Abstract
Background
Mycoplasma pneumoniae is one of the leading causes of community-acquired pneumonia. Due to its microbiological variation, clinical presentations of mycoplasma infections are atypical and diverse. Multiple pulmonary and extrapulmonary manifestations of Mycoplasma pneumoniae have been documented. Among pulmonary, common manifestations are fever, malaise, lymphadenopathy, pneumonia, upper respiratory tract infections, sinusitis, etc. Necrotising pneumonia leading to cavitation as a manifestation is rather an uncommon presentation.
Case presentation
We are reporting a rare case of a 5-year-old female child who presented with bilateral haemorrhagic pleural effusion and necrotising pneumonia with cavitation along with extrapulmonary manifestation in the form of maculo-papular rash, Coombs-positive haemolytic anaemia and serositis. The child was started on azithromycin and symptomatic management, but she did not respond to it; she had clinical worsening and evidence of radiological necrotising pneumonia. The child was treated as macrolide-resistant mycoplasma pneumonia with levofloxacin, steroids and rigorous physiotherapy.
Conclusions
Accurate clinical acumen along with timely radiological imaging is the need of the hour for early diagnosis of macrolide-resistant mycoplasma pneumonia (MRMP). This case also emphasises role of fluoroquinolones and steroids in treatment of macrolide-resistant mycoplasma pneumonia.
Similar content being viewed by others
Background
Mycoplasma pneumonia (MP) is one of the leading etiological agent causing respiratory tract infections in children. In India, MP contributes to up to 30% of community-acquired pneumonia [1]. MP is a pathogen of Mycoplasmataceae family, characterised by its small size and the absence of cell wall which contributes to its inherent resistance to beta-lactam antibiotics. MP usually causes mild or moderate pneumonia which improves without sequelae, and rarely, it takes a fulminant course causing necrotising pneumonia, bronchiolitis obliterans, acute respiratory distress syndrome, lung abscesses, etc. Extrapulmonary manifestations like arthritis, maculo-papular rash, Steven-Johnsons syndrome, hepatitis, encephalitis and glomerulonephritis are seen in up to 25% MP infections [2].
The diagnosis of MP is usually based on immunological titres, as blood cultures are seldom positive. Enzyme-linked immunoassays IgM and IgG have 99% specificity and 98% sensitivity [3].
Case presentation
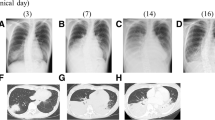
A previously healthy 5-year-old female child admitted to our tertiary care hospital, with complaints of fever and dry cough for 1 week. Prior to admission, she was treated with oral antibiotics for 5 days. On admission, the patient was febrile (38.5 °C), lethargic, tachycardic and tachypneic, and oxygen saturation was 88% on room air. She also had pallor but no cyanosis, clubbing or oedema. On respiratory system examination, the patient had reduced breath sounds bilaterally with fine crepitations. Chest X-ray revealed right lower zone pneumonia as shown in Fig. 1. She was started on oxygen by nasal prongs with flow of 4 L/min. On laboratory investigations, complete blood count (CBC) revealed anaemia with Hb of 7.1 g/dL (11–14 g/dL) and leucopenia-3300 cells/mm3 (4000–11,000 cells/mm3) with neutrophilic predominance (84%), CRP-74 mg/dL (N − < 1 mg/dL) and ESR-100 mm/h (N < 5 mm/h), and blood culture had no growth. The patient developed erythematous nonpruritic maculo-papular rash, which started on the chest and later progressed to trunk and limbs (Fig. 2). She received packed cell transfusion by 10 ml/kg body weight in the setting of anaemia, clinical worsening and increased oxygen requirement. Posttransfusion CBC had evidence of haemolysis with fall in Hb to 6.8 g/dL with corrected reticulocyte count of 4%. Sputum culture showed no growth, and sputum CBNAAT was negative. On further evaluation, direct Coomb’s test was strongly positive (4 +). MP was suspected as there was evidence of pneumonia with autoimmune haemolytic anaemia, rash and serositis. Mycoplasma IgM levels were high 33 ng/dL (> 11 ng/dL considered significant), and cold agglutinins were positive. The patient was given symptomatic management and was started on intravenous azithromycin at 10 mg/kg/dose; detailed evaluation with computed tomography (CT) thorax was done which revealed pneumonia with air bronchogram on left upper lobe, lingula and entire right lobe, with ground-glass opacification in left lower lobe and infrahilar region of right lower lobe with mild bilateral pleural effusion and mildly enlarged mediastinal lymph node. Diagnostic pleural tapping had haemorrhagic aspirate (Fig. 3). Pleural fluid examination showed transudative fluid with 20,000 RBCs and 5000 WBCs (75% neutrophils and 25% lymphocytes). Pleural fluid protein was 1.3 g/dL, and sugars were 93 mg/dL. Pleural fluid smear and CBNAAT (cartridge-based nucleic acid amplification test) were negative for mycobacterium tuberculosis. Patient also developed ascites in the meantime. As the patient had multisystem involvement with serositis, muco-cutaneous ulcers, high erythrocyte sedimentation rate and bicytopenia (thrombocytopenia and anaemia), she was investigated for autoimmune disorders such as systemic lupus erythematosus (SLE — antinucleic acid antibody (ANA) came weakly positive (1:80, fine speckled pattern), and anti double-stranded DNA (anti dsDNA) was negative. The child continued to have fever spikes, respiratory distress and extrapulmonary manifestations which pointed towards macrolide-resistant mycoplasma pneumonia (MRMP) infection. Repeat HRCT thorax was done, which revealed (Fig. 3) areas of consolidation with secondary large thick-walled cavitatory changes seen involving apico-posterior and anterior segment of left upper lobe (4.6*3.6 cm) and superior and basal segment of right lower lobe (4.4 × 4.1 cm). These findings of necrotising pneumonia with cavitations were suggestive of progression of disease despite adequate treatment with macrolide group of antibiotics as the other common causes of necrotising pneumonia are Staphylococcus aureus and streptococcus pneumonia. The sputum culture showed no growth, and blood culture also did not show any growth. Tuberculosis was also ruled out with sputum cartridge-based nucleic acid amplification test (CBNAAT).
