Abstract
Background
Yolk sac tumor or endodermal sinus tumor is an uncommon malignant germ cell neoplasm. This tumor usually presents in childhood or young adulthood as a testicular or ovarian mass. Extragonadal sites such as mediastinal, intracranial, and sacrococcygeal have been described. A review of the literature revealed limited related cases. The clinical presentation, radiographic characteristics, operative findings, and patient outcomes are discussed.
Case presentation
We report the occurrence of a primary paraspinal germ cell tumor in a 28-month-old boy who presented with thoracic spinal cord compression. The patient presented with pain, weakness, paraplegia, and bowel and bladder disturbances.
MRI was done and showed a retroperitoneal and paravertebral mass invading the left diaphragmatic crus, the lateral neural foramen, and the posterior paravertebral muscles. Morphologic and immunohistochemical features were consistent with a germ cell tumor, namely an endodermal sinus tumor (yolk sac) of the epidural area. The final diagnosis was determined to be stage IV extragonadal germ cell tumor. The patient underwent emergency surgery consisting of T10–12 laminectomy and epidural mass resection with the release of the spinal cord compression and received chemotherapy consisting of cisplatin, bleomycin, and etoposide. After six cycles of chemotherapy, follow-up MRI showed complete resolution of the tumor. The patient has been in complete remission 16 years from his initial diagnosis. He still, however, has mild residual weakness in both lower extremities and some detrusor-sphincter dyssynergia.
Conclusion
Extragonadal germ cell tumors presenting with spinal cord compression are rare; however, they should be included in the differential diagnosis of every child younger than 3 years old who does not present with the typical features. Germ cell tumors are sensitive to platinum-based chemotherapy, and surgery should only be performed for spinal cord compression and for obtaining tissue biopsy for a definitive diagnosis. The sooner the decompression is done, the better neurological outcome is achieved. Long-term remission, and possibly cure, can be achieved with a multidisciplinary treatment strategy.
Similar content being viewed by others
Background
Malignant germ cell tumors are relatively uncommon in children, accounting for approximately 3% of all childhood malignancies [1]. Yolk sac tumor or endodermal sinus tumor (EST) primarily originates from the testes or the ovaries. In 2–5% of cases, it originates from extragonadal sites involving posterior midline structures in the mediastinal, retroperitoneal, and sacrococcygeal areas and intracranially in the suprasellar and pineal regions [2, 3]. Gonadal sites predominate in children older than 3 years old and adolescents, while extragonadal tumors are more common in neonates and infants [4].
Spinal cord compression from EST is rare. Systemic EST has occasionally been reported to metastasize to the spine [3]. There are few previously reported cases of EST in children and adults presenting with spinal cord compression [2, 3, 5,6,7]. In this article, we report a 28-month-old boy with primary EST located in the retroperitoneal region presenting with thoracic spinal cord compression.
Case presentation
A 28-month-old boy with unremarkable past medical history began having pain and weakness in the left lower extremity for 3 weeks prior to presentation, with rapid progression to paraplegia over a few days. Physical examination upon arrival showed flaccid total paralysis (grade 0/5 in bilateral lower limb, except right hip flexors) and absent sensations in the lower extremities (L1 sensory level) (grade 0/5). Weak right hip flexion to severe pain was still present (grade 1/5 for right hip flexors). The patient also had bowel and bladder disturbances.
Laboratory workup revealed normal electrolytes, uric acid, liver and renal function tests, mild anemia, and an LDH level of 589 IU/ml. Urine VMA and HVA were normal, and NSE was 21 ng/ml (Nl < 16.3).
Initial MRI showed a 4 × 3 × 2.5 cm retroperitoneal and paravertebral mass invading the left diaphragmatic crus, the lateral neural foramen, and the posterior paravertebral muscles (Fig. 1a). The tumor surrounded the T10 vertebral body with intraspinal extension and compression of the spinal cord and bone erosion of the vertebral bodies of T10 and T11 on the left side (Fig. 1b). Chest CT scan revealed a 6-mm nodule in the right lung (Fig. 2). Abdominal CT scan did not detect any metastases in the liver. Bone scan was normal, and bilateral bone marrow biopsies were negative for malignancy.
a and b MRI of the mass. MRI showed a 4 × 3 × 2.5 cm retroperitoneal and paravertebral mass invading the diaphragmatic crus, the lateral neural foramen, and posterior paravertebral muscles. The tumor was surrounding the T10 vertebral body with intraspinal extension and compression of the spinal cord and bony erosion of the vertebral bodies of T10 and T11 on the left side
The patient underwent emergency surgery consisting of T10–12 laminectomy and epidural mass resection of the dumbbell-shaped tumor with release of the spinal cord compression.
