Abstract
Background
Pediatric pyeloplasty in ureteropelvic junction obstruction (UPJO) is indicated in renal impaired drainage or renal function deterioration. The improvement of renal function after pediatric pyeloplasty is still controversial in poorly functioning kidneys. Past studies on poorly functioning kidneys had a variable SRF specification, and these studies often had a limited number of patients so that they did not achieve statistical significance. The study aims to detect the renal functional improvement after pediatric Anderson-Hynes pyeloplasty (AHP) with split renal function (SRF) less than 20% (poor renal function).
Results
A retrospective study included 46 pediatric patients with unilateral UPJO who underwent open AHP with SRF < 20% on a renal isotope scan from August 2012 to October 2018. Success was defined based on either improvement in symptoms, improvement in drainage on postoperative renography, and/or improvement or stability in SRF on the renal scan done 6 months postoperatively and yearly thereafter. Deterioration of SRF by more than 5% was deemed to be deterioration. An increase in SRF of more than 5% was deemed to be an improvement.
A total of 46 patients with a mean age of 32 months with poor renal function on isotope renogram (SRF < 20%) were included. All patients had an obstructive pattern on the preoperative radionuclide scans. The median preoperative SRF was 9.26%. The mean (range) follow-up was 30 months. The success rate was 91.3%. Three patients underwent redo pyeloplasty, whereas a secondary nephrectomy was necessary for one. The remaining (42) patients showed stability or improvement of SRF with no further symptoms. Renal scintigraphy at 6 and 12 months after surgery revealed significantly increased SRF compared to preoperative one.
Conclusion
Poorly functioning renal unit with SRF < 20% can show functional improvement and recoverability after pediatric pyeloplasty.
Similar content being viewed by others
Background
In children with unilateral ureteropelvic junction obstruction (UPJO), a reduction in the split renal function (SRF) of less than 40% is usually considered an indication for surgery [1]. Improvement of SRF in poorly functioning kidneys after pediatric pyeloplasty is still under dispute [2, 3]. A study showed that PUJO cases with SRF < 35% had a high risk of substantial biopsy histological changes and a low likelihood of postoperative improvement in SRF [4].
The pyeloplasty vs. nephrectomy indication is focused primarily on the results of repeated renal ultrasonography (US) and renal scintigraphy [5]. Usually, nephrectomy was recommended when SRF < 10% [6, 7]. Long-term follow-up studies suggest that even with an initial SRF of less than 10%, a considerable increase in SF can be seen when pyeloplasty is done so that nephrectomy is not warranted [8,9,10].
Past studies on poorly functioning kidneys had a variable SRF specification, and these studies often had a limited number of patients so that they did not achieve statistical significance [11].
In this study, we conducted Anderson-Hynes pyeloplasty (AHP) for UPJO in children with poor renal function defined as SRF less than 20% on a renogram to detect renal function improvement and avoid unnecessary nephrectomy. Besides, to promote better management of family expectations and understanding of the course of UPJO in cases where a renal function has already been significantly reduced.
Methods
A retrospective study included 46 children with unilateral UPJO with a normal contralateral kidney, who underwent AHP in poorly functioning kidneys with SRF < 20% on renogram from August 2012 to October 2018. The research was approved by Urology and Faculty Ethics Committees (IRB No. Uro-surg./D/2017/0001), and informed consent that were given by parents of all cases were reviewed.
Bilateral UPJO and UPJO with associated congenital anomalies such as duplex kidneys, posterior urethral valve, vesicoureteric reflux, solitary kidney, and crossed renal ectopia were excluded. Records of detailed history, clinical examination, and routine investigations have been reviewed.
The diagnosis of UPJO was based on the renal US, the hydronephrosis degree according to the guidelines of the Society of Fetal Urology (SFU) (grade I–IV) [12], and obstructed drainage in renal scintigraphy using Tc-99m DTPA. Renal static and dynamic images were performed, and SRF proportions were detected. Excretory urography and magnetic resonance urography (MRU) were done in selected cases.
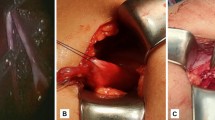
Open AHP had been done in all children. During operation, the antegrade double-J (DJ) stent was fixed in all children and then postoperatively removed after 4–6 weeks.
