Abstract
Background
Pneumoperitoneum is defined as the presence of free air in the peritoneal cavity. It is a surgical emergency that represents in 90% of the cases with a hollow viscus perforation and its feared consequences of sepsis and death. On the other hand, spontaneous pneumoperitoneum is a benign surgical entity occurring in newborns that requires no surgical intervention.
Cases presentation
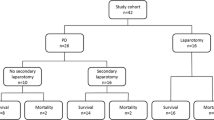
In this series, we report three cases of benign spontaneous pneumoperitoneum in neonates treated at Jordan University Hospital between 2004 and 2021. Two of them were treated by exploration laparotomy but no gross pathology could be identified; one case was successfully treated conservatively with observation alone.
Conclusion
This case series recognizes the presence of such entity which can be treated conservatively, eliminating the unnecessary burden of morbidity and mortality of surgery in such age group.
Similar content being viewed by others
Introduction
Pneumoperitoneum, or gas in the peritoneal cavity, represents a surgical emergency in adults and paediatric age groups. In the majority of cases (>90%), pneumoperitoneum occurs as a result of a perforated intra-abdominal viscus [1]. The entity of ‘benign’, ‘spontaneous’, ‘non-surgical’, ‘asymptomatic’, or ‘idiopathic’ pneumoperitoneum has been reported in the literature, which when recognized requires conservative measures to resolve only.
After reviewing the literature, we found several reported cases supporting watchful waiting of this entity [1,2,3,4] with favourable outcomes in relation to decreased hospital stay and avoidance of unnecessary laparotomies with its related morbidity and mortality. Some studies suggested the insertion of a peritoneal drain as a bridging procedure for surgery to gain some health and stability of the newborn, especially in low-birthweight and very-low-birthweight neonates that cannot tolerate the impact of surgery [5]. Studies have reported no significant difference in mortality between infants treated with laparotomy or peritoneal drain placement when the diagnosis was NEC [6]. Another reported measure in literature for the treatment of spontaneous pneumoperitoneum is one-time abdominocentesis by insertion of an 18G cannula in the right hypochondrial region at the midclavicular line and then aspiration of abdominal gas; the neonate is then followed for the resolution of pneumoperitoneum.
The decision to go for operative exploration cannot be made solely on the mere presence of pneumoperitoneum, when no signs of peritonitis or laboratory findings that suggest a much gravid aetiology has been identified. Studies have suggested an algorithm to select those that go into surgery and those that can be treated conservatively [3, 7]. The indications for surgical intervention in pneumoperitoneum are the features of peritonitis, pain, cardiovascular instability, leukocytosis, evidence of leakage from the gastrointestinal tract, and failure of conservative management [8].
Different theories have been made to explain the pathophysiology of spontaneous pneumoperitoneum. In cases of increased intra-thoracic pressure, it is assumed that air dissects its way downwards along the oesophagus and aorta into the retroperitoneal tissue [5]. It can also pass through a posterolateral defect of the diaphragm secondary to arrest in the closure of the pleuroperitoneal canal and diaphragmatic defects at the sternocostal and lumbo-costal region as described by Gummalla et al. [4]. Other studies suggest the presence of micro-perforations in the anterior wall of the stomach, ranging between 2 and 4 mm in diameter, for pneumoperitoneum to occur [9].
We report in this series three patients who were treated at Jordan University Hospital, at the period between 2004 and 2021, adding to the work reported by Al-lawama et al. at the same hospital in 2016 [7].
Case 1
A 1-day-old male neonate, 34+3 weeks of gestation, who was delivered by caesarean section with a birth weight of 2340 g and an APGAR score of 8 and 9 at 1 and 5 min, respectively. The infant was admitted to the neonatal intensive care unit (NICU) due to respiratory distress syndrome and was managed by elective intubation. A chest X-ray showed severe perihilar infiltrates bilaterally with a fine granular pattern picture suggestive of transient tachypnoea of the newborn (TTN). On the next day, he was extubated and kept on non-invasive positive pressure ventilation device (NIPPV). At the same day, an abdominal X-ray (Fig. 1a) was done due to abdominal distension, which showed dilated bowel loops associated with free intra-abdominal air. Upon physical examination, the patient had normal vital signs for his age, the skin colour of his abdomen was not erythematous, the abdomen was distended and tense, and the bowel sounds were audible. His white cell count was 6000 with 70% neutrophils. The infant did not vomit, he passed stool four times prior to presentation. Therefore, a diagnosis of spontaneous pneumoperitoneum was made, and the decision was to keep the infant NPO on TPN, and to insert a cannula (20 G) at the right lower quadrant through his abdominal wall reaching the peritoneal cavity, to deflate the abdomen and observe for any faecal materials discharging through cannula, which would be suggestive of bowel perforation. The cannula was kept for 24 h open to free air then removed, no discharge from the cannula could be detected. Follow-up abdominal X-ray (Fig. 1b) showed gastric distension and persistent pneumoperitoneum; therefore, a gastrografin follow-through was ordered (Fig. 1c), and it showed free intraperitoneal air and passage of contrast from the stomach through small bowel loops with evidence of contrast extravasation that appeared more evident on 10 min images after contrast introduction and build-up on sequential imaging, suggesting small bowel perforation with a probable site of leak from the duodenum or proximal jejunum. The evidence of contrast leak radiologically shifted the management plan from conservative to urgent laparotomy the same day. Intraoperatively, the stomach was inflated with gas, yet no perforation could be identified, and the small intestine was explored with methylene blue dye injection intra-luminal but no visible leak from a bowel wall perforation was identified, the large intestine was free as well, rest of bowel was grossly healthy, so the closure of abdomen with no further intervention was carried out.