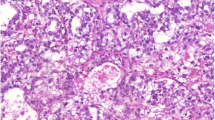
Pathology showed a malignant proliferation consisting of clusters of oval and round cells with a spindle cell component. The nucleoli were prominent, and the cytoplasm was well outlined, presenting rare vacuoles and PAS positive intracytoplasmic inclusions. Necrosis was present. The tumor tissue infiltrated and destroyed bone and cartilage. It also infiltrated adipose tissue, striated muscle, capsule, and ligaments. The tumor cells were arranged in patterns that included a predominant reticular and microcystic pattern, a macrocystic and papillary pattern, a perivascular festooned and papillary pattern that edifies Schiller-Duval bodies, and a solid and sarcomatoid pattern. There was an arrangement of cylindrical cells suggestive of intestinal or endometrioid differentiation: the stroma was loose, myxoid and rarely fibrous.
Immunohistochemistry showed positive immunoreactivity with cytokeratin, vimentin, chromogranin, AFP (strong positivity), and CD30 and negative immunoreactivity with Beta HCG, EMA, NSE, PLAP, and P53. All these morphological and immunohistochemical features were consistent with a germ cell tumor, namely an endodermal sinus tumor (yolk sac) of the epidural area. The immunoreactivity with CD30 raised the point of focal differentiation of embryonal carcinoma which was ruled out by the absence of immunoreactivity with PLAP.
Further blood investigations showed elevated alpha fetoprotein (AFP) at 6285 UI/ml (Nl < 10 UI/ml) confirming the presence of yolk sac elements in the tumor. Beta-HCG was 0 mUI/ml, CEA was normal at 1.59 ng/ml (Nl < 10 ng/ml), and CA-125 was 23.7 UI/ml (Nl < 35 UI/ml).
Testicular ultrasound and Brain CT scan with contrast did not demonstrate any abnormalities.
The final diagnosis was determined to be stage IV and high-risk extragonadal germ cell tumor as per the Children’s Oncology Group (COG) staging and risk stratification. The patient received chemotherapy consisting of cisplatin 40 mg/m2 days 1–5, bleomycin 15 mg/m2 day 1, and etoposide 100 mg/m2 days 1–5.
During chemotherapy, the evaluation was done by imaging studies for the tumor and metastatic site, in addition to serum AFP monitoring. Re-evaluation after two cycles showed an excellent response with 50–60% decrease in the size of the residual retroperitoneal and intrathoracic tumor. The lung nodule disappeared. The patient received two additional cycles of chemotherapy with a further decrease of the tumor by 90%. After the second chemotherapy cycle, AFP decreased to 370, and then returned to normal levels (9.35) after the fourth cycle of chemotherapy. The administered chemotherapy was relatively well tolerated, except for grade IV hematologic toxicity and a renal Fanconi syndrome secondary to cisplatin after the fourth cycle of treatment. This resolved progressively after electrolyte supplementation. The patient also underwent physical therapy which resulted in improvement of his gait.
He received two additional cycles of chemotherapy with a 50% reduction of the cisplatin dose (total of six cycles of chemotherapy). Follow-up MRI showed complete resolution of the tumor with mild kyphosis. He has been in complete remission sixteen years from his initial diagnosis. He still, however, has mild residual weakness in both lower extremities and some detrusor-sphincter dyssynergia.
Discussion
Endodermal sinus tumors (EST) are the most common histologic subtype of malignant germ cell tumors with a high degree of malignancy [8]. They may originate either from the gonads or from extragonadal organs and tissues. The exact pathogenesis of extragonadal germ cell tumors is unknown, but it has been suggested that the malignancy process starts during the early embryological days. It is explained by an abnormal migration of primordial germ cells. The primordial cells located in the midline of the embryo are thought to be affected during this period and develop a malignant tumor later [9, 10]. Extragonadal EST can occur in the mediastinum, the retroperitoneal, presacral, and intracranial regions [8]. A recent report described a primary yolk sac tumor from the spinal cord [11].
The main considerations in the differential diagnosis of masses in the posterior mediastinum, particularly in the paravertebral region, include neurogenic masses, lymphoma, paravertebral abscess, lateral meningocele, and extramedullary hematopoiesis [12].
Table 1 summarizes some of the cases found in the literature of EST presenting with spinal cord compression.
Although some authors believe that extragonadal germ cell tumors are biologically distinct from their testicular counterparts [13], other investigators who evaluated the imprinting status of gonadal and nongonadal pediatric germ cell tumors have found a common precursor cell for these tumors [14].
Cytogenetic data on extragonadal germ cell tumors in children have shown cytogenetic differences from their adult counterparts [15,16,17].