The primary outcome was to evaluate the functional success of AHP for UPJO in poorly functioning kidneys with SRF < 20% on renogram. Succeeded AHP was defined based on either improvement in symptoms, improvement in drainage on renal scintigraphy, and/or improvement or stability in SRF on the renal scintigraphy using Tc-99m DTPA done 6 months after the operation and annually afterward. Renal scintigraphy performed at the last follow-up was involved in the study.
Deterioration of SRF by more than 5% of the preoperative value was deemed to be deterioration. An increase in SRF of more than 5% in the ipsilateral kidney was deemed an improvement. A change in SRF of within ± 5% was deemed stable renal function [13, 14].
The secondary outcome was detecting the impact of child age at AHP, gender, the affected side, clinical presentation, parenchymal thickness, SFU Grade of hydronephrosis, and preoperative SRF on the outcome of AHP.
IBM SPSS Statistics version 23.0 (IBM Co., USA) was used to collect and analyze data. We used the chi-square or Fisher’s exact tests for categorical variables. The continuous variables were evaluated by Student’s t test or Mann-Whitney U test for, respectively, equal and unequal distributions. p < 0.05 was significant.
Results
A total of 46 children with a mean age of 32 months (3 to 154 months), and boys to girls ratio of 4:1, with poor renal function on renal scintigraphy (SRF < 20%) were included in the study. All children had an obstructive pattern (T1/2 > 20 min) on the preoperative renal scintigraphy. There were no abnormalities present in the contralateral kidney in the US. The mean preoperative SRF was 9.26% (range 3–19%). Patient preoperative features are given in Table 1.
No intra-operative complications were detected, the mean operative time was 90.3 ± 20.6 min, and there was no major intra-operative blood loss.
The mean (range) follow-up was 30 (12–84) months. The success rate of AHP was 91.3%. Three children required redo pyeloplasty, while a secondary nephrectomy was required for one. The remaining 42 children displayed improvement or stability of SRF on follow-up renal scintigraphy with no additional symptoms.
Renal scintigraphy at 6 and 12 months after surgery revealed significantly increased SRF compared to preoperative one (mean 19.7% and 21.2%, p = 0.002 and 0.009 respectively). However, there is no statistical difference between 6 months and 12 months after AHP (p = 0.29).
At 6 months, SRF improved in 24 cases (52.2%), remained stable in 18 (39.1%), and deteriorated in 4 cases (8.7%). The level of SRF improvement was in the range of 8–21%. On the other hand, postoperative diuretic renography demonstrated normal drainage in 22 children (47.8%) and prolonged drainage in 24 children (52.2%). Postoperative outcomes at 6 months are provided in Table 2.
We analyzed the impact of child age at AHP, gender, the affected side, clinical presentation, parenchymal thickness, SFU Grade of hydronephrosis, and preoperative SRF on the outcome of AHP. We observed no statistically significant relationship between these variables and the success of AHP in the study group of children (Table 3).
Discussion
UPJO is the most prominent upper urinary tract congenital anomaly; it causes flank pain, hematuria, UTI, and renal function deterioration. Open pyeloplasty is a gold standard therapy for UPJO with a recorded success rate of more than 95% [15,16,17].
Broad use of the US and the advancement of new imaging modalities also contributed to earlier UPJO diagnosis. The definition of poorly functioning kidneys shows wide variability. We considered the kidney is poorly functioning if SRF < 20%, and in the literature, other cut-offs were used, are ranging from < 30 to < 5%. This is the reason for heterogeneity in the results of different studies. We assume that there is no evidence to justify the use of a clear cut-off [5, 8,9,10,11, 18, 19].
Research has been undertaken to establish the association between SRF, histological renal changes, and results after pediatric pyeloplasty. They detected that with SRF< 35%, the kidneys have a high probability of major histological improvements and a low probability of SRF improvement [4].
UPJO management’s objectives are to release obstruction, avoid additional renal function deterioration, and relieve symptoms. The effects of pyeloplasty in children with poorly functioning kidneys are still appraised [19].
The UPJO natural history is unpredictable; although some patients undergo severe and permanent kidney damage, others demonstrate stabilization or improvement over time [20].
