Abstract
Background
Secondary bacterial infections are an important cause of mortality in patients with coronavirus disease 2019 (COVID-19). All healthcare providers acted with utmost care with the reflex of protecting themselves during the COVID-19 period. We aimed to compare the rates of ventilator-associated pneumonia (VAP) and bloodstream infections (BSIs) in our intensive care units (ICUs) before and during the COVID-19 outbreak surges.
Methods
This multicenter, retrospective, cross-sectional study was performed in six centers in Turkey. We collected the patient demographic characteristics, comorbidities, reasons for ICU admission, mortality and morbidity scores at ICU admission, and laboratory test data.
Results
A total of 558 patients who required intensive care from six centers were included in the study. Four hundred twenty-two of these patients (males (62%), whose mean age was 70 [IQR, 58–79] years) were followed up in the COVID period, and 136 (males (57%), whose mean age was 73 [IQR, 61–82] years) were followed up in the pre-COVID period. BSI and VAP rates were 20.7 (19 events in 916 patient days) and 17 (74 events in 4361 patient days) with a −3.8 difference (P = 0.463), and 33.7 (31 events in 919 patient days) and 34.6 (93 events in 2685 patient days) with a 0.9 difference (P = 0.897), respectively. The mortality rates were 71 (52%) in pre-COVID and 291 (69%) in COVID periods.
Conclusion
Protective measures that prioritize healthcare workers rather than patients and exceed standard measures made no difference in terms of reducing mortality.
Similar content being viewed by others
Introduction
Despite the worldwide mass vaccination strategy, coronavirusdisease 2019 (COVID-19) caused significant morbidity and mortality with emerging new vaccine-resistant variants. It worsened those with an underlying disease, such as diabetes, cancer, and neurological disorders [1, 2]. Non-invasive and/or invasive mechanical respiratory support may be required in patients with COVID-19 who develop progressive respiratory failure. Secondary bacterial infections in the intensive care unit (ICU) are an important cause of mortality in these patients [3, 4].
Corticosteroids and other immunomodulatory agents [e.g., interleukin (IL)-6, IL-1 antagonists], frequently used in patients with COVID-19, have the potential to increase nosocomial infections [5]. Preventive bundles have been developed to prevent intensive care-associated infections [6]. Strict contact precautions and hand hygiene are the main factors among these measures. All healthcare providers acted with utmost care with the reflex of protecting themselves during the COVID-19 period, especially for strict contact precautions and hand hygiene [7]. It is an important issue whether this care provides a reduction in the rates of hospital infections. There are conflicting results regarding the frequency of nosocomial infections in ICU observational studies conducted during the COVID-19 period.
In a meta-analysis evaluating bacterial co-infection and secondary bacterial infections, the burden of infections was not found statistically significant in hospitalized patients at the beginning of the pandemic [8]. We believe the dynamic process of the disease and intensive care conditions require a different perspective.
In this study, we aimed to compare the rates of ventilator-associated pneumonia (VAP) and bloodstream infections (BSIs) in our ICUs before and during the COVID-19 outbreak.
Material and methods
Study design and population
This multicenter, retrospective, cross-sectional study was performed in six centers in Turkey. In this study, we analyzed patients admitted to the ICU during the first wave of COVID-19 (April 1, 2020, to June 30, 2020) and the second wave of COVID-19 (October 1, 2020, to December 31, 2020) and compared them with patients admitted to the ICU before the COVID-19 pandemic (April 1, 2019, to June 30, 2019).
Randomly selected adult patients were included in the study who were hospitalized in the ICU for 3 to 28 days. We excluded pregnant women and patients who had an infection at the time of admission to the ICU or who were in the incubation period of probable nosocomial infections (48 h of ICU hospitalization).
Data collection and definitions
We collected the patient demographic characteristics, comorbidities (based on Charlson’s Comorbidity Index), reasons for ICU admission, Acute Physiology and Chronic Health Evaluation (APACHE) II and Sequential Organ Failure Assessment (SOFA) scores at ICU admission, laboratory tests (blood leukocyte count in cells/mm3, blood neutrophil count in cells/mm3, blood lymphocyte count in cells/mm3, blood platelet count in cells/mm3, blood hemoglobin in g/dL, serum D-dimer in ng/mL, serum lactate in mmol/L), microbiologic results (blood cultures, respiratory samples, and antimicrobial susceptibility), and clinical outcomes (duration of mechanical ventilation, duration of central venous catheter, ICU length of stay, ICU mortality) from the patients’ electronic medical records.