The cytogenetic finding of one or multiple copies of the short arm of chromosome 12p with the loss of the long arm of chromosome 12 is seen in nearly all germ cell cancers of primary gonadal and extragonadal origin [9]. The molecular changes associated with the development of germ cell tumors are still not clearly understood; however, it is clear from the universal cytogenetic finding of increased 12p copy number that this chromosomal change is a key event [9]. Of particular interest is an amplification of the proximal 12p11.2–12 region which includes the genes ras-k2, SOX5 and JAW1, and cycline CCND2 mapped to the 12p13 region, which could be the best candidate for the 12p3 gene in normal testicular genesis and malignant germ cell development and growth [9].
The prognosis of a malignant germ cell tumor depends on the size of the tumor, the presence of the liver, brain, or mediastinal metastases, the serum lactate dehydrogenase (LDH) level, and the presence of choriocarcinoma in the primary tumor [18].
Management depends on the staging of the disease. It usually consists of surgical resection, chemotherapy, and, in some cases, radiotherapy.
The management of tumors with spinal cord compression is slightly more complicated and requires a rapid diagnosis and treatment to prevent irreversible damage [7]. Several signs indicate compression, such as motor or sensory weakness in lower extremities and bowel or bladder dysfunction. Both of them were found in our patient [7].
Because this event is so rare, there is no consensus regarding the best therapeutic approach. The first aim should be the preservation of the neurologic function and the second is obtaining a histologic specimen. The management of EST causing cord compression in the reported cases was surgical decompression followed by chemotherapy. Neurosurgical decompression is used in cases who show rapidly progressive neurological defects and recent onset neurologic dysfunction [3]. This is done to avoid permanent damage. However, if this isn’t the case, surgery should be avoided to decrease the incidence of spinal deformities and instabilities after laminectomy [3]. Survival rates of pediatric GCTs have been improved significantly up to 80% in patients who receive platinum-based chemotherapy [7]. Chemotherapy should be used as an initial management in children with spinal cord compression from EST as this would limit complications from radiotherapy and laminectomy [3].
Radiation therapy for spinal cord compression in children must be carefully considered because of the potentially irreversible complications such as spinal deformity, neurological sequelae, and secondary malignant diseases such as radiation induced lymphoma [7].
Pashankar et al. reported that they used a different method. After performing a biopsy of the paraspinal mass, they opted to use only chemotherapy without laminectomy or radiation therapy to shrink the epidural mass. With this approach, they had excellent tumor response and a complete neurologic recovery despite a near-complete paraplegia at presentation. However, neurologic function was to be monitored closely, and frequent imaging was conducted to ensure there was no tumor recurrence [3]. The long-term outcome of this therapy remains unknown.
Recent studies showed the importance of using steroid treatment after direct surgical decompression in order to prevent secondary injury caused by posttraumatic spinal ischemia [7]. It has also been shown to improve neurologic function and spinal cord blood flow [7].
In our case, there was no doubt that the spinal cord compression needed to be relieved immediately. The question remained whether further surgery on the residual tumor should be attempted initially followed by chemotherapy or whether chemotherapy should be attempted first. Because this tumor is known to be chemosensitive, we opted to start with two cycles of chemotherapy, assess the clinical and radiological response and then decide for the best timing of subsequent surgery. Because of the spectacular response observed in this patient, chemotherapy was continued to facilitate the surgery and decrease surgical morbidity. After six cycles of chemotherapy, there was a complete resolution of the tumor on follow-up MRI, and further surgery or radiotherapy was not needed. The child is still in complete remission 16 years from the last chemotherapy with only mild residual weakness in both lower extremities and some detrusor-sphincter dyssynergia. It is remarkable that the patient was able to recover from his almost-lost neurologic functions even though he was brought to treatment in a tardive manner, several weeks after loss of motor function in the lower extremities.
Conclusion
Tumors presenting with spinal cord compression in early childhood include neuroblastoma, sarcoma, and, rarely, extragonadal germ cell tumors. Germ cell tumors should be suspected in children presenting with signs of spinal cord compression, and serum AFP assessment could be helpful in orienting the diagnosis. Germ cell tumors are very sensitive to chemotherapy, as shown in our case, and aggressive surgery should be avoided in these patients. Surgery remains indicated for urgent spinal cord decompression, to achieve a better neurological outcome in cases with rapidly deteriorating neurological function. An accurate pathological diagnosis is also essential to define an appropriate treatment plan for the patient and to optimize the chances of cure. Long-term remission, and possibly, cure can be achieved with a multidisciplinary treatment strategy.
Availability of data and materials
Not applicable.
