Abstract
Background
Torsion of the appendix testis (TAT) is considered the most common cause of acute scrotum in childhood. When clinical and ultrasound (US) findings agree with the diagnosis, after testicular torsion has been excluded, conservative therapy is attempted whereas scrotal exploration and removal of the hydatid are required when medical therapy has failed. We hypothesized there are US features that can predict the failure of conservative therapy.
Methods
We conducted a retrospective analysis on pediatric patients treated for TAT. The age of patients, number of days spent with symptoms before the start of treatment, presence of epididymitis and/or hydrocele, and dimension of the twisted hydatid were analyzed. A search for a correlation between these variables and failure of conservative treatment was conducted.
Results
Patients were divided into 2 groups based on the efficacy of conservative management: responders (group I) and non-responders subjected to surgical treatment (group II). No statistically significant differences were registered in regard to age (p = 0.25), average dimension of hydatid (p = 0.09), and time gap between symptoms and the start of therapy (p = 0.92) between the 2 groups. An associated epididymitis was described in 27.5% of patients in group I and 41.7% in group II (p = 0.03; OR 1.89), and associated hydrocele was described in 33.4% of patients in group I and 45.8% in group II (p = 0.03; OR 1.83). Considering the odds ratios, the probability of surgical intervention when presenting only epididymitis without hydrocele is estimated to be 15%, when presenting only hydrocele without epididymitis: 9%, with both epididymitis and hydrocele: 74%, and without epididymitis nor hydrocele: 2%.
Conclusions
The presence of both epididymitis and hydrocele at first US evaluation is associated with a high probability of conservative treatment failure, thus predicting the need for surgical intervention.
Similar content being viewed by others
Background
Acute scrotum is enumerated among the most frequent acute surgical conditions in children [1,2,3,4,5,6,7,8,9,10,11,12].
Torsion of the appendix testis (TAT) is considered the most common cause of testicular swelling in childhood, accompanied by prominent clinical symptoms (acute pain, swelling, and redness) [13].
TAT presents with an almost similar history, although often the degree of pain is less severe compared to testicular torsion (TT). A bluish-black spot (blue-dot) may be seen through the skin at the upper pole of the testis, but this may not be apparent for 24 to 48 h after the development of symptoms, and palpation of this area causes extreme pain but usually in point tenderness fashion, whereas palpation of the testis itself causes little discomfort. The degree of inflammation of the epididymis is variable with testicular appendage torsion. Once secondary inflammation and edema of the scrotum occur, it may be impossible to distinguish between TT and TAT [14, 15].
Management is not universally accepted in all pediatric surgery centers. In many pediatric surgery units, medical therapy with non-steroid anti-inflammatory drugs (NSAIDs) is the first-line treatment for TAT; surgical removal is instead proposed in those patients with persistent scrotal pain thus not responding to NSAIDs [16,17,18,19]. For other authors, considering the tremendous consequences a misdiagnosed TT can lead to, treatment of acute scrotum, regardless of the underlying cause, is an immediate operative exploration in all cases, including TAT [15, 20]. Where the testis appears normally viable, its upper pole is manipulated into the wound, and the twisted hydatid is delivered through the incision and excised. Usually, this is a black pea after hemorrhagic infarction. A significant number of hydatids, however, undergo torsion without secondary hemorrhage and appear pale at surgery. These should always be excised and sent for pathologic confirmation of necrosis [15].
In our center, when clinical and ultrasound (US) findings agree with the diagnosis, after testicular torsion has been excluded, conservative therapy is attempted, and surgical removal of the hydatid is required only once medical therapy has failed.
The aim of the study is to discover clinical and US findings that, during the first clinical examination, may suggest an early surgical treatment instead of a conservative approach in case of torsion of testicular appendage.
Methods
Patients and study design
We conducted a retrospective analysis on all patients managed, admitted in our pediatric emergency department (Emergency Room, E.R.) for acute scrotum in a 15-year range period [2005–2020]. Being in a well-defined pediatric environment, all patients were less than 14 years old.
Patients with clinical and ultrasonographic diagnoses of isolated acute epididymitis (discharged) and patients with a suspicion of testicular torsion (explored immediately) were excluded.