The definitions of VAP and BSI were defined according to the criteria provided by the Centers for Disease Control and Prevention’s National Healthcare Safety Network and European Centers for Disease Control and Prevention, which include clinical, radiologic, and bacteriologic criteria. Only VAP with positive microbiologic criteria was included [9, 10].
Outcomes
The primary outcome of our study was the incidence of VAP and BSIs among patients admitted to the ICU during the COVID-19 pandemic as compared with before the pandemic. The secondary endpoint was the etiology of VAP and BSI.
Statistical analysis
Physicians randomly selected the patients who were hospitalized in ICUs from their hospitals’ electronic data archives according to the exclusion criteria and recorded the relevant information in the prepared Microsoft Access-based data program. Patients were divided into groups based on the date of infection relative to COVID-19 as pandemic and pre-pandemic cohorts. We used Fisher’s exact test and the 2-tailed Wilcoxon signed-rank test for analysis. A P value of <.05 was considered statistically significant. Calculations, figures, and tables were made using the R program.
Results
A total of 558 patients who required intensive care from six centers were included in the study. Of these patients, 422 (males (62%), whose mean age was 70 [IQR, 58–79] years) were followed up during the COVID period, and 136 (males (57%), whose mean age was 73 [IQR, 61–82] years) were followed up in the pre-COVID period. Demographic, basic clinical scales, rates of BSI and VAP, and in-hospital mortality rates in the pre-COVID and COVID periods are summarized in Table 1. The comparison of the underlying disease spectrum of the patients is also described in Table 1. Underlying disease was detected in 94% of the patients in the pre-COVID period and 92.6% of the patients in the COVID period. Hypertension was the most common underlying disease in the pre-COVID and COVID periods. It is noteworthy that during the COVID period, those with chronic lung disease were hospitalized at a lower rate and those with diabetes mellitus were hospitalized at a higher rate.
The mean APACHE II score was found as 20 (IQR, 14–25) in the pre-COVID period, which was significantly higher than in the COVID period [17 (IQR, 11–24)]. The SOFA score, on the other hand, was found to be the same in each group, with a value of 6 (IQR 4.0–8.0).
BSI and VAP rates were 20.7 (19 events in 916 patient days) and 17 (74 events in 4361 patient days) with a −3.8 difference (P = 0.463), and 33.7 (31 events in 919 patient days) and 34.6 (93 events in 2685 patient days) with a 0.9 difference (P = 0.897), respectively.
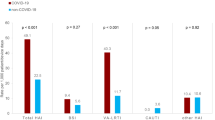
The microbiology of the infections is described in Table 2. The most frequent bacterium among patients with primary BSI in the COVID period was Acinetobacter baumannii (n = 14, 36%); this was isolated in endotracheal aspirate (ETA) cultures in both periods. Stenotrophomonas maltophilia was an emergent bacterium that was isolated from ETA cultures only during the COVID period.
Discussion
Our retrospective cohort study found that the mean age of patients in the ICUs was lower during the COVID period. Male sex was dominant in both periods. The BSI rate increased, but the VAP rate remained stable.
Comparing the patients admitted to the ICU, we found increased mortality rates in patients admitted during the pandemic (52% vs. 69%, P < 0.001). Unterberg et al. also found a significant difference in the mortality rates of patients with sepsis as 52% during the pandemic and 33% before the pandemic [11]. They speculated that the patients admitted to the hospital with more severe disease were due to their delayed admission. They supported their theory with higher initial SOFA scores during the pandemic than before the pandemic. In our study, the initial mean SOFA scores were the same, but APACHE II scores were lower in patients during the COVID period. The statistically significantly increased diabetes mellitus rates may be associated with steroid treatment effects, which are widely used in pre-ICU clinics.
