Abstract
Background
Acute pancreatitis is a relatively common acute medical presentation that may progress beyond the pancreas to cause multi-organ failure or death. It is associated with high morbidity and mortality with mortality rates changing little in the past few decades despite advances in intensive care and surgical management. Early evaluation of acute pancreatitis severity is essential to allow the clinician to predict the patient’s clinical course, estimate the prognosis, determine the need for intensive care unit admission, and prevent complications. So, the purpose of our study is to evaluate the prognostic value of the neutrophil to lymphocyte ratio, lactate dehydrogenase enzyme, and proteinuria in patients with acute pancreatitis and its correlation with Ranson’s criteria scoring system as new, rapid, and easy parameters to predict severity of acute pancreatitis.
Results
The mean age of patients in years was 47.97, and the median was 52 with a range of ages between 18 and 87; 38% of the patients included were males, and 61% were females. The mean Ranson’s score was 2.77 ± 1.4, and the median was 3 with a range of 0–6; 44.5% of patients included have low severity, 42.4% have mild severity, and 13.1% of patients have high severity. Neutrophil to lymphocyte ratio both at the time of admission and after 48 h of admission was significantly increasing with an increase in disease severity with a P value of < 0.001 that was statistically significant. Lactate dehydrogenase enzyme at the time of admission was also significantly increasing with diseased severity with a P value of 0.001 that was statistically significant and the same for lactate dehydrogenase enzyme level after 48 h of admission with a P value of 0.002 that was also statistically significant. Proteinuria is positive only in 15.2% of patients and with the same result after 48 h of admission.
Conclusion
The neutrophil to lymphocyte ratio gives a rapid impression of the extent of the inflammatory process, and it can effectively predict severity at the time of admission and even after 48 h of admission and can also differentiate between patients with mild and severe acute pancreatitis in both calcular and non-calcular cause-dependent acute pancreatitis patients. Lactate dehydrogenase can be used to predict severity in calcular cause-dependent acute pancreatitis patients only at the time of admission and after 48 h of admission. Proteinuria in urine analysis on admission and after 48 h does not seem to be a reliable predictor for disease severity in acute pancreatitis.
Similar content being viewed by others
Background
Acute pancreatitis is a disease characterized by the devastation and irritation of pancreas tissue through the activation of pancreatic acinar cells as a result of being activated by different causes such as biliary disease, alcohol use, and hyperlipidemia [1]. The rate of events of each etiology of acute pancreatitis changes over geographic districts and socio-economic states.
Other causes which will cause acute pancreatitis include idiopathic, drug-induced pancreatitis; post-ERCP pancreatitis; any benign or malignant mass that obstructs the main pancreatic duct; autoimmune pancreatitis; bacterial and viral infection; trauma to the pancreas; congenital or acquired anatomical abnormalities as choledochal cysts, duodenal duplication, and secondary fibrosis of the pancreatic duct; hypercalcemia; and vasculitis (polyarteritis nodosa and systemic lupus erythematosus) [2,3,4].
According to the American College of Gastroenterology, a patient must have at least two of the following three features present to make the diagnosis of acute pancreatitis: (1) abdominal pain consistent with acute pancreatitis (acute onset of a persistent, severe, epigastric pain often radiating to the back), (2) serum amylase and/or lipase level at least 3 times greater than the upper limit of the normal value, and (3) characteristic manifestation of acute pancreatitis on contrast-enhanced computed tomography, magnetic resonance imaging, or transabdominal ultrasonography [5].
Acute pancreatitis can be mild, moderate, or severe. While mild pancreatitis is commonly self-limited, severe pancreatitis can be associated with the development of many local and systemic complications such as fluid collections and necrosis. Severe acute pancreatitis is associated with single or multiple organ failure with a mortality rate as high as 25% [6].
Forming risk-defining systems and determining the severity of acute pancreatitis are of great importance in predicting the prognosis and how successful the treatment is [7]. Several scoring systems, such as Ranson’s score, the Glasgow criteria, APACHE-II score, BISAP, and computed tomography severity index, have been developed. These scoring systems incorporate physiologic, laboratory, and radiographic parameters using cutoff values and converting continuous variables into binary values to evaluate and determine the severity of acute pancreatitis. Given that the multiple factors scoring systems are complex and sometimes difficult to use, there has been continued interest in identifying simpler or less expensive methods to predict severity [8].
