Abstract
Background
Intussusception is the most common intestinal obstruction among infants and young children. Most of the pediatric cases are ileo-cecal, while jejuno-jejunal and ileo-ileal combined contribute only 2.5% of the cases.
Case presentation
A 5-day-old child presented with recurrent non-bilious vomiting since birth. Physical examination revealed a slightly distended abdomen. A plain radiograph revealed a countable bubble appearance. The initial clinical diagnosis was gastric outlet obstruction. During surgery, we discovered multiple ileo-ileal intussusception associated with duodenal atresia. We manually reduced the intussusceptions and bypassed the duodenal atresia using Kimura’s procedure. We did not find any significant morbidity in the post-operative phase.
Conclusion
Multiple ileo-ileal intussusception rarely associates with duodenal atresia. In our case report, the intussusceptions might be indirectly caused by duodenal atresia through various pathophysiology. Other unusual findings also supported this suggestion.
Similar content being viewed by others
Background
Intussusception is the invagination of one part of the intestine into another. It is the most frequent cause of intestinal obstruction among infants and toddlers between 6 and 18 months of age [1,2,3]. This illness contributes to only 3% of intestinal obstruction in neonates and premature infants [3]. Most of the pediatric cases are ileo-cecal, while jejuno-jejunal and ileo-ileal combined contribute only 2.5% of the cases [2].
Duodenal atresia is a congenital anomaly and one of the most common causes of fetal bowel obstruction [4]. The incidence of this anomaly varies between 1 in 6000 and 1 in 10,000. Duodenal atresia is associated with Down syndrome in 28.2% of the case, annular pancreas in 23.1% of the case, congenital heart disease in 22.6% of the case, malrotation in 19.7% of the case, esophageal atresia-tracheoesophageal fistula in 8.5% of the case, genitourinary malformations in 8.0% of the case, anorectal malformations in 4.4% of the case, another bowel atresia in 3.5% of the case, and other anomalies in 10.9% of the case [5]. A duodenoduodenostomy that bypasses the obstruction is the best corrective option in almost all situations [5]. Here, we report a case of duodenal atresia associated with multiple ileo-ileal intussusception.
Case presentation
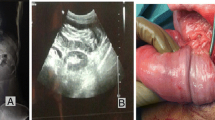
A 5-day-old male infant was presented with recurrent non-bilious vomiting since birth. The vital sign was normal. Physical examination showed a slightly distended abdomen, and rectal examination revealed yellow fecal material. Laboratory test results and biochemical profile were normal. Plain radiograph (Fig. 1) revealed a countable bubble appearance including 1 massively dilated bubble and minimum bowel gas at the lower portion of the abdomen. The patient was initially assessed with gastric outlet obstruction.
During surgery, a type 1 duodenal atresia and a total of 4 intussusception sites (Fig. 2) were found. The invaginated segments were 15 cm (Fig. 2a), 20 cm (Fig. 2b), 30 cm (Fig. 2c), and 40 cm (Fig. 2d) proximal to the ileocecal junction. None of the invaginated segments was gangrenous. All the intussusception segments had collapsed bowel both proximal and distal to each of them. All intussusception sites were reduced manually. We did not find any associating pathological lead point. We performed Kimura’s procedure to bypass the duodenal atresia (Fig. 3). The overall performed procedures is illustrated below (Fig. 4). The patient had a stable condition in the postoperative phase and was able to tolerate breast milk diet orally at the 2nd day following the surgery. Anal dilation using the examiner’s finger was required to initiate defecation; once the patient was able to defecate spontaneously, anal dilation was no longer performed.
Discussion
Intussusception is the leading cause of intestinal obstruction in childhood. Presenting symptoms vary between patients. The classic triad of vomiting, abdominal pain, and bloody stools was only found in one fourth of the total patients [6]. The correct diagnosis of intussusception can only be made clinically about 50% of the time. The diagnostic evaluation relies on radiologic imaging to either confirm or make the correct diagnosis [1].
Our 5-day-old patient is out of the prevalent age for intussusception, which is 6 to 18 months. We suggest that multiple intussusception might have a wider range of prevalent age.
Well-known possible comorbidities associating duodenal atresia are Down syndrome, annular pancreas, congenital heart disease, malrotation, esophageal atresia-tracheoesophageal fistula, genitourinary malformations, anorectal malformations, and another bowel atresia [5, 7]. A case of retrograde intussusception secondary to duodenojejunostomy in duodenal atresia has been reported [7], while duodenal atresia associated with multiple ileo-ileal intussusception has not yet been reported. To our knowledge, multiple small bowel intussusception in childhood was reported with only the following conditions: celiac disease, Peutz-Jeghers syndrome, segmentary lipomatosis, and Rapunzel syndrome [2].