In their review, Fumagalli et al. reported that the VAP incidence varied from 18 to 45 episodes per 1000 ventilator days among patients with COVID-related acute respiratory distress syndrome (ARDS). Incidence rates varied widely based on the country, study population, and criteria used to identify VAP [12]. In the present study, there was no significant difference in VAP incidence density during the pandemic compared with the pre-pandemic period. Similar to ours, in a multicenter study evaluating 21 Brazilian hospitals, there was no significant difference in VAP incidence density between the two periods [13]. However, in two other recent reports, there was a significant increase in VAP rates in patients with COVID-19. In these studies, VAP rates in the control groups were 15.4 and 13 episodes per 1000 ventilator days, respectively. In our study, the high incidence rate of VAP in the control group could have affected the results [14, 15]. During the pandemic and pre-pandemic periods, the most common infections in patients who were mechanically ventilated were VAP, and in both periods, Gram-negative bacteria were the predominant microorganisms (>70% in most series) [12]. In a multicenter study conducted in Italian hub hospitals, Enterobacterales and Staphylococcus aureuscaused 33% and 28% of cases of VAP, respectively, in critically ill patients with COVID-19 [16]. In a European multicenter study, Gram-negative bacilli, mainly Pseudomonas aeruginosa (22.3%), Enterobacter spp. (18.8%), and Klebsiellaspp. (11.5%), were the most common pathogens of ventilator-associated lower respiratory tract infections in patients with COVID-19 [17]. In a Turkish study investigating the lower respiratory tract infections of patients in the ICU during the pandemic versus the pre-pandemic period, A. baumannii was the most common bacteria, followed by K. pneumoniaein both periods [18]. In our study, similar to this result, A. baumannii was the most common microorganism in the two periods, but P. aeruginosa was found to be the second most common pathogen in the COVID period and K. pneumoniae in the pre-COVID period. In Turkey, A. baumannii was an important cause of hospital-acquired infections in the ICU before the pandemic.
In our study, the BSI rates were found as 15% and 11% in the COVID and pre-COVID periods, respectively. A. baumannii (36%), coagulase (coA)-negative Staphylococcus (36%), and Enterococcus faecium (28%) in blood culture were the most common microorganisms during the pandemic.
Similar results were observed in a Serbian study in the ICU; A. baumannii (26.5%) and coA-negative Staphylococcus (26.5%) were the main pathogens of BSIs, followed by Enterococcusspp. (11.2%) [19]. Consistent with our study, Palanisamy et al. found that A. baumannii(32.8%) was the most common pathogen of BSIs. However, although Gram-negative pathogens (82.8%) were predominant in their study, conflictingly 64% of BSIs were Gram-positive bacteria in our study [20]. In the study of Zhu et al., 26.9% of bacteremia were in the ICU. In microbiologic analysis, mostly Enterococcus spp. were detected (n=90, 22.8%), followed by Escherichia coli (n=55, 14.0%), Klebsiella spp. (n=49, 12.4%), and CoA-negative Staphylococcus (n=48, 12.2%), respectively. Acinetobacterhas never been revealed in blood cultures [21]. In our cohort, Acinetobacter spp. and S. hominis were found most commonly in blood cultures as associated with BSIs, followed by E. faecium. Interestingly, Acinetobacterspp. were never detected in another cohort study [3]. There were no differences in BSI- and VAP-associated etiologic patterns between patients who were polymerase chain reaction (PCR) positive and negative in the COVID period.
Conclusions
The mortality rates of patients in the ICUs were higher during the COVID-19 period. Protective measures that prioritize healthcare workers rather than patients and exceed standard measures made no difference in terms of reducing mortality.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- VAP:
-
Ventilator-associated pneumonia
- BSI:
-
Bloodstream infection
- ICU:
-
Intensive care unit
- IL:
-
Interleukin
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- SOFA:
-
Sequential Organ Failure Assessment
- ETA:
-
Endotracheal aspirate
- ARDS:
-
Acute respiratory distress syndrome
- PCR:
-
Polymerase chain reaction
References
Hoffmann M, Krüger N, Schulz S, Cossmann A, Rocha C, Kempf A et al (2022) The Omicron variant is highly resistant against antibody-mediated neutralization: implications for control of the COVID-19 pandemic. Cell 185:447–56
Ahmad W, Shabbiri K (2022) Two years of SARS-CoV-2 infection (2019–2021): structural biology, vaccination, and current global situation. Egypt J Intern Med 34(1):5. https://doi.org/10.1186/s43162-021-00092-7
Bardi T, Pintado V, Gomez-Rojo M, Escudero-Sanchez R, Azzam Lopez A, Diez-Remesal Y et al (2021) Nosocomial infections associated to COVID-19 in the intensive care unit: clinical characteristics and outcome. Eur J Clin Microbiol Infect Dis 40(3):495–502