Instead, we included patients with a clinical and ultrasonographic final diagnosis of twisted hydatid of Morgagni. All these patients were at first treated conservatively with medical therapy (ibuprofen 10 mg/kg three times a day for 4 days). Patients were invited to come back in case of failure of conservative treatment, defined as missed improvement or worsen symptomatology after at least 2 days of treatment. If failure of medical therapy occurred, clinical and US evaluation was repeated, and if the diagnosis was confirmed, patients were brought in the same day to the operating room for removal of the twisted hydatid. The maximum diameter of the twisted hydatid was measured with ultrasounds.
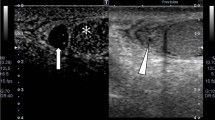
Epididymitis was defined in ultrasounds as an increase in epididymal volume, altered epididymal echogenicity, and increased peritesticular perfusion at Doppler interrogation, compared to the healthy contralateral (Fig. 1). US examinations were performed with a 13-MHz linear probe by 4 experienced pediatric radiologists working in the pediatric radiology service of our center. The radiologists had not been given the clinically suspected diagnosis of the surgeon before the US examination. A search for a correlation between these variables and failure of conservative treatment was conducted.
Thirteen megahertz linear probe ultrasounds. Comparison between a testis affected by TAT (A–C) and the contralateral one (D). A Maximum diameter of the twisted hydatid is measured (white dashed line). B Hydrocele (white star) secondary to the twisted hydatid is registered. C Epididymitis, defined as an increase in volume, echogenicity, and blood flow of epididymis compared to the healthy contralateral side (D)
Statistical analysis
Continuous data were presented as mean value ± standard deviation. The Shapiro–Wilk test was used to define if the data analyzed were normally distributed or not. Not normally distributed data were compared using a non-parametric test (Mann–Whitney U-test). A p-value < 0.05 was considered statistically significant. To study the association between the presence of hydrocele and epididymitis and the need for surgical interventions, the chi-square test was applied, and odds ratios were calculated.
Results
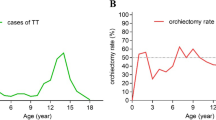
Between 2005 and 2020, 463 TATs were diagnosed and treated at our E.R. A total of 415 (89.6%) responded to conservative treatment and did not need any further treatment (group I), and 48 (10.4%) came back because of persistence and/or worsening of pain and were then operated (group II). The symptoms’ duration at first medical evaluation and age at diagnosis were not normally distributed; therefore, the U-test was applied. The average size of hydatids was 6.3 ± 2.4 mm (range: 2–13 mm) in group I and 8.0 ± 6.2 mm (range: 2–40 mm) in group II, but this difference was not statistically significant (p = 0.09). Group I patients got their first evaluation and therefore started medical therapy after an average of 1.7 ± 0.9 days (range: 0–7 days) while group II patients after 2.4 ± 1.0 days (range: 0–7 days), but no statistically significant difference was found (p = 0.92). The mean age was 10.2 ± 2.4 years old (range: 1–13 years old) in group I and 10.6 ± 2.1 years old (range: 1–13 years old) in group II, and no statistically significant difference was found (p = 0.25). An associated epididymitis was described in 27.5% of patients in group I and 41.7% in group II, and this difference was statistically significant (p = 0.03; OR 1.89). An associated hydrocele was described in 33.4% of patients in group I and 45.8% in group II, and this difference was statistically significant (p = 0.03; OR 1.83). Both epididymitis and hydrocele were registered in 15.6% of patients in group I and 30% in group II, and the difference was statistically significant (p = 0.02). Considering the ORs, it is possible to state that, according to our records, the probability of surgical intervention when presenting only epididymitis without hydrocele is estimated to be 15%, when presenting only hydrocele without epididymitis: 9%, with both epididymitis and hydrocele: 74%, and without epididymitis nor hydrocele: 2% (Fig. 2). Data are reassumed in Table 1.