We researched the improvement of SRF after AHP in 46 children with preoperative SRF less than 20% on renal scintigraphy to detect renal function improvement and avoid unnecessary nephrectomy. The cases were diagnosed by using US and diuretic renal scintigraphy using DTPA.
Our study’s presentation mode is the antenatal diagnosis, abdominal swelling, accidentally discovered, UTI, or abdominal pain. There were no cases admitted with pyonephrosis or needed DJ stents or percutaneous nephrostomy (PCN). We observed no significant effect on postoperative SRF from preoperative presentation mode.
Capolicchio et al. noticed minimal recovery after pyeloplasty is in with poorly functioning kidneys and hydronephrosis diagnosed antenatally [13]. Salem et al. reported the same results in all their studied populations [21].
In several studies, the PCN tube was used preoperatively in all their patients to detect the chance of renal recovery [8, 9, 11]. While in our study, PCN not used in any case, as the policy in our center to use PCN only in case of an emergency such as pyonephrosis, single kidney, or bilateral obstruction with elevated serum creatinine, this opinion is in agreement with Lone et al. in their study [5]. Also, PCN fixation in pediatrics is done under general anesthesia, which epitomizes the child’s extra risk [22].
The success rate in the current study was 91.3%. Redo-pyeloplasty was needed in three children, while one case needed a nephrectomy. The stability or improvement of SRF was detected in forty-two cases on follow-up radiography with no additional complaints. The mean follow-up (range) was 30 (12–84) months, which is in range with most of the previous studies [5, 8, 9, 18, 19].
Renal scintigraphy at 6 and 12 months after AHP revealed significantly increased SRF compared to preoperative one (median: 14.8% and 15.7%, p = 0.002 and 0.009, respectively). However, there is no statistical difference between 6 months and 12 months after surgery (p = 0.29).
Menon et al. studied 112 patients with SRF< 20 undergoing pyeloplasty. The improvement of mean SRF was detected from 3.1 ± 2.9 to 18.4 ± 14.1% in the preoperative < 10% and from 14.8 ± 3.4 to 23.71 ± 10.48% in the 10–20% group and 10 cases needed a nephrectomy. PCN was done in 34 patients with significant improvement in mean SRF [11].
Wagner et al. reported pyeloplasty outcomes in 32 cases by dividing them into three groups (I > 40%, II 10–40%, III < 10%). They detected an increase of SRF one year after the operation in cases with < 10% SRF [18].
A retrospective analysis of pyeloplasty in 39 cases was divided into group I with SRF (10–30%) and group II with SRF < 10%. The mean SRF increased after the operation to 38.9% in group I and 19% in group II. The success rate was 90%, with a mean follow-up period of 41.6 months [19].
In other, the study of Lone et al. included 24 pyeloplasty cases with SRF ≤ 15%. The postoperative SRF improvement was to a mean of 18.08 ± 7.3% at 3 months with no significant changes at 9 months and 18 months results, so the significant SRF improvement happens early after pyeloplasty [5].
In a retrospective study done by Gnech et al., the improvement in SRF was observed in 13 (36%), stability in 16 (45%), and deterioration in 7 patients (19%). Patients with improved SRF > 5% were compared with the other cases; the only postnatal presentation was associated with better progress [23].
Chandrasekharam et al. retrospectively studied pyeloplasty’s functional outcome in children, with substantial improvement in most kidneys with compromised function, particularly with SRF less than 30%. Children with abdominal swelling at an early age demonstrated improved outcomes and substantial continued improvement for one year after surgery [22].
Nayyar et al. retrospectively analyzed 32 cases after pyeloplasty with a split function of less than 20%. The success rate was 93.7% [24]. In their study, Aziz et al., with a comparatively small number of cases, placed a nephrostomy in hydronephrotic kidneys with SRF < 10%. The renal function increased significantly after the initial PCN, eliminating any nephrectomy need in them [8]. Another study analyzed the outcomes of 23 pediatric pyeloplasties. The hydronephrotic kidneys, which had decreased GFR preoperatively enhanced postoperatively, were found. The change was more evident in the kidneys with substantially decreased preoperative GFR [25].
In this study, there was no association between improvement of SRF after AHP and other preoperative factors, such as the age of patients at AHP and severity of hydronephrosis, which is the same as Wagner et al. study [18]. The improvement of hydronephrotic kidney SRF with an antenatal diagnosis was no different than those diagnosed later, as stated by Capolicchio et al. and Cornford and Rickwood [13, 26].