The antibiotics were changed to intravenous levofloxacin at 10 mg/kg/dose, and oral steroids were started at a dose of 2 mg/kg/day, which was tapered over a period of 2 weeks. Intensive physiotherapy was started which included manoeuvres of percussion, vibration and incentive spirometry.
Clinically, improvement (fever decreased) was seen after 3 days of injection of levofloxacin and steroids, respiratory symptoms required 3 weeks to settle, Hb improved to 9 g/dL and platelets improved to 185,000 cells/mm3 by the end of 2 weeks. Patient was discharged after 28 days of admission. After 2 weeks of discharge, DCT was negative. HRCT thorax was done after 6 months of discharge which showed complete resolution of cavitation and fibroatelectatic changes Table 1.
Discussion
MP infection usually presents with minor respiratory illnesses, which are self-limiting and characterised by constitutional symptoms; however, 3–15% patients will develop pneumonia, and on rarer occasions, MP can present as tracheobronchitis with asthma-like clinical picture. Schoolgoing children and adolescents in the age group of 5–20 years of age are most susceptible for MP infection. MP has an incubation period of 2–4 weeks, and mode of transmission is via droplets and fomites. Macrolide resistance is observed in 90–100% mycoplasma pneumonia infections in Asia [4]. Conventionally, MP was treated with macrolides — oral azithromycin or clarithromycin in adequate dosage. Macrolide-resistant strains of MP are treated with either fluoroquinolones or tetracyclines. Clinically, symptoms of macrolide-resistant MP are similar to macrolide-sensitive MP, but worsening or persistence of clinical signs and symptoms and early radiological evaluation can guide to a diagnosis of macrolide-resistant MP [4].
In our case, the patient had persistent fever and respiratory distress with CT thorax showing cavitatory necrotising pneumonia (NP) giving evidence of inadequate response to macrolide group of antibiotics. NP is characterized by cavitatory lesions which are caused by necrosis and liquefaction of lung tissues. Most common causes of necrotizing pneumonia are Staphylococcus aureus and streptococcus pneumonia. These organisms could be ruled out as there was no growth in neither blood culture nor in sputum culture. Tuberculosis was also ruled as there was no significant contact history and sputum CBNAAT was negative. This helped us narrow down our diagnosis to an organism which is not usually grown in cultures and also present with multiple extrapulmonary manifestations. Thus, provisional diagnosis was mycoplasma pneumonia with extrapulmonary manifestations. It was late confirmed with mycoplasma antibody titers.
Children with necrotizing pneumonia are very sick, febrile and usually will not respond to even adequate dose of appropriate antibiotic. In some cases, there may be associated empyema which might require surgical drainage. Bronchopleural fistula is a rare complication of MP, which may be diagnosed with spontaneous pneumothorax. Lung necrosis can be detected at an early stage with contrast-enhanced chest CT. A study of 37 patients with MP by Baoying Zheng et al. describes the average time from onset of symptoms to development of necrotic lesion was 24 + / − 10 days [5]. Similarly, our patient had developed necrotising pneumonia by the 3rd week of illness which was identified with CT thorax. Another study of 25 children with MP caused by MRMP by Xia Wang et al. describes the usual antibiotic duration for treatment was 32 days, 80% had pleural effusion, 55% required thoracocentesis and 10% requires chest drainage [6, 7]. Our patient did not require any surgical intervention and was treated with fluoroquinolones and steroids for 7 days with complete recovery.
Extrapulmonary manifestations are in the form of rash, arthritis, serositis and autoimmune haemolytic anaemia. These are early signs which point towards diagnosis of MP infection. Extrapulmonary manifestations of MP are attributed to immunological cross-reactivity; steroids are therefore indicated in counteracting these immune responses [6, 8,9,10].
