Abstract
Background
Nodular fasciits is thought to be a benign superficial nodular disease, which most often occurs in the medium age of adolescence, mainly in the subcutaneous or fascial plane on the upper extremities and trunk. The percentage of this entity in children compared to adults is less than 10%. Most cases in childhood were reported at the head and neck region, therefore often renamed to cranial or extracranial fasciitis. These lesions often consists of sarcoma like structures. Preoperative imaging is often unspecific and the standard of treatment in children is biopsy or in some cases complete resection with narrow margin depending on size or location of the lesion.
Case presentation
We present a clinical case of a female newborn with a congenital nodular presternal mass. Biopsy revealed nodular fasciits by testing on USP6 gen rearrangement. With ongoing growth of her nodular thoracic tumor, she underwent complete resection with primary closure. We followed her clinical course over more than 3 years and give a review of the literature.
Conclusion
Only a minority of reports are documented with a neonate onset and none with a real congenital. We hereby presented the first case in literature of a proven congenital fasciits other than cranial/extracranial in a newborn and her clinical course.
Similar content being viewed by others
Background
Nodular fasciitis is rare benign tissue proliferation [1] especially in children which appears often as a sarcoma or sarcoma like lesion. It was first described as a subcutaneous pseudosarcomatous fibrosis in 1955 by Kornwaler [2]. If diagnosed in early childhood it is mostly located at the head or neck region and therefore often named as cranial or extracranial fasciits [3] depending on site of location with a male predominance but also with reports of distribution patterns comparable to adults [3, 4]. Average onset is around age of three with sometimes history of prior trauma [5] or inflammatory or family disposition as risk factors. Treatment of choice was historically radical excision because of often rapid growth and clinical signs of malignancy. Today treatment consist at least of biopsy and molecular histological testing. Depending on laboratory results conservative treatment could nowadays be even justified [5,6,7,8].
Clinical case
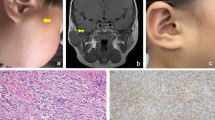
A female infant presented to our university hospital at 4 months of age with a painless nodule on her sternal chest wall. This fibrous nodule was already present at the time of delivery in the hospital and was examined by ultrasound by the local pediatrician on the same day. The first ultrasound diameter after delivery was 11 mm. Tentative diagnosis was arteriovenous malformation based on weak intralesional Doppler signals. Three months later, a follow-up examination revealed an increase in size of 16 mm and a surface diameter of 30 mm. She was referred to our department for further treatment with a diagnosis of arteriovenous malformation. At the first visit to our hospital, the mass was diagnosed as congenital dermatofibroma protuberans (Fig. 1), and a 4-mm punch biopsy was obtained. On reexamination 2 weeks later, the diagnosis of nodular fasciitis was confirmed histologically by USP6 gene FISH translocation analysis. With persistent slow progressive growth (Fig. 2), she was again referred to our plastic surgery department at one year of age. Considering possible spontaneous regression and benign pathology of the lesion, further surgical therapy was deferred for 1 year. At 2 years of age, she returned with a 5 × 3-cm livid plaque with indistinct margins. At the express request of the parents-even with evidence of some clinical regression-a complete narrow margin resection (Fig. 3) was planned because of the progressive growth and blurred margins. Further pathological analysis confirmed nodular fasciitis with USP6 gene rearrangement at the 17p13.2 gen locus. Two weeks later, she presented to our outpatient clinic with an allergic wound reaction and an incipient hypertrophic scar. One week later, we started silicone gel therapy after additional control. Six weeks postoperatively she came again for control. No recurrence of nodular fasciitis was seen, and we started silicone gel taping. One year after complete resection, there were still no clinical signs of recurrence.