Discussion
TAT is considered the most common cause of acute scrotum in children. Patients with TAT are usually younger than patients with TT and have also a longer duration of symptoms. Differential diagnosis with TT and epididymitis can be challenging [14, 21]. Mushtaq et al. reported a misdiagnosis rate of 12.5% in the case of TT, 17% for TAT, and 44% for epididymitis [22]. The literature remarks on the importance of US in enhancing the diagnostic power of clinical examination alone [23,24,25,26,27,28,29]. TAT’s clinical management is not homogenous across the world. Many surgeons prefer to attempt a conservative therapy with NSAIDs, thus leaving the surgical option only to those patients who do not respond to this strategy [16,17,18,19]. Others, as reported by Murphy et al., prefer to explore all cases of acute scrotum to minimalize testis damage [30]. In our center, we behave as the first ones when both clinical and US findings are strongly suggestive of TAT. To our knowledge, clinical or radiological signs that can predict a failure of conservative management are still missing. According to this lack of strong predictive factors in the literature, we retrospectively analyzed the clinical and US findings of our cohort of patients. The original idea was that twisted hydatid’s dimension could affect the response to conservative management because of a more difficult resorption and/or the greater inflammatory process involving the epididymis and testicular tunics, but no statistically significant results were observed. Another hypothesis we formulated is that, maybe, the later NSAIDs are started, the higher the risk of failure and, consequently, the chance of undergoing surgery: surprisingly, even if the operated group (group II) was diagnosed later than group I, the difference was not statistically significant. Summing up, NSAIDs have been successful in most patients (90%), even in those with very big, twisted appendages that received medical evaluation with a certain delay. On the contrary, our data suggested that cases that underwent surgery were the ones in which US documented a well-established epididymitis (p = 0.03), hydrocele (p = 0.03), or both (p = 0.02). Talking in terms of probability, according to our data, the chance of surgical intervention in the case of TAT when associated only with epididymitis without hydrocele is estimated to be 15%, when associated with hydrocele without epididymitis is 9%, with both epididymitis and hydrocele is 74%, and finally, an isolated TAT without epididymitis nor hydrocele has only a 2% chance of surgery (Fig. 2).
In other words, apparently, it does not matter how big the twisted appendix is nor the celerity of diagnosis, at least until the epididymis is significantly affected by an inflammatory process that associates with secondary hydrocele.
These results may suggest preferring a surgical first-line treatment in patients with TAT when presenting with both epididymitis and hydrocele.
Nevertheless, even if a more aggressive behavior is justified by the will of reducing the days of pain and discomfort of our little patients, looking carefully at our data, operating immediately all TATs with both epididymitis and hydrocele would determine a risk of 16% of unnecessary surgical treatment. This rate of avoidable procedures is too high in our opinion.
Moreover, an important limitation of our study is the too-subjective nature of the US description of epididymitis and hydrocele: if we accept that these findings may affect the surgical timing, we must ask radiologists to design a more objective description of these entities possibly with a severity grading scale. These struggles could reduce the number of unnecessary surgical interventions changing definitively the actual approach. Considering how US changed not only diagnostics but also operative procedures [23, 31,32,33] in the modern era, we believe surgeons should themselves dedicate to this technique and flank radiologists investigating the features we described in our paper.
Finally, what we can state with reasonable certainty after our analysis is that patients with TAT and associated hydrocele and epididymitis should be given a strict out-clinic follow-up due to the high risk of therapy failure.
Conclusion
Our retrospective analysis has no sufficient evidence to change the current approach to TAT.
Nevertheless, we find out that the presence of a well-established hydrocele and epididymitis, especially simultaneously, represents strong risk factors of conservative treatment failure whereas other apparently more intuitive features, such as dimensions of twisted hydatids or therapeutic delays, are not.
We think that a more objective and stratified US description of TAT-associated hydrocele and epididymitis may lead, in selected patients, to a change in the current approach encouraging early surgical treatment. Therefore, we invite radiologists with competence in the pediatric US, to cope with this limit.
An important take-home massage of our study is that patients with TAT and associated hydrocele and ependymitis deserve a strict follow-up protocol due to the high risk of failure of conservative treatment.
Availability of data and materials
Please contact the author for data requests.
Abbreviations
- NSAIDs:
-
Non-steroid anti-inflammatory drugs
- OR:
-
Odds ratio
- TAT:
-
Torsion of the appendix testis
- TT:
-
Testicular torsion
- US:
-
Ultrasound
References
Davenport M. ABC of general surgery in children. Acute problems of the scrotum BMJ. 1996;312(7028):435–7. https://doi.org/10.1136/bmj.312.7028.435.
Günther P, Rübben I. The acute scrotum in childhood and adolescence. Dtsch Arztebl Int. 2012;109(25):449–58. https://doi.org/10.3238/arztebl.2012.0449.