Over the past years, multiple research groups have investigated the value of the hematological components of the systemic inflammatory response specifically for use in predicting the severity of the disease, as well as the outcome, and have reported that the individual components of the differential leukocyte count may have clinically predictive utility. Neutrophil to lymphocyte ratio (NLR) is a straightforward and effectively calculated systemic inflammation-based score that has been widely investigated in the assessment of a variety of disease states, including inflammatory, cardiovascular, and neoplastic conditions [9, 10].
Methods
A prospective study was performed in the period between May 2018 and May 2019.
Inclusion criteria
This study was carried out on 99 patients with acute pancreatitis, all of them fulfilling the 3 American College of Gastroenterology criteria for the diagnosis of acute pancreatitis: (1) abdominal pain consistent with acute pancreatitis (acute onset of a persistent, severe, epigastric pain often radiating to the back), (2) serum amylase and/or lipase level at least 3 times greater than the upper limit of the normal value, and (3) characteristic manifestation of acute pancreatitis on contrast-enhanced computed tomography, magnetic resonance imaging, or transabdominal ultrasonography.
Exclusion criteria
The following are the exclusion criteria:
-
1.
Patients are excluded from the study if they do not meet the criteria for acute pancreatitis.
-
2.
Patients who are under the age of 18.
-
3.
Patients with chronic pancreatitis.
All patients in the study were subjected to the following:
-
Full history and examination.
-
Full laboratory investigation such as liver function test, coagulation profile, kidney function test, complete blood count, serum calcium level, serum sodium and potassium level, and albumin level, and assessment of the patient according to Ranson’s score.
-
Neutrophil to lymphocyte ratio, lactate dehydrogenase, and proteinuria in urine analysis.
-
The parameters will be compared between cases of different etiologies in relation to Ranson’s criteria as two groups, acute gallstone pancreatitis and acute pancreatitis not due to gallstones as shown below, and the patients were categorized according to their Ranson’s score into low, mild, and high severity groups.

Ranson’s score interpretation
One point is given for each positive parameter:
-
0 to 2 points: low severity
-
3 to 4 points: low severity
-
5 to 6 points: mild severity
-
7 to 11 points: high severity [11]
The NLR, LDH, and proteinuria in urine analysis were assessed at the time of admission and after 48 h of admission in addition to the assessment of the patient according to Ranson’s score at the time of admission and after 48 h of admission.
Statistical analysis
Data were verified, coded by a researcher, and analyzed using IBM-SPSS 21.0 (IBM-SPSS Inc., Chicago, IL, USA). Descriptive statistics such as means, standard deviations, medians, ranges, and percentages were calculated. Test of significances—for continuous variables with more than two categories, ANOVA test was calculated to test the mean differences of the data that follow a normal distribution and independent sample Kruskal-Wallis was used to compare the median difference between the groups that do not follow a normal distribution, and post hoc test was calculated using Bonferroni corrections [12]. A significant P value was considered when it is equal to or less than 0.05.
Results
Ninety-nine patients diagnosed with acute pancreatitis were included in the study fulfilling the 3 American College of Gastroenterology criteria for the diagnosis of acute pancreatitis (38 of them were males and 61 females) as shown in Fig. 1. The mean age of patients in years was 47.97, and the median was 52 with a range of ages between 18 and 87 as shown in Fig. 2.
Seventy-six of the patients diagnosed with acute pancreatitis were due to calcular cause, and 23 were due to non-calcular cause including hypertriglyceridemia, idiopathic, and malignancy as shown in Fig. 3. The main presenting symptom of patients diagnosed with acute pancreatitis was epigastric pain radiating to the back with a range of 90.9% as shown in Fig. 4.
It was found that the mean ± SD of WBCs was 14.42 ± 5.8 with a median (range) of 14.7 (4–34), Hgb level mean ± SD was 12.01 ± 2.0 with a median (range) of 11.5 (8–17), and platelet level mean ± SD was 249.60 ± 88.1 with a median (range) of 234 (74–521) as shown in Table 1.
It was found that neutrophil to lymphocyte ratio at the time of admission mean ± SD was 8.15 ± 6.8 and the median was 5.5 with a range of 0.4–43 and that neutrophil to lymphocyte ratio after 48 h mean ± SD was 4.59 ± 3.1 and the median was 3 with a range of 0.8–27 as shown in Table 2. It was found that the mean LDH level at the time of admission was 562.21 ± 179.2 and the median was 541 with a range of 100–971) and that the mean LDH after 48 h of admission was 288.86 ± 125.1 and the median was 269 with a range of 75–843 as shown in Table 3.