Discussion
Nodular fasciits was first presented as a separate entity in 1955 as subcutaneous pseudosarcomatous fibrosis [2] and renamed to nodular fasciitis (NF) in 1961 [9]. Main predilection site in adults are the subcutaneous fat and fascia of upper extremities with lower prevalence in trunk, head and neck region and lower extremities [1, 10] with case reports of other rare locations. In contrary main predominance in younger children is the head and neck region [3] whereas in older children more comparable to adults [11] . Most commonly NF is mainly diagnosed in adults younger than 50 years of age (85%) with a spread sometimes up to 70 years and older [1] without gender predominance in older publications or up to 1.4:1 in recent [12]. Only 10% or less of all NF positive confirmed cases has been reported on children [12] with an estimated male ratio up to 2:1 [13] but other series state no gender preference [3]. In actual literature number of patients with nodular fasciits (NF) other than cranial/extracranial presenting congenital is zero and with cranial fasciitis during first days of life is extremely low [14, 15] and number of NF at other places than head and neck region in early newborns is limited to a single case report in the literature [16]. NF in early childhood presents often as a subcutaneous nodule with fast growing within 2–4 weeks unilateral and mainly solitary [12]. Most often, the nodule is firm, fixed and painless. Imaging with Doppler ultrasound reveals normally no to week detectable Doppler signals with an “fascial tail sign” on sonography [17]. MRI and CT scans are often stated unspecific [18], but with specific “cloud sign” in recent publication on MRI [19] and one report in literature which demonstrates intense vascularity on angiography [20]. Histologically specimen imitate sarcoma like type of tumors like dermatofibroma protuberans, spindle cell sarcoma, fibrosacroma, myofibroblastic sarcoma, desmoid-type fibromatosis, or inflamed cyst at early age [21, 22]. It presents often as a self-limiting, reactive proliferation of fibroblasts and myofibroblasts with sometimes infiltration of bone and muscles. Pathogenesis was stated unknown in the past as a putative reactive process as 10–15% of known reports reveals a history of trauma or infection in elderly. Today’s most common accepted origin is a rearrangement of the USP6-gen which drives the tumor [23]. Therefore, on molecular level a distinction between NF en sarcomas is possible which facilitates further treatment decisions. Tumors with USP6 gen rearrangement are benign and conservative excision- which is actually standard treatment of choice by clinical easily visibly margins—to avoid overtreatment seems to be possible in NF even in especially aggressive growing tumors. The actual most emphasized treatment in children with this type of rapid growing masses is sonographic control in superficial lesions with biopsy at early clinical presentation and surgical resection with keeping functional structures intact. If other treatment options like local corticosteroid injections [24] or systemic corticosteroids are helpful in children is somewhat speculative because of its mostly solitary aspect, the fast growth and the need to biopsy compared to the sometimes multiple lesions in adults [25]. To our best knowledge, this is the first case of a proven congenital nodular fasciitis of the skin and the first case of such a congenital pediatric lesion of the trunk.
Conclusions
Congenital nodular fasciits is an extremely rare benign entity, which appears like a sarcoma type lesion which easily can misdiagnosed and occurs most often around the head/neck region in newborns. Preoperative ultrasound can be helpful. To avoid unaesthetically surgical overcorrection we advise biopsy and USP6 gene mutation analysis. With a confirmed diagnosis of true nodular fasciitis by molecular gen testing treatment should be watch and wait except possible live threatening conditions in faster growing tumors. With demanding parents a near complete resection should be appropriate and recurrence is unlikely.
Availability of data and materials
All data and material is available
References
Bernstein KE, Lattes R. Nodular (pseudosarcomatous) fasciitis, a nonrecurrent lesion: clinicopathologic study of 134 cases. Cancer. 1982;49(8):1668–78.
Konwaler BE, Keasbey L, Kaplan L. Subcutaneous pseudosarcomatous fibromatosis (fasciitis). Am J Clin Pathol. 1955;25(3):241–52.
Hseu A, et al. Pediatric nodular fasciitis in the head and neck: evaluation and management. JAMA Otolaryngol Head Neck Surg. 2015;141(1):54–9.