Our patient, even though it had developed necrotising pneumonia, pleural effusion and cavitation, did not require any invasive treatment. This emphasises that timely interventions along with appropriate antibiotics, good supportive care and intensive physiotherapy can result in complete recovery without compromising quality of life.
Conclusion
MRMP is on the rise in community. Accurate clinical acumen along with timely radiological imaging is the need of the hour for early diagnosis of MRMP. Mycoplasma pneumonia infection can have varied extrapulmonary manifestations which may sometimes present with multisystem involvement, and well-timed treatment of these manifestations might call for use of immunosuppressive treatment with steroids in addition to the usual antibiotic regimen. It should also be noted that macrolide resistance should be evaluated at a community level and appropriate antibiotic should be given. As macrolide-resistant mycoplasma pneumonia is becoming more prevalent in Asia, clinicians should rethink macrolides as first-line treatment to mycoplasma pneumonia.
Availability of data and materials
The datasets used or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MRMP:
-
Macrolide-resistant mycoplasma pneumonia
- MP:
-
Mycoplasma pneumonia
- SLE:
-
Systemic lupus erythematosus
- ANA:
-
Anti-nucleic acid antibody
- NP:
-
Cavitatory necrotizing pneumonia
References
Noviello S, Huang DB (2019) The basics and the advancements in diagnosis of bacterial lower respiratory tract infections. Diagnostics 9(2):37. https://doi.org/10.3390/diagnostics9020037
Nir-Paz R, Michael-Gayego A, Ron M, Block C (2006) Evaluation of eight commercial tests for Mycoplasma pneumoniae antibodies in the absence of acute infection. Clin Microbiol Infect 12(7):685–688. https://doi.org/10.1111/j.1469-0691.2006.01469.x. (PMID: 16774570)
Pereyre S, Goret J, Bébéar C (2016) Mycoplasma pneumoniae: current knowledge on macrolide resistance and treatment. Front Microbiol 7:974. https://doi.org/10.3389/fmicb.2016.00974. (PMID:27446015;PMCID:PMC4916212)
Zheng B, Zhao J, Cao L (2020) The clinical characteristics and risk factors for necrotizing pneumonia caused by Mycoplasma pneumoniae in children. BMC Infect Dis 20:391. https://doi.org/10.1186/s12879-020-05110-7
Tong L, Huang S, Zheng C, Zhang Y, Chen Z (2022) Refractory Mycoplasma pneumoniae pneumonia in children: early recognition and management. J Clin Med 11(10):2824
San Martin I, Zarikian SE, Herranz M, Moreno-Galarraga L. Necrotizing pneumonia due to mycoplasma in children: an uncommon presentation of a common disease. Adv Respir Med. 2018. https://doi.org/10.5603/ARM.a2018.0049. Epub ahead of print. PMID: 30594998.
Lee CHo. et al. Mycoplasma pneumoniae-associated necrotizing pneumonia in children: a case-report. Kosin Med J. 2019:57–64. pesquisa.bvsalud.org, https://doi.org/10.7180/kmj.2019.34.1.57.
Song WJ, Kang B, Lee HP, Cho J, Lee HJ, Choe YH (2017) Pediatric Mycoplasma pneumoniae infection presenting with acute cholestatic hepatitis and other extrapulmonary manifestations in the absence of pneumonia. Pediatr Gastroenterol Hepatol Nutr. 20(2):124–129. https://doi.org/10.5223/pghn.2017.20.2.124. (Epub 2017 Jun 28. PMID: 28730137; PMCID: PMC5517379)
Waris ME, Toikka P, Saarinen T, Nikkari S, Meurman O, Vainionpää R, Mertsola J, Ruuskanen O (1998) Diagnosis of mycoplasma pneumoniae pneumonia in children. J Clin Microbiol 36(11):3155–3159. https://doi.org/10.1128/JCM.36.11.3155-3159.1998. (PMID:9774556;PMCID:PMC105292)
Kumar S (2018) Mycoplasma pneumoniae: a significant but underrated pathogen in paediatric community-acquired lower respiratory tract infections. Indian J Med Res 147(1):23–31. https://doi.org/10.4103/ijmr.IJMR_1582_16. (PMID:29749357;PMCID:PMC5967212)
Acknowledgements
Not applicable.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
VS data collection; NM data collection and idea of research; AK idea of research, writing and proofreading; VS analysed and interpreted data; and the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Consent for publication from parent was taken.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mohan, N., Sawant, V.D. & Kondekar, A. Cavitatory necrotising pneumonia with extrapulmonary multi-systemic involvement — a rare presentation of macrolide-resistant Mycoplasma pneumoniae. Egypt J Intern Med 35, 20 (2023). https://doi.org/10.1186/s43162-023-00205-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43162-023-00205-4