It was found that the mean amylase level at the time of admission was 658.36 ± 319.1 and the median was 596 with a range of (37–2460) and that the mean amylase level after 48 h of admission was 250.16 ± 111.8 and the median was 189 with a range of 23–1069) as shown in Table 4.
Ranson’s criteria scoring system is calculated and interpreted for all patients and divided based on different etiologies in relation to Ranson’s criteria into two groups: acute gallstone (calcular)-dependent pancreatitis and acute non-gallstone (non-calcular)-dependent pancreatitis. It was found that the mean Ranson’s score was 2.77 ± 1.4, and the median was 3 with a range of 0–6.
Regarding the severity of acute pancreatitis (totally), it was found that 44.5% of patients have low severity, 42.4% have mild severity, and 13.1% of patients have high severity. Regarding the severity in case of non-calcular cause of acute pancreatitis (hypertriglyceridemia, idiopathic, and malignancy), it was found that 26.1% of patients have low severity, 56.5% have mild severity, and 17.4% of patients have high severity. Regarding the severity in case of calcular cause of acute pancreatitis, it was found that 50% of patients have low severity, 38.2% have mild severity, and 11.8% of patients have high severity as shown in Table 5 and Figs. 5 and 6.
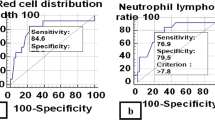
After categorization of the patients according to Ranson’s criteria scoring system into low, mild, and high severity, analysis of data revealed that NLR both at the time of admission and after 48 h of admission was significantly increased with an increase in disease severity with a P value of < 0.001 that was statistically significant. Analysis of data also revealed that LDH at the time of admission was also significantly increasing with disease severity with a P value of 0.001 that was statistically significant and revealed the same for LDH level after 48 h of admission with a P value of 0.002 that was also statistically significant as shown in Table 6.
Analysis of the data in case of patients diagnosed with acute pancreatitis due to non-calcular cause revealed that NLR both at the time of admission and after 48 h of admission was increasing with an increase in disease severity according to Ranson’s scoring system with a P value of 0.023 at admission and a P value of 0.003 after 48 h of admission that was statistically significant. About LDH, it was found that both levels at the time of admission and after 48 h of admission were statistically insignificant with a P value of 0.079 and 0.083, respectively, as shown in Table 7.
Analysis of the data in case of patients diagnosed with acute pancreatitis due to calcular cause revealed that NLR both at the time of admission and after 48 h of admission was increasing with an increase in disease severity according to Ranson’s scoring system with a P value of < 0.001 at admission and a P value of < 0.001 after 48 h of admission that was statistically significant. About LDH, it was found that both levels at the time of admission and after 48 h of admission were increasing with an increase in disease severity with a P value of 0.010 at admission and a P value of 0.020 48 h after admission that was statistically significant as shown in Table 8.
Discussion
The current study included 99 patients who were diagnosed to have acute pancreatitis; the mean age of those patients was 47.97 ± 8.11 years with a range between 18 and 87 years. Thirty-eight (38.4%) patients were males, and 61 (61.6%) patients were females with female predominance 2:1 ratio, agreeing with data obtained by Gülen et al. [1] which stated that the median age of the patients was 53.1 (IQR = 36–64) years, and 63.8% (n = 212) of the total patients (332) were female and this may be attributed to the increased incidence of gallstones in females [1].
Acute pancreatitis is an inflammatory disease of the pancreas. The etiology and pathogenesis of acute pancreatitis have been intensively investigated for many years worldwide. There are multiple causes of acute pancreatitis which can be easily recognized. In developed countries, obstruction of the common bile duct by stones (38%) and alcohol consumption (36%) are the most frequent causes of acute pancreatitis. Gallstone-induced pancreatitis is caused by duct obstruction by gallstone migration. Obstruction is localized in the bile duct and pancreatic duct, or both [13]. The most frequent etiology in the current study is gallstones (76.8%).
In this study, we focused on the prognostic value of the neutrophil to lymphocyte ratio, LDH, and proteinuria in urine analysis to predict the severity of acute pancreatitis based on the classification by Ranson’s criteria scoring system; with respect to the relationship between NLR and systemic inflammatory response, multiple studies have recently investigated the relationships between NLR and outcome in a population of patients with acute pancreatitis. The utility of the NLR in acute pancreatitis was first investigated by Azab et al. [14]. They noticed that the NLR was a more sensitive parameter than total leukocyte counts in predicting ICU admission and longer hospitalization. Suppiah et al. [15] later revealed that NLR measured during the first 48 h of hospitalization was significantly associated with the risk of developing a severe form of acute pancreatitis (classified by 1992 Atlanta Criteria).
