stomach mimicking as submucosal tumor : - Two case reports fishbone as foreign body granuloma of the stomach mimicking as Aditya Prasad p 7–9
Kim HU (2016) Oroesophageal fish bone foreign body. Clin Endosc 49(4):318–326. https://doi.org/10.5946/ce.2016.087
Goh BK, Tan YM, Lin SE et al (2006) CT in the preoperative diagnosis of fish bone perforation of the gastrointestinal tract. AJR Am J Roentgenol 187(3):710–714. https://doi.org/10.2214/AJR.05.0178
Acknowledgements
We would like to acknowledge our great Kasr Al Ainy Hospital, and its workers, nurses, and staff members, for all the support and help in this study and throughout our careers.
Funding
The authors received no funding for this study.
Author information
Authors and Affiliations
Contributions
HO was the main endoscopist and did the final review and editing. AZ and HD helped in investigations. HF collected the data. AA wrote the manuscript. AS designed the methodology and helped in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institution’s ethical committee. Oral and written informed consent was obtained from the patient or from his eligible relative.
Consent for publication
Oral and written informed consent was obtained from the patient or his eligible relative.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Okasha, H.H., Alzamzamy, A.E., Delsa, H. et al. Gastric foreign body granuloma resembling gastric cancer: a case report. Egypt J Intern Med 36, 18 (2024). https://doi.org/10.1186/s43162-024-00281-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43162-024-00281-0