The neonate was doing well post-operatively; he resumed enteral feeding on post-operative day one and passed stool on the same day. He was discharged from NICU on POD 4. On follow-up at the clinic 2 weeks later, the baby was doing well, gaining weight, tolerating enteral feeding, and showing good physical activity.
Case 2
A 1-day-old male neonate (34 weeks of gestation) was delivered by caesarean section with a birth weight of 2280 g and an APGAR score of 8 and 9 at 1 and 5 min, respectively. The infant was admitted to the NICU with respiratory distress syndrome and was managed by non-invasive positive pressure ventilation (NIPPV). A chest X-ray showed severe hilar infiltrates bilaterally with a fine granular pattern. The respiratory status of the infant deteriorated on his second day of life. Thus, he required intubation and received surfactant therapy. After surfactant administration, the condition of the infant showed no improvement. A follow-up chest X-ray showed severe lung disease with evidence of free intraabdominal air (Fig. 2). The abdomen showed no skin erythema and was distended and soft on palpation; bowel sounds were audible. The patient was afebrile, had borderline blood pressure, and had normal capillary refill time. The laboratory results were all within normal ranges.
As this patient respiratory condition rapidly deteriorated a decision of urgent exploration laparotomy was decided, during exploration no gastrointestinal perforation could be found; the bowel was grossly healthy. A few hours post-surgery, the patient developed metabolic acidosis, followed by hypotension, and delayed capillary refill. He was managed with inotropes and intravenous hydrocortisone. A head ultrasound was done, which showed bilateral grade 3 intraventricular haemorrhage. The patient had a severe drop in haemoglobin level that necessitated a blood transfusion. This was later complicated by post-haemorrhagic hydrocephalus for that he required ventriculoperitoneal shunt insertion. A large ductus arteriosus was identified, which responded well to fluid restriction and a 3-day course of oral paracetamol.
Follow-up abdominal X-ray showed no free air in the abdomen. His abdominal examination was normal. Moreover, the neonate passed meconium on the second postoperative day, the inotropes were weaned gradually, and enteral feeding was started on POD 3 and was well tolerated.
Case 3
A 28-day-old boy, product of vaginal delivery term, with a birth weight of 2800 g, no NICU admission. He was born with syngnathia which is a craniofacial anomaly resulting in fusion of upper and lower jaws, he had bony fusion between maxilla and mandible on the right side and soft tissue fusion on the left side. Associated with secondary cleft palate and bilateral congenital cataract, his heart was normal as proven by echocardiogram and was gaining weight. At the age of 21 days, he underwent surgery under GA for osteotomy of his fused jaw and tracheostomy insertion (size 3.5 Fr). Postoperatively, he was doing well, with stable vital signs; he had a left femoral central venous line, nasogastric tube, oral airway, and packing of the jaw to prevent bleeding. Later, his postoperative course was complicated with fever and respiratory depression, for which he required oxygen support in the form of high-frequency oscillatory ventilation and low dose inotropes. On POD 8, the patient developed a sudden episode of cardiopulmonary arrest, he received cardiopulmonary resuscitation CPR for 3 cycles and ambu bagging through tracheostomy, surgery team was consulted during CPR to assess for tension pneumothorax, and he underwent needle thoracocentesis which was positive followed by right-sided chest tube insertion (10 Fr, closed technique, at 5th intercostal space, anterior axillary line). Chest X-ray (CXR) is shown in (Fig. 3a), viewing large right-sided pneumothorax and pneumoperitoneum. His abdominal exam showed soft abdomen on palpation with no skin erythema with mild distension. Due to the patient’s condition, a decision was taken to observe pneumoperitoneum and resuscitate the child. CXR post chest tube insertion showed almost the resolution of pneumothorax and significant improvement of pneumoperitoneum as shown in (Fig. 3b). After 2 days, Gastrografin follow-through (Fig. 3c) showed no evidence of contrast extravasation from the GI tract. The patient was kept on observation, he resumed enteral feeding via NGT, passed stool after 1 day and showed significant clinical improvement. The chest tube was removed after the resolution of pneumothorax, and the baby was followed up by the primary team with no evidence of recurrence of pneumoperitoneum. The infant later developed multiple respiratory complications and arrested multiple times; he died after 3 months of surgery due to sepsis and respiratory depression.