In the current study, after categorization of the patients according to Ranson’s criteria scoring system into low, mild, and high severity, we evaluate the prognostic value of the NLR both at the time of admission and 48 h after admission in the total population of the patients and calcular cause and non-calcular cause patients, and the P value at the time of admission was < 0.001 in total patients, 0.023 in non-calcular cause patients, and < 0.001 in calcular cause patients, while the P value of the NLR after 48 h of admission was < 0.001 in total patients, 0.003 in non-calcular cause patients, and < 0.001 in calcular cause patients that was statistically significant and consistent with other studies.
Interpretation of the data revealed that NLR both at the time of admission and after 48 h of admission can predict severity and also can effectively differentiate patients with mild and severe acute pancreatitis in both calcular and non-calcular cause-dependent acute pancreatitis patients.
Multivariate investigation showed that LDH and lipase at the time of admission had a great ability in predicting the outcome in patients with acute pancreatitis [16, 17].
In the current study, after categorization of the patients according to Ranson’s criteria scoring system into low, mild, and high severity, we evaluate the prognostic value of the LDH both at the time of admission and 48 h after admission in the total population of the patients, calcular cause- and non-calcular cause-dependent patients, and the P value at the time of admission was 0.001 in total patients, 0.079 in non-calcular cause patients, and 0.010 in calcular cause patients, while the P value of the LDH after 48 h of admission was 0.002 in total patients, 0.083 in non-calcular cause patients, and 0.020 in calcular cause patients. The interpretation of the data revealed that LDH results were statistically significant and can predict severity in calcular cause-dependent acute pancreatitis patients. However, it was statistically insignificant in non-calcular cause-dependent patients, and this is similar to the data obtained by Sharif et al. which stated that LDH and lipase at the time of admission could be paramount prognostic markers for predicting morbidity and mortality in patients with acute pancreatitis. However, the previously mentioned study did not divide patients into calcular and non-calcular cause-dependent pancreatitis [17].
Proteinuria in urine analysis was positive only in 15.2% of patients and the same result after 48 h of admission. There was no difference in the incidence of severe acute pancreatitis between patients with or without proteinuria and was similar to the results found by Zuidema et al. [18].
Conclusion
-
The neutrophil to lymphocyte ratio (NLR) is a simple, easily calculated systemic inflammation-based score which is calculated from the white cell differential count, gives a rapid impression of the extent of the inflammatory process, and can effectively predict severity at the time of admission and even after 48 h of admission and can also differentiate between patients with mild and severe acute pancreatitis in both calcular and non-calcular cause-dependent pancreatitis patients.
-
Lactate dehydrogenase (LDH) can be used to predict severity in calcular cause-dependent acute pancreatitis patients only at the time of admission and after 48 h of admission.
-
Proteinuria in urine analysis on admission and after 48 h does not seem to be a reliable predictor for disease severity in acute pancreatitis.
Recommendations
-
Early diagnosis, assessment of severity, and treatment of acute pancreatitis patients are a cornerstone in determining the overall morbidity and mortality.
-
All patients diagnosed with acute pancreatitis should be subjected to full history and examination; full laboratory investigation such as liver function test, coagulation profile, kidney function test, complete blood count, serum calcium level, serum sodium and potassium level, and albumin level; and assessment of the patient according to Ranson’s criteria scoring system.
-
All patients diagnosed with acute pancreatitis should be subjected to neutrophil to lymphocyte ratio (NLR) and lactate dehydrogenase (LDH) level as they provide an easy, early, and rapid prediction of the severity and adverse outcomes in patients with acute pancreatitis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- WBCs:
-
White blood cells
- APACHE-II:
-
Acute Physiology and Chronic Health Evaluation-II
- BISAP:
-
Bedside Index for Severity in Acute Pancreatitis
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- LDH:
-
Lactate dehydrogenase
- NLR:
-
Neutrophil to lymphocyte ratio
- SD:
-
Standard deviation
- Hgb:
-
Hemoglobin
References
Gülen B, Sonmez E, Yaylaci S, Serinken M, Eken C, Dur A, Turkdogan FT, Söğüt Ö (2015) Effect of harmless acute pancreatitis score, red cell distribution width and neutrophil/lymphocyte ratio on the mortality of patients with nontraumatic acute pancreatitis at the emergency department. World J Emerg Med 6(1):29
Bazerbachi F, Haffar S, Hussain MT, Vargas EJ, Watt KD, Murad MH, Chari S, Abu Dayyeh BK (2015) A systematic review of acute pancreatitis associated with interferon-α or pegylated interferon-α: possible or definitive causation? Pancreatology (7):691–699
Fonseca Sepúlveda EV, Guerrero-Lozano R (2018) Acute pancreatitis and recurrent acute pancreatitis: an exploration of clinical and etiologic factors and outcomes. J Pediatr (Rio J).