Hatch EI Jr. The acute abdomen in children. Pediatr Clin North Am. 1985;32(5):1151–64. https://doi.org/10.1016/s0031-3955(16)34899-4.
Tsalkidis A, Gardikis S, Cassimos D, et al. Acute abdomen in children due to extra-abdominal causes. Pediatr Int. 2008;50(3):315–8. https://doi.org/10.1111/j.1442-200X.2008.02578.x.
Erikci VS, Hoşgör M, Aksoy N, et al. Treatment of acute scrotum in children: 5 years’ experience. Ulus Travma Acil Cerrahi Derg. 2013;19(4):333–6. https://doi.org/10.5505/tjtes.2013.82783.
Parente G, Gargano T, Pavia S, et al. Pyelonephritis in pediatric uropathic patients: differences from community-acquired ones and therapeutic protocol considerations. A 10-year single-center retrospective study. Children (Basel). 2021;8(6):436. Published 2021 May 23.https://doi.org/10.3390/children8060436.
Brisighelli G, Consonni D, Macchini F, et al. A single-center experience with very low birth weight infants and focal intestinal perforation: comparison of primary anastomosis versus stoma opening. Eur J Pediatr Surg. 2018;28(5):426–32. https://doi.org/10.1055/s-0037-1605348.
Coles V, Elagami H, Bhandarker K, et al. The acute scrotum in infancy: a retrospective regional study. J Pediatr Urol. 2022;18(2):226–31. https://doi.org/10.1016/j.jpurol.2021.08.008.
Parente G, Di Mitri M, D’Antonio S, et al. Pelvic health assessment in adult females following pediatric appendicitis: a monocentric retrospective case-control study. Children (Basel). 2022;9(3):346. Published 2022 Mar 3.https://doi.org/10.3390/children9030346.
Marcozzi D, Suner S. The nontraumatic, acute scrotum. Emerg Med Clin North Am. 2001;19(3):547–68. https://doi.org/10.1016/s0733-8627(05)70203-0.
Di Mitri M, Parente G, Bonfiglioli G, et al. IL-6 serum levels can enhance the diagnostic power of standard blood tests for acute appendicitis. Children (Basel). 2022;9(10):1425. Published 2022 Sep 20. https://doi.org/10.3390/children9101425.
Thomas DFM. The acute scrotum in infancy: a retrospective regional study. J Pediatr Urol. 2022;18(2):232. https://doi.org/10.1016/j.jpurol.2021.10.021.
Papparella A, Fabiano N, Ferrante I, et al. Scroto Acuto. In: Lima M, Ruggeri G, editors. Chirurgia Pediatrica. Edises; 2015, p 498–503.
Gkalonaki I, Patoulias I, Anastasakis M, Panteli C, Patoulias D. The challenging diagnosis of acute scrotum: remaining difficulties and further insights. Folia Med Cracov. 2022;62(3):91–100. https://doi.org/10.24425/fmc.2022.142371.
Hutson JM. Undescended testis, torsion, and varicocele. In: Coran AG, Scott Adzick N, Laberge J, Shamberger RC, Caldamone AA, editors. Pediatric surgery.-7th edition, Elsevier Saunders; 2012, p 2543–2586.
Klin B, Zlotkevich L, Horne T, et al. A selective approach to the treatment of acute scrotum in children. Pediatr Surg Int. 1996;11(7):483–6. https://doi.org/10.1007/BF00180089.
Beck V, Grabbert M, Apfelbeck M, Schulz G, Stief CG, Tritschler S. Akutes Skrotum sofort abklären! [The acute scrotum - primary diagnostic approach and treatment]. MMW Fortschr Med. 2016;158(17):49–50. https://doi.org/10.1007/s15006-016-8779-7.
Gordhan CG, Sadeghi-Nejad H. Scrotal pain: evaluation and management. Korean J Urol. 2015;56(1):3–11. https://doi.org/10.4111/kju.2015.56.1.3.
Knight PJ, Vassy LE. The diagnosis and treatment of the acute scrotum in children and adolescents. Ann Surg. 1984;200(5):664–73. https://doi.org/10.1097/00000658-198411000-00019.
Miliaras D, Koutsoumis G & Vlahakis-Miliaras E. Appendix testis and appendix epididymis. Pediatr Surg Int. 1995; 10:241–242. https://doi.org/10.1007/BF00177169.