Despite the latest classification, the Urinary Tract Dilation (UTD) Classification System, this study used SFU classification because it is a retrospective study, and this system has not been popularized for postsurgical kidneys [27].
There were drawbacks to our analysis. The first had a retrospective style and a comparatively limited number of cases; this caused the analysis deficient in identifying some variations. It appears to be a large series that underlines the study results’ clinical relevance due to poor renal function, with PUJO kidneys is a relatively uncommon disease. The second limitation was the usage of DTPA in renal scintigraphy as MAG3 is favored in pediatrics, kidneys with impaired function, and patients with a potential obstruction due to its more effective extraction; however, unfortunately, it is not available in our country [28].
Conclusion
A poorly functioning renal unit with SRF < 20% can show functional improvement and recoverability after pediatric pyeloplasty, so offering pyeloplasty for these children can preserve their kidneys and avoid unnecessary nephrectomy.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available because that is our university’s policy but are available from the corresponding author on reasonable request.
Abbreviations
- SRF:
-
Split renal function
- UPJO:
-
Ureteropelvic junction obstruction
- AHP:
-
Anderson-Hynes pyeloplasty
- UTI:
-
Urinary tract infection
- MAG3:
-
Mercaptoacetyltriglycine
- SFU:
-
Society of Fetal Urology
- APD:
-
Anteroposterior diameter
- PCN:
-
Percutaneous nephrostomy
- GFR:
-
Glomerular filtration rate
References
Chertin B, Pollack A, Koulikov D, Rabinowitz R, Hain D, Hadas-Halpren I, Farkas A. Conservative treatment of ureteropelvic junction obstruction in children with antenatal diagnosis of hydronephrosis: lessons learned after 16 years of follow-up. Eur Urol. 2006;49:734–8.
McAleer IM, Kaplan GW. Renal function before and after pyeloplasty: does it improve? J Urol. 1999;162:1041–4.
Ransley PG, Dhillon HK, Gordon I, Duffy PG, Dillon MJ, Barratt TM. The postnatal management of hydronephrosis diagnosed by prenatal ultrasound. J Urol. 1990;144:584–7.
Stock JA, Krous HF, Heffernan J, Packer M, Kaplan GW. Correlation of renal biopsy and radionuclide renal scan differential function in patients with unilateral ureteropelvic junction obstruction. J Urol. 1995;154:716–8.
Lone YA, Samujh R, Bhattacharya A, Kanojia RP. Outcome of poorly functioning kidneys secondary to PUJO preserved by pyeloplast. J Pediatr Surg. 2017;52:578–81.
Thorup J, Jokela R, Cortes D, Nielsen OH. The results of 15 years of consistent strategy in treating antenatally suspected pelviureteric junction obstruction. BJU Int. 2003;91:850–2.
Dhillon HK. Prenatally diagnosed hydronephrosis: The Great Ormond Street experience. Br J Urol. 1998;81:39–44.
Aziz MA, Hossain AZ, Banu T, Karim MS, Islam N, Sultana H, Alam MI, Hanif A, Khan AR. In hydronephrosis less than 10% kidney function is not an indication for nephrectomy in children. Eur J Pediatr Surg. 2002;12:304–7.
Gupta DK, Chandrasekharam VVSS, Srinivas M, Bajpai M. Percutaneous nephrostomy in children with ureteropelvic junction obstruction and poor renal function. Urology. 2001;57:547–50.
Ismail A, Elkholy A, Zaghmout O, Alkadhi A, Elnaggar O, Khairat A, Elhassanat H, Mosleh A, Hamad B, Elzomer J, Elkaabi A. Postnatal management of antenatally diagnosed ureteropelvic junction obstruction. J Pediatr Urol. 2006;2:163–8.
Menon P, Rao KL, Bhattacharya A, Mittal BR. Outcome analysis of pediatric pyeloplasty in units with less than 20% differential renal function. J Pediatr Urol. 2016;12(3):171.e1–7.
Fernbach SK, Maizels M, Conway JJ. Ultrasound grading of hydronephrosis: introduction to the system used by the society for fetal urology. Pediatr Radiol. 1993;23:478–80.