Barbara M, Tsen A, Rosenkranz L (2018) Acute pancreatitis in chronic dialysis patients. Pancreas. 47(8):946–951
Banks PA, Freeman ML (2006) Practice guidelines in acute pancreatitis. AmJ Gastroenterol. 101:2379–2400
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG et al (2013) Classification of acute pancreatitis (2012): revision of the Atlanta classification and definitions by international consensus. Gut. 62:102–111. https://doi.org/10.1136/gutjnl-2012-302779
Li XY, Wang XB, Liu XF, Li SG (2010) Prevalence and risk factors of organ failure in patients with severe acute pancreatitis. World J Emerg Med. 1:201–204
Wu BU, Johannes RS, Sun X, Tabak Y, Conwell DL, Banks PA (2008) The early prediction of mortality in acute pancreatitis: a large population-based study. Gut. 57:1698–1703
Park JJ, Jang HJ, Oh IY et al (2013) Prognostic value of neutrophil to lymphocyte ratio in patients presenting with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol. 111:636–642
Pichler M, Hutterer GC, Stoeckigt C et al (2013) Validation of the pre-treatment neutrophil-lymphocyte ratio as a prognostic factor in a large European cohort of renal cell carcinoma patients. Br J Cancer. 108:901–907
Kuo DC, Rider AC, Estrada P, Kim D, Pillow MT (2015) Acute pancreatitis: what’s the score? J Emerg Med. Jun 48(6):762–770
IBM_SPSS. Statistical Package for Social Science. Ver.21. Standard version. Copyright © SPSS Inc., 2011-2012. NY, USA. 2012
Lankisch PG, Assmus C, Lehnick D, Maisonneuve P, Lowenfels AB (2001) Acute pancreatitis: does gender matter? Dig Dis Sci. 46:2470–2474
Azab B, Jaglall N, Atallah JP, Lamet A, Raja-Surya V, Farah B, Lesser M, Widmann WD (2011) Neutrophil-lymphocyte ratio as a predictor of adverse outcomes of acute pancreatitis. Pancreatology. 11:445–452
Suppiah A, Malde D, Arab T, Hamed M, Allgar V, Smith AM, Morris-Stiff G.(2013): The prognostic value of the neutrophil–lymphocyte ratio (NLR) in acute pancreatitis: identification of an optimal NLR. Journal of Gastrointestinal Surgery. 1:17(4):675-81.
Hofmeyr S, Meyer C, Warren BL (2014) Serum lipase should be the laboratory test of choice for suspected acute pancreatitis. S. Afr. J. Surg. 52(3):34–38
Sharif A, Akhtar T, Akhtar M, Malik I, Hanif M, Zia N. (2018): Acute pancreatitis: role of lipase and LDH at admission as predictors of morbidity and mortality . AASCIT Journal of Health. May 1;5(3):65-69.
Zuidema MJ, van Santvoort HC, Besselink MG, van Ramshorst B, Boerma D, Timmer R, Bollen TL, Weusten BL. (2014): The predictive value of proteinuria in acute pancreatitis. Pancreatology. Nov 1;14(6):484-489.
Acknowledgements
Not applicable
Funding
Nil.
Author information
Authors and Affiliations
Contributions
LA made substantial contributions to the design of the work and the acquisition, analysis, interpretation of the data, and was a major contributor in revising the manuscript.
AIk made substantial contributions to the design of the work and supervising the work.
FRE is the corresponding author, has a major role in collecting the data and laboratory investigations of the patients in the study, had a major role in writing the manuscript, and had a major role in doing the statistical analysis of the data.
All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Review Board of Faculty of Medicine, Assiut University, and informed written consent was obtained from all participants according to the Declaration of Helsinki.
The committee’s reference number is not available.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmed, L.Aw., Kelani, AA.I.A. & Nasr-Allah, F.R.E. Evaluation of the prognostic value of the neutrophil to lymphocyte ratio, lactate dehydrogenase enzyme, and proteinuria in patients with acute pancreatitis admitted at Assiut University Hospitals and its correlation with Ranson’s criteria scoring system. Egypt J Intern Med 32, 5 (2020). https://doi.org/10.1186/s43162-020-00001-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43162-020-00001-4