a CXR; showing right-sided tension pneumothorax, and pneumoperitoneum. b Follow-up CXR for Pt in a; showing resolution of pneumothorax after chest tube insertion and improvement of pneumoperitoneum. c Gastrografin follow-through; showing no evidence of contrast extravasation from the gastrointestinal tract
Discussion
The identification of pneumoperitoneum on abdominal imaging has been always considered a surgical emergency requiring prompt surgical intervention. Yet, with the recognition of spontaneous pneumoperitoneum, the management of such can be altered to a more benign course, avoiding the burden of surgery and general anaesthesia on the weak newborns.
While cases of non-surgical pneumoperitoneum have been well documented in adults, evidence within the pediatric population is lacking. It was believed that pneumoperitoneum in children almost always resulted from a perforated viscus as in the case of necrotizing enterocolitis [6].
There are numerous documented causes of non-surgical pneumoperitoneum, which are categorized into thoracic, abdominal, gynaecological, idiopathic, and pseudo-pneumoperitoneum, it can also be a complication of cardiopulmonary resuscitation, mechanical ventilation, gynaecologic manipulation, peritoneal dialysis, and gastrointestinal endoscopic procedures [10, 11]. Previous abdominal surgeries are also an obvious cause of pneumoperitoneum. However, 97% of cases of post-operative free air resolves within 5 days [12].
In children, the most common causes of non-surgical pneumoperitoneum are peritoneal dialysis, endoscopic gastrointestinal procedures, pneumatosis cystoides intestinalis, and mechanical ventilation [13]. In the paediatric population, pneumoperitoneum occurs in 1–3% of infants who are mechanically ventilated [11]. In our series, our reported cases have developed pneumoperitoneum following positive pressure ventilation or ambu bagging, which we believed was the most likely because of their pneumoperitoneum, given that no other source of perforation or infection was identified.
Subclinical perforations may be an expected route for the development of idiopathic pneumoperitoneum, but those perforations are thought to resolve without surgical intervention [14].
Plain chest or abdominal radiography is the most common imaging modality for the diagnosis of intraperitoneal free air in the emergency setting [15], but abdominal CT is a more sensitive method of diagnosing pneumoperitoneum and identifying the cause of acute abdomen [16]. In our series, all of the patients did not get a CT scan because there were on respiratory support and were unstable for the transfer to CT rooms. Moreover, modern technology with multidetector CT is highly accurate for predicting the site of GI tract perforation [17]. In our hospital, the upper GI contrast study was done bedside in the NIC Units with serial portable X-rays.
While imaging modalities have greatly aided in our detection of pathologies requiring emergent surgery, the clinical picture of the patient needs to remain the primary determinant of the need for operative intervention.
In clinical practice, once pneumoperitoneum is found, it is difficult to avoid emergency surgical exploration, because it is needed to rule out visceral perforation, especially when the patients show signs of sepsis and abdominal exam finding suggesting NEC which is the most common cause of perforation. However, Karaman et al. developed an algorithm for evaluation of pneumoperitoneum; it includes a thorough history taking concerning cardiopulmonary resuscitation, intubation, and ventilator use, a physical examination to investigate subcutaneous emphysema, and a number of diagnostic procedures such as paracentesis or peritoneal lavage [11]. Regarding our cases, case 1 radiological contrast study that showed evidence of leak led the clinical decision to exploration. While in case 2, the progression of the clinical condition led us to early exploration. In case 3, we applied the suggested algorithm.
In conclusion, spontaneous pneumoperitoneum should be considered in every neonate with a similar presentation, which when recognized requires no further surgical intervention but close observation and supportive care. we recommend every treating physician facing such cases evaluate each case individually, to consider conservative management every time the patient condition allows and not rush for unnecessary surgery.