Capolicchio G, Leonard MP, Wong C, Jednak R, Brzezinski A, Salle JL. Prenatal diagnosis of hydronephrosis: impact on renal function and its recovery after pyeloplasty. J Urol. 1999;162(3 Pt 2):1029–32.
Abdrabuh AM, Salih EM, Aboelnasr M, Galal H, El-Emam A, Elzayat T. Endopyelotomy versus redo pyeoloplasty for management of failed pyeloplasty in children: a single center experience. J Pediatr Surg. 2018;53:2250–5.
Anderson JC, Hynes W. Retrocaval ureter; a case diagnosed pre-operatively and treated successfully by a plastic operation. Br J Urol. 1949;21:209–14.
O'Reilly PH, Brooman PJ, Mak S, Jones M, Pickup C, Atkinson C, Pollard AJ. The long-term results of Anderson-Hynes pyeloplasty. BJU Int. 2001;87:287–9.
Persky L, Krause JR, Boltuch RL. Initial complications and late results in dismembered pyeloplasty. J Urol. 1977;118:162–5.
Wagner M, Mayr J, Häcker F-M. Improvement of renal split function in hydronephrosis with less than 10 % function. Eur J Pediatr Surg. 2008;18:156–9.
Bansal R, Ansari MS, Srivastava A, Kapoor R. Long-term results of AHP in poorly functioning kidneys in the pediatric age group. J Pediatr Urol. 2012;8:25–8.
Pascual L, Oliva J, Vega PJ, Principal I, Valles P. Renal histology in ureteropelvic junction obstruction: are histological changes consequence of hyperfiltration. J Urol. 1998;160:976–9.
Salem YH, Majd M, Rushton G, Belman AB. Outcome analysis of pediatric pyeloplasty as a function of patient age, presentation and differential renal function. J Urol. 1995;154:1889–93.
Chandrasekharam VVSS, Srinivas M, Bal CS, Gupta AK, Agarwala S, Mitra DK, Bhatnagar V. Functional outcome after pyeloplasty for unilateral symptomatic hydronephrosis. Pediatr Surg Int. 2001;17:524–7.
Gnech M, Berrettini A, Lopes RI, Moscardid P, Esposito C, Zucchetta P, Dénes FT, Manzoni G, Braga LH, Castagnetti M. Pyeloplasty vs. nephrectomy for ureteropelvic junction obstruction in poorly functioning kidneys (differential renal function <20%): a multicenteric study. J Pediatr Urol. 2019;15:553.e1–8.
Nayyar R, Yadav S, Singh P, Kumar R, Seth A, Dogra PN. Outcomes of pyeloplasty in very poorly functioning kidneys: examining the myths. Urology. 2016;92:132–5.
Vihma Y, Korppi-Tommola T, Parkkulainen KV. Pelviureteric obstruction in children: the effect of pyeloplasty on 99mTc-DTPA uptake and washout. Z Kinderchir. 1984;39:358–63.
Cornford PA, Rickwood AMK. Functional results of pyeloplasty in patients with antenatally diagnosed pelviureteric junction obstruction. Br J Urol. 1998;81:152–5.
Nguyen HT, Benson CB, Bromley B, et al. Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol. 2014;10(6):982–98.
Gordon I, Piepsz A, Sixt R. Guidelines for standard and diuretic renogram in children. Eur J Nucl Med Mol Imaging. 2011;38(6):1175–88.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
E S: protocol development, data collection, and manuscript writing. I A: data collection and manuscript editing. M.E: data collection and analysis. G S: data analysis and manuscript writing. H G: data analysis and manuscript revision. M Z: data collection and manuscript revision. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were following the Al-Azhar Faculty of Medicine Ethical Committee’s ethical standards and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Institutional Review Board (IRB) approval was obtained. Firstly, by the urology department ethical committee then by the faculty of medicine Al-Azhar University Ethical Committee.
No. Uro-Surg./D/2017/0001.
Informed written consent was obtained from all parents or legal guardians of participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salih, E., Abdelmaksoud, I., Elfeky, M. et al. Renal functional improvement after pediatric pyeloplasty in kidneys with split renal function less than 20%: a single institute experience. Ann Pediatr Surg 17, 17 (2021). https://doi.org/10.1186/s43159-021-00084-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-021-00084-w