Stout AP. Pseudosarcomatous fascitis in children. Cancer. 1961;14:1216–22.
Strazzula L, et al. Child abuse masquerading as a soft tissue sarcoma. Pediatr Dermatol. 2014;31(6):708–11.
Bemrich-Stolz CJ, et al. Single institution series of nodular fasciitis in children. J Pediatr Hematol Oncol. 2010;32(5):354–7.
Stanley MW, et al. Nodular fasciitis: spontaneous resolution following diagnosis by fine-needle aspiration. Diagn Cytopathol. 1993;9(3):322–4.
Majumdar B. Spontaneously regressing nodular fasciitis of the neck. J Laryngol Otol. 1983;97(10):973–7.
Price EB Jr, Silliphant WM, Shuman R. Nodular fasciitis: a clinicopathologic analysis of 65 cases. Am J Clin Pathol. 1961;35:122–36.
Shimizu S, Hashimoto H, Enjoji M. Nodular fasciitis: an analysis of 250 patients. Pathology. 1984;16(2):161–6.
Pandian TK, et al. Nodular fasciitis in the pediatric population: a single center experience. J Pediatr Surg. 2013;48(7):1486–9.
Lu L, et al. Nodular fasciitis: a retrospective study of 272 cases from China with clinicopathologic and radiologic correlation. Ann Diagn Pathol. 2015;19(3):180–5.
Tomita S, et al. Nodular fasciitis: a sarcomatous impersonator. J Pediatr Surg. 2009;44(5):e17–9.
Lang DA, et al. Cranial fasciitis of the orbit and maxilla: extensive resection and reconstruction. Childs Nerv Syst. 1996;12(4):218–21.
Svrakic M, Bent JP 3rd, Adler E. Neonatal nodular fasciitis of the larynx. Int J Pediatr Otorhinolaryngol. 2009;73(7):1007–9.
Lao I, et al. Infantile nodular fasciitis of the hand: A case report and literature review. Human Pathol. 2016;5:43–6.
Khuu A, et al. Nodular fasciitis: characteristic imaging features on sonography and magnetic resonance imaging. J Ultrasound Med. 2014;33(4):565–73.
Meyer CA, et al. MR and CT appearance of nodular fasciitis. J Comput Assist Tomogr. 1991;15(2):276–9.
Wu SY, et al. MR imaging features and a redefinition of the classification system for nodular fasciitis. Medicine (Baltimore). 2020;99(45):e22906.
Koenigsberg RA, et al. Nodular fasciitis as a vascular neck mass. AJNR Am J Neuroradiol. 1996;17(3):567–9.
Handa Y, Asai T, Tomita Y. Nodular fasciitis of the forehead in a pediatric patient. Dermatol Surg. 2003;29(8):867–8.
Shields JA, et al. Orbital nodular fasciitis simulating a dermoid cyst in an 8-month-old child. Case report and review of the literature. Ophthalmic Plast Reconstr Surg. 2001;17(2):144–8.
Malik F, et al. Benign infiltrative myofibroblastic neoplasms of childhood with USP6 gene rearrangement. Histopathology. 2020;77(5):760–8.
Keren S, et al. The management of periorbital nodular fasciitis using intra-lesional triamcinolone: a case report and review of the literature. Orbit. 2021;40(4):333–7.
Graham BS, Barrett TL, Goltz RW. Nodular fasciitis: response to intralesional corticosteroids. J Am Acad Dermatol. 1999;40(3):490–2.
Acknowledgements
None
Funding
None
Author information
Authors and Affiliations
Contributions
The corresponding author wrote the manuscript and approved it. The second author was involved in correction and support. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable in case reports/not required
Consent for publication
Both parents of the patient gave informed consent to use clinical photographs
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wagner, T., Ulrich, D. Congenital nodular fasciitis: an extremely rare entity with review of literature. Ann Pediatr Surg 18, 64 (2022). https://doi.org/10.1186/s43159-022-00204-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-022-00204-0