Ponsford MJ, Jefferies R, Davies C, Farewell D, Humphreys IR, Jolles S et al (2021) Burden of nosocomial COVID-19 in Wales: results from a multicentre retrospective observational study of 2508 hospitalised adults. Thorax 76(12):1246–9
Obata R, Maeda T, Rizk D, Kuno T (2021) Increased secondary infection in COVID-19 patients treated with steroids in New York City. Jpn J Infect Dis 74(4):307–15
Pincock T, Bernstein P, Warthman S, Holst E (2012) Bundling hand hygiene interventions and measurement to decrease health care–associated infections. Am J Infect Control 40(4, Supplement):S18-27
Ambrosch A, Rockmann F, Klawonn F, Lampl B (2020) Effect of a strict hygiene bundle for the prevention of nosocomial transmission of SARS-CoV-2 in the hospital: a practical approach from the field. J Infect Public Health 13(12):1862–7
Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR et al (2020) Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis 26(12):1622–9
Centers for Disease Control and Prevention/National Healthcare Safety Network (2022) Identifying healthcare-associated infections (HAI) for NHSN surveillance (Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/2psc_identifyinghais_nhsncurrent.pdf)
Plachouras D, Lepape A, Suetens C (2018) ECDC definitions and methods for the surveillance of healthcare-associated infections in intensive care units. Intensive Care Med 44(12):2216–8
Unterberg M, Rahmel T, Rump K, Wolf A, Haberl H, von Busch A et al (2022) The impact of the COVID-19 pandemic on non-COVID induced sepsis survival. BMC Anesthesiol 22(1):12
Fumagalli J, Panigada M, Klompas M, Berra L (2022) Ventilator-associated pneumonia among SARS-CoV-2 acute respiratory distress syndrome patients. Curr Opin Crit Care 28(1):74–82
Porto APM, Borges IC, Buss L, Machado A, Bassetti BR, Cocentino B et al (2022) Healthcare-associated infections on the ICU in 21 Brazilian hospitals during the early months of the COVID-19 pandemic: an ecological study. Infect Control Hosp Epidemiol 18:1–37
Vacheron CH, Lepape A, Savey A, Machut A, Timsit JF, Vanhems P et al (2022) Increased incidence of ventilator-acquired pneumonia in coronavirus disease 2019 patients: a multicentric cohort study. Crit Care Med 50(3):449–59
Maes M, Higginson E, Pereira-Dias J, Curran MD, Parmar S, Khokhar F et al (2021) Ventilator-associated pneumonia in critically ill patients with COVID-19. Crit Care Lond Engl 25(1):25
Grasselli G, Scaravilli V, Mangioni D, Scudeller L, Alagna L, Bartoletti M et al (2021) Hospital-acquired infections in critically ill patients with COVID-19. Chest 160(2):454–65
Rouzé A, Martin-Loeches I, Povoa P, Makris D, Artigas A, Bouchereau M et al (2021) Relationship between SARS-CoV-2 infection and the incidence of ventilator-associated lower respiratory tract infections: a European multicenter cohort study. Intensive Care Med 47(2):188–98
Bahçe YG, Acer Ö, Özüdoğru O (2022) Evaluation of bacterial agents isolated from endotracheal aspirate cultures of Covid-19 general intensive care patients and their antibiotic resistance profiles compared to pre-pandemic conditions. Microb Pathog 164:105409
Despotovic A, Milosevic B, Cirkovic A, Vujovic A, Cucanic K, Cucanic T et al (2021) The impact of COVID-19 on the profile of hospital-acquired infections in adult intensive care units. Antibiot Basel Switz 10(10):1146
Palanisamy N, Vihari N, Meena DS, Kumar D, Midha N, Tak V et al (2021) Clinical profile of bloodstream infections in COVID-19 patients: a retrospective cohort study. BMC Infect Dis 21(1):933
Zhu N, Rawson TM, Mookerjee S, Price JR, Davies F, Otter J, et al. Changing patterns of bloodstream infections in the community and acute care across two COVID-19 epidemic waves: a retrospective analysis using data linkage. Clin Infect Dis Off Publ Infect Dis Soc Am. 2021;ciab869
Acknowledgements
We are thankful to all dedicated healthcare workers at tertiary hospitals in the SARS-CoV-2 pandemic.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
FA, SS and HV made consept, designed and wrote the study. HV and HA did statistical analysis and interpreted the results. Selection of patients and control group and acquisition of data were proved by SS, ST, TM, AS, MAÇ, ÇBD, DTA, HA, YT. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ministry of Health (2021-03-26T17_41_25) and Niğde Ömer Halisdemir University Ethics Committee (date: July 2, 2021, No: 2021/11-26). The requirement for informed consent in addition to what the patients had given prior to hospitalization was waived because of the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sarı, S., Arslan, F., Turan, S. et al. Comparison of the healthcare-associated infections in intensive care units in Turkey before and during COVID-19. Egypt J Intern Med 35, 30 (2023). https://doi.org/10.1186/s43162-023-00215-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43162-023-00215-2