Ethical approval was obtained from the institution review board for reviewing the cases’ medical records and imaging.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
Estridge P, Akoh JA. Recurrent spontaneous pneumoperitoneum: a surgical dilemma. Int J Surg Case Rep. 2017;30:103–5. https://doi.org/10.1016/j.ijscr.2016.11.053.
Abdelmohsen SM, Osman MA. Idiopathic neonatal pneumoperitoneum, a case report. Int J Surg Case Rep. 2017;31:250–3. https://doi.org/10.1016/j.ijscr.2017.01.053.
Čečka F, Sotona O, Šubrt Z. How to distinguish between surgical and non-surgical pneumoperitoneum? Signa Vitae. 2014;9(1):9–15.
Gummalla P, Mundakel G, Agaronov M, Lee H. Pneumoperitoneum without intestinal perforation in a neonate: case report and literature review. Case Rep Pediatr. 2017;2017:1–5 Available from: https://www.hindawi.com/journals/cripe/2017/6907329/.
Broekaert I, Keller T, Schulten D, Hünseler C, Kribs A, Dübbers M. Peritoneal drainage in pneumoperitoneum in extremely low birth weight infants. Eur J Pediatr. 2018;177(6):853–8.
Swanson JR. Surgical necrotizing enterocolitis defined. J Perinatol. 2014;34(10):731.
Al-lawama M, Al-Momani HM, Abokwaik WM, Al-zaben KR. Benign pneumoperitoneum in newborns: which abdomen to open and which one to observe? Clin Case Rep. 2016;4(6):561–3.
Gupta R, Sharma SB, Golash P, Yadav R, Gandhi D. Pneumoperitoneum in the newborn: is surgical intervention always indicated? J Neonatal Surg. 2014;3(3):2–4.
He TZ, Xu C, Ji Y, Sun XY, Liu M. Idiopathic neonatal pneumoperitoneum with favorable outcome: a case report and review. World J Gastroenterol. 2015;21(20):6417–21.
Mularski RA, Sippel JM, Osborne ML. Pneumoperitoneum: a review of nonsurgical causes. Crit Care Med. 2000;28(7):2638–44.
Karaman A, Demirbilek S, Akın M, Gurunluoglu K, Irsi C. Does pneumoperitoneum always require laparotomy? Report of six cases and review of the literature. Pediatr Surg Int. 2005;21:819–24.
Nielsen KT, Lund L, Larsen LP, Knudsen P. Duration of postoperative pneumoperitoneum. Eur J Surg. 1997;163(7):501–3.
Mosely HS, Grout G, Luallin D. Pneumoperitoneum and its association with ruptured abdominal viscus. Arch Surg. 1988;123(6):709–12.
Spinelli N, Nfonsam V, Marcet J, Velanovich V, Frattini JC, Spinelli N, et al. Postoperative pneumoperitoneum after colorectal surgery: expectant vs surgical management. world. J Gastrointest Surg. 2012;4(6):152–6.
Chiu Y, Chen J, Tiu C, Chou Y. Reappraisal of radiographic signs of pneumoperitoneum at emergency department. Am J Emerg Med. 2009;27(3):320–7. https://doi.org/10.1016/j.ajem.2008.03.004.
Ng CS, Watson CJE, Palmer CR, See TC, Beharry NA, Housden BA, et al. Evaluation of early abdominopelvic computed tomography in patients with acute abdominal pain of unknown cause: prospective randomised study. BMJ. 2002;325(7377):1387.
Oguro S, Funabiki T, Hosoda K, Inoue Y, Yamane T, Sato M, et al. 64-slice multidetector computed tomography evaluation of gastrointestinal tract perforation site: detectability of direct findings in upper and lower GI tract. Eur Radiol. 2010;20:1396–403.
Acknowledgements
The authors appreciate the work of Ms. Hadil Al-Qaisi in editing the manuscript English language.
Funding
None received.
Author information
Authors and Affiliations
Contributions
RA is the principal investigator that generated the study idea, revised the manuscript, and edited the discussion section. EB and ML are the physicians that followed the patients clinically and provided data for the study. MA wrote the introduction section and made a literature review. EH collected the images and double-checked the collection of cases data. BD wrote the first case. AS written the second case. MJ wrote the third case. HM wrote the discussion section and abstract section. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is approved by institutional review board IRB.
Consent for publication
Written informed consent was obtained from the patients’ parents for publication of this case series and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al-Taher, R., Mansour, H., Al-Qaisi, M. et al. Spontaneous pneumoperitoneum in neonates: a case series. Ann Pediatr Surg 18, 33 (2022). https://doi.org/10.1186/s43159-022-00170-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-022-00170-7