Abbreviations
- EST:
-
Endodermal sinus tumor
- LDH:
-
Lactate dehydrogenase
- VMA:
-
Vanillylmandelic acid
- HLA:
-
Human leukocyte antigen
- NSE:
-
Neuron-specific enolas
- NI:
-
Normal index
- MRI:
-
Magnetic resonance imaging
- PAS:
-
Periodic acid Schiff
- AFP:
-
Alpha-fetoprotein
- EMA:
-
Eosin-5′-maleimide
- PLAP:
-
Placental alkaline phosphatase
- Beta-HCG:
-
Beta human chorionic gonadotropin
- CEA:
-
Carcinoembryonic antigen
- CT:
-
Computed tomography
- GCT:
-
Germ cell tumor
References
Rescorla FJ, Breitfeld PP. Pediatric germ cell tumors. Curr Probl Cancer. 1999;23(6):257–303.
Guzel A, Tatli M, Belen D, Seckin H. Spinal cord compression of primary extragonadal giant yolk sac tumor. Spinal Cord. 2007;45(3):254–7.
Pashankar FD, Steinbok P, Blair G, Pritchard S. Successful chemotherapeutic decompression of primary endodermal sinus tumor presenting with severe spinal cord compression. J Pediatr Hematol Oncol. 2001;23(3):170–3.
Pai MR, Baliga PB, Naik R. Extragonadal germ cell tumours in Mangalore with review of the literature. J Indian Med Assoc. 1996;94(8):294–295, 310.
Resnick DK, McLaughlin MR, Albright AL. Primary endodermal sinus tumor presenting with spinal cord compression. Case Re J Neurosurg. 1997;86(1):151–3.
Todani T, Watanabe Y, Toki A, Urushihara N, Sato Y. Endodermal sinus tumour of the posteroinferior mediastinum resembling dumbbell neuroblastoma in a child. Z Kinderchir. 1990;45(2):120–2.
Yon DK, Ahn TK, Shin DE, et al. Extragonadal germ cell tumor of the posterior mediastinum in a child complicated with spinal cord compression: a case report. BMC Pediatr. 2018;18:97. https://doi.org/10.1186/s12887-018-1070-6.
Davidoff AM, Hebra A, Bunin N, Shochat SJ, Schnaufer L. Endodermal sinus tumor in children. J Pediatr Surg. 1996;31:1075–8.
Schmoll HJ. Extragonadal germ cell tumors. Ann Oncol. 2002;4:265–72.
Nichols CR. Extragonadal and pediatric germ cell tumors. Hematol Oncol Clin North Am. 1991;5(6):1189–209.
Kurisaka M, Moriki A, Mori K, Sonobe H. Primary yolk sac tumor in the spinal cord. Childs Nerv Syst. 1998;14:653–7.
Marchiori E, Hochhegger B, Zanetti G. Paravertebral mass. J Bras Pneumol. 2018;44(5):352. https://doi.org/10.1590/s1806-37562018000000256.
Hsu YJ, Pai L, Chen YC, Ho CL, Kao WY, Chao TY. Extragonadal germ cell tumors in Taiwan: an analysis of treatment results of 59 patients. Hsu YJ, Pai L, Chen YC, Ho CL, Kao WY, Chao Y. Cancer. 2002;95(4):766–74.
Schneider DT, Schuster AE, Fritsch MK, Hu J, Olson T, Lauer S, et al. Multipoint imprinting analysis indicates a common precursor cell for gonadal and nongonadal pediatric germ cell tumors. Schneider DT, Schuster AE, Fritsch MK, Hu J, Olson T, Lauer S, Gobel U, Perlman EJ. Cancer Res. 2001;61(19):7268–76.
Jenderny J, Koster E, Borchers O, Meyer A, Grote W, Harms D, et al. Interphase cytogenetics on paraffin sections of paediatric extragonadal yolk sac tumours. Virchows Arch. 1996;428(1):53–7.
Perlman EJ, Cushing B, Hawkins E, Griffin CA. Cytogenetic analysis of childhood endodermal sinus tumors: a Pediatric Oncology Group study. Pediatr Pathol. 1994;14(4):695–708.
Hoffner L, Deka R, Chakravarti A, Surti U. Cytogenetics and origins of pediatric germ cell tumors. Cancer Genet Cytogenet. 1994;74(1):54–8.
Kawakita M, Terachi T, Hida S, Takeuchi H, Yoshida O. Survival and prognostic factors associated with metastatic nonseminomatous testicular and extragonadal germ cell tumors. Int J Urol. 1994;1(2):172–6.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
RF: the pediatrician who diagnosed and followed the case. Also helped with literature review and writing of the case report. JM: literature review and writing of this case report. AM: literature review and in writing this case report. NBD, from the Department of Pathology who performed the histological examination. IS: The neurosurgeon who performed the operation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Approved.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Farah, R.A., Matta, J.K., Metri, A.A. et al. Extragonadal germ cell tumor presenting with spinal cord compression: a case report and literature review. Ann Pediatr Surg 18, 36 (2022). https://doi.org/10.1186/s43159-022-00173-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-022-00173-4