Factors listed below has been proposed as the underlying pathophysiology of intussusception [8]:
-
1.
Mature lymphoid tissue that might develop into lead points of intussusception, particularly when the patient has a viral/bacterial infection that may cause a lymphoid hyperplasia
-
2.
The thin wall of the small intestine which makes it easily invaginate
-
3.
Narrow ileal lumen which is easily obstructed and develop into a lead point of intussusception
-
4.
Underdeveloped fixation of the ileocecal region
Other possibilities of lead points are polyps, lipomas, Meckel diverticulum, intestinal duplication, Henoch-Schonlein purpura, lymphomas, foreign bodies, parasitic infestations, celiac disease, and cystic fibrosis [9, 10].
According to the factors mentioned above, we suggested that the duodenal atresia in our patient might be the cause of multiple ileo-ileal intussusception indirectly by obstructing the food passage. The obstruction gave an absence in ileal lumen thus, narrowing it. The thin wall of the small intestine and underdeveloped fixation of the ileocecal region made this process became more likely to occur. Collapsed ileum both proximal and distal to the intussusception sites supported our suggestion. The absence of a possible lead point emphasized that multiple intussusception does not require all of the factors above to develop.
Availability of data and materials
The data is kept confidential and is in place within the records of the Division of Surgery Department, RSD Dr. Soebandi, Jember, Indonesia.
References
Columbani PM, Scholz S. Intussusception. In: Coran AG, Adzick NS, Krummel TM, editors. Pediatric surgery. 7th ed. Philadelphia: Elsevier Saunders; 2012. p. 1093–110.
Kızılyıldız BS, Beger B, Sönmez B, Karaman K. Multiple ileo-ileal intussusception in a 3-year-old child. Eur J Gen Med; doi: 0.15197/ejgm.1454.
Bothara V, Rawat J, Pandey A. Neonatal intussusception: a review. J Neonatal Surg. 2018. https://doi.org/10.21699/jns.v7i1.662.
Sigmon DF, Eovaldi BJ, Cohen HL. Duodenal atresia and stenosis. [Updated 2020 Feb 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470548/.
Applebaum H, Sydorak R. Duodenal atresia and stenosis – annular pancreas. In: Coran AG, Adzick NS, Krummel TM, editors. Pediatric surgery. 7th ed. Philadelphia: Elsevier Saunders; 2012. p. 1051–8.
Pandey A, Rawat JD, Wakhlu A, Kureel SN, Gopal SC. Simultaneous occurrence of jejuno-jejunal and ileo-ileal intussusception in a child: a rare occurrence. BMJ Case Rep. 2011, 2011;11. https://doi.org/10.1136/bcr.08.2010.3294.
Humbyrd CJ, Baril DT, Dolgin SE. Postoperative retrograde intussusception in an infant: a rare occurence. J Pediatr Surg. 2006;41:E13–5.
Doi O, Aoyama K, Hutson JM. Twenty-one cases of small bowel intussusception: the pathophysiology of idiopathic intussusception and the concept of benign small bowel intussusception. Pediatr Surg Int. 2004;20:140–3.
Young TH, Ho P, Lee HS, et al. A rare case of multiple intussusceptions: intense segmentary lipomatosis of the ileum. Am J Gastroenterol. 1996;91(1):162–3.
Kibria R, Michail S, Ali SA. Rapunzel syndrome-a rare cause of multiple jejunal intussusception. South Med J. 2009;102(4):416–8.
Acknowledgements
Not applicable
Funding
The article received no funding.
Author information
Authors and Affiliations
Contributions
SS contributed to performing the surgery, general supervision of the case, and interpreting the radiographs and laboratory results. GVAEC contributed to performing the early physical examination and post-operative care. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Researchers have received consent from the patient’s guardian.
Consent for publication
The patient’s guardian gave consent through phone. The authors at the present time could not reach the patient’s guardian to obtain written consent. The authors will reach the patient’s guardian as soon as possible.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Candy, G.V.A.E., Supangat, S. Multiple ileo-ileal intussusception associated with duodenal atresia in a 5-day-old infant: case report. Ann Pediatr Surg 16, 41 (2020). https://doi.org/10.1186/s43159-020-00049-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-020-00049-5