Boettcher M, Bergholz R, Krebs TF, et al. Differentiation of epididymitis and appendix testis torsion by clinical and ultrasound signs in children. Urology. 2013;82(4):899–904. https://doi.org/10.1016/j.urology.2013.04.004.
Mushtaq I, Fung M, Glasson MJ. Retrospective review of paediatric patients with acute scrotum. ANZ J Surg. 2003;73(1–2):55–8. https://doi.org/10.1046/j.1445-2197.2003.02612.x.
Herbener TE. Ultrasound in the assessment of the acute scrotum. J Clin Ultrasound. 1996;24(8):405–21. https://doi.org/10.1002/(SICI)1097-0096(199610)24:8%3c405::AID-JCU2%3e3.0.CO;2-O.
Laimer G, Müller R, Radmayr C, Lindner AK, Lebovici A, Aigner F. Multiparametric ultrasound in torsion of the testicular appendages: a reliable diagnostic tool? Med Ultrason. 2022;24(1):33–7. https://doi.org/10.11152/mu-3206.
Lim Y, Hwang J, Park J, Kim YC, Min SJ. A simplified ultrasound approach to diagnose testicular torsion and predict unsalvageable testis. Med Ultrason. 2022;24(3):305–13. https://doi.org/10.11152/mu-3507.
Bhatt S, Dogra VS. Role of US in testicular and scrotal trauma. Radiographics. 2008;28(6):1617–29. https://doi.org/10.1148/rg.286085507.
Shields LB, Daniels MW, Peppas DS, Rosenberg E. Sonography findings predict testicular viability in pediatric patients with testicular torsion. Cureus. 2022;14(1):e21790. Published 2022 Jan 31. https://doi.org/10.7759/cureus.21790.
Kylat RI, Ahmed MN. Neonatal testicular torsion. Afr J Paediatr Surg. 2022;19(1):1–4. https://doi.org/10.4103/ajps.AJPS_153_20.
Girgenti V, Pelizzo G, Amoroso S, et al. Emphysematous pyelonephritis following ureterovesical reimplantation for congenital obstructive megaureter. Pediatric case report and review of the literature. Front Pediatr. 2019;7:2. Published 2019. https://doi.org/10.3389/fped.2019.00002.
Murphy FL, Law H, Mushtaq I, Sebire NJ. Testicular and paratesticular pathology in infants and children: the histopathological experience of a tertiary paediatric unit over a 17 year period. Pediatr Surg Int. 2007;23(9):867–72. https://doi.org/10.1007/s00383-007-1959-x.
Sahlani L, Thompson L, Vira A, Panchal AR. Bedside ultrasound procedures: musculoskeletal and non-musculoskeletal. Eur J Trauma Emerg Surg. 2016;42(2):127–38. https://doi.org/10.1007/s00068-015-0539-3.
Parente G, Pinto V, Di Salvo N, et al. Preliminary study on the echo-assisted intersphincteric autologous microfragmented adipose tissue injection to control fecal incontinence in children operated for anorectal malformations. Children (Basel). 2020;7(10):181. Published 2020 Oct 13. https://doi.org/10.3390/children7100181.
Fu WX, Wang Q, Zhang YS, et al. Application of ultrasound technology in the diagnosis and treatment of digestive tract diseases. Eur Rev Med Pharmacol Sci. 2015;19(4):602–6.
Acknowledgements
Not applicable
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: NDS and MDM. Methodology: NDS, GP, and MDM. Software: GP. Validation: NDS and ML. Formal analysis: GP. Investigation: NDS, DB, ET, and MDM. Resources: NDS, GP, and ET. Data curation: NDS, ET, MDM, and DB. Writing—original draft preparation: NDS and MDM. Writing—review and editing: NDS, GP, MDM, and ML. Supervision: ML. Project administration: NDS. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of IRCCS Sant’Orsola Malpighi University Hospital (CHPED-04–20-IM). Informed consent was obtained from all subjects involved in the study.
Consent for publication
Written informed consent has been obtained from the patients to publish this paper.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salvo, N.D., Parente, G., Benivegna, D. et al. Ultrasound findings to predict failure of conservative treatment in the appendix testis torsion. Ann Pediatr Surg 19, 25 (2023). https://doi.org/10.1186/s43159-023-00258-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-023-00258-8