Abstract
Background
Association between Helicobacter pylori (H. pylori) and chronic hepatitis C (CHC) still remains controversial. This work is concerned with assessing the potential role of H. pylori in the progression of hepatitis C virus (HCV)-related chronic liver disease.
Results
A total of 449 individuals constituted this study (200 individuals were used to validate the assay while 249 individuals were used to assess the correlation between H. pylori infection and CHC). H. pylori antigen was quantified in serum samples using ELISA. As a consequence, our findings showed that H. pylori positivity was increased significantly (P = 0.021) with liver fibrosis progression as it was found in 44.45% of fibrotic patients and 71.88% of cirrhotic patients. We demonstrated that patients with F4 were accompanied by a significant (P < 0.05) increase in the concentration of H. pylori antigen displaying 16.52-fold and 1.34-fold increase in its level over F0 and F1-F3, respectively. Patients co-infected with H. pylori and HCV are 3.19 times (219%) more likely to experience cirrhosis than those who are mono-infected with HCV. This suggests that the risk for developing F4 was found to increase upon H. pylori co-infection when compared to CHC mono-infected patients.
Conclusion
The elevated levels of H. pylori-antigen in HCV/H. pylori co-infection suggest increased susceptibility of co-infected patients for promoting hepatic fibrosis progression.
Similar content being viewed by others
Background
The discovery of Helicobacter pylori (H. pylori) has without doubt been one of the most remarkable achievements in medical research in the past three decades. H. pylori infects 50% of the world population. Its prevalence varies widely in different parts of the world with higher rates in developing countries. In most instances, it is acquired during childhood, and is often associated with low socio-economic class [1, 2]. It produces chronic gastritis by provoking local inflammatory response in the epithelium through release of a range of cytokine [3]. The World Health Organization classifies the bacterium as a class I carcinogen and a close association between infection and 70% of gastric cancer cases worldwide has been reported [1, 2]. Additionally, liver is likely a probable organ to be affected by H. pylori activity [4,5,6]. In this case, clinicians would need a rapid and reproducible, noninvasive assay for the screening of patients for the presence of this pathogen and if a patient indeed tested positive for H. pylori for monitoring the success of eradication therapy [7]. Unfortunately, H. pylori is fastidious and difficult to cultivate [8]. Therefore, detecting serum H. pylori antigen offers an alternative noninvasive diagnostic test. In this respect, we previously developed a sensitive and specific noninvasive immunoassay based on the detection of H. pylori circulating antigen in sera from H. pylori-infected individuals with high degree of accuracy [9]. On the other hand, increasing evidence suggests that H. pylori may be a risk factor for developing cirrhosis in patients with chronic hepatitis C (CHC) [10, 11].
Herein, we are concerned with achieving two objectives. The first one is concerned with identification and quantitation of H. pylori antigen in CHC patients and validate whether the predictive criteria identified in the previous study were able to reproduce their predictive ability in a subsequent different, but related, group of patients. The second one is dedicated to assessing the potential role of H. pylori infection in the progression of hepatitis C virus (HCV)-related chronic liver disease.
Methods
Samples
A total of 449 consecutive Egyptian individuals composed of three different groups constituted the present study. Informed consents were obtained from all participants and they were fully informed concerning the diagnostic procedures involved and disease nature. The study protocol was approved by the Ethics Committee of the Mansoura University hospitals, Mansoura University, Egypt. The consent to participate was obtained verbally and approved by Ethics Committee. The first group included serum samples of 100 H. pylori-infected individuals collected from the Gastro-Enterology and Surgery Center, Mansoura University, Mansoura, Egypt. They were diagnosed based on culture as a gold standard.
The second group included serum samples of another 249 chronic hepatitis C patients [95 with F0, 90 with F1‑F3, and 64 with F4] collected from the Tropical Medicine Department, Mansoura University hospitals, Mansoura, Egypt. These patients were tested positive for the presence of HCV-ribonucleic acid (RNA) using quantitative polymerase chain reaction assay (COBAS Ampliprep/COBAS TaqMan, Roche Diagnostics, Pleasanton, USA). Histopathological classification for liver fibrosis and cirrhosis was performed according to the METAVIR score [12]. Liver fibrosis was defined as a METAVIR score of ≤ 3 (F1‑F3) whereas cirrhosis was defined as a METAVIR score of 4 (F4). The third group included serum samples of another 100 healthy volunteers used as a control group. Overall, the first and the third groups were used to validate the assay while the second group was dedicated to assessing the correlation between H. pylori infection and chronic hepatitis C.
Laboratory tests
All serum samples constituted this study were subjected to laboratory investigations including liver function tests [alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin, albumin, and alkaline phosphatase (ALP)] measured on an automated biochemistry analyzer (A15, Biosystem, Spain). Alpha fetoprotein (AFP) level was performed by chemiluminescence, with Immulite AFP (1000) kit (Diagnostic Products Corporation; Los Angeles, CA, USA).
Detection of 58-kDa H. pylori antigen using ELISA
First of all, the target 58-kDa H. pylori antigen was previously identified at 58-kDa molecular weight based on sodium dodecyl sulfate-polyacrylamide gel electrophoresis followed by Western blot as published by Attallah et al. [9]. In this work, the quantification of 58-kDa H. pylori antigen was performed based on ELISA technique using its mono-specific antibodies (ABC Diagnostics, New Damietta, Egypt) as according to Attallah et al. [9]. Color intensity was proportional to the amount of bound conjugate and therefore is a function of the concentration of H. pylori antigen present in the serum sample.
Statistical analysis
All statistical calculations were done by the SPSS software v.15.0 (SPSS Inc., Chicago, IL) and GraphPad Prism package v.5.0 (GraphPad Software, San Diego, CA). Continuous variables were expressed as mean ± standard error of mean. One-way analysis of variance (ANOVA) and Tukey’s post hoc test were used to compare continuous variables while chi-square test was used to compare proportions. All tests were two-tailed and statistical significance assessed at the 0.05 level. Area under the curve (AUC) was used to assess the diagnostic value of 58-kDa H. pylori antigen to distinguish between patients infected with H. pylori and non-infected individuals. An AUC equal to 1.0 is characteristic of an ideal test, whereas 0.5 indicates a test without diagnostic value. The nearer a curve shifts to the top left-hand corner of the graph, the more useful the marker is for the diagnosis. Results obtained by the H. pylori culture test as a gold standard; common indicators of 58-kDa H. pylori antigen accuracy (sensitivity, specificity, efficiency, and odds ratio) were derived from such a 2 × 2 contingency table. Odds ratio (with 95% confidence intervals) was calculated to estimate the risk of a target disorder from subjects without it.
Results
As formerly mentioned, the first objective of this work is to validate whether the predictive criteria identified in the previous study [9] were able to reproduce their predictive ability in a subsequent different, but related, group of patients based on ELISA analysis. In order to estimate the diagnostic accuracy of 58-kDa H. pylori antigen, ROC curve was used as depicted in Fig. 1. As a result, the 58-kDa H. pylori antigen enabled the correct identification of H. pylori patients showing an AUC of 0.946 with 90% sensitivity, 90% specificity, and 90% efficiency.
The levels of H. pylori antigen were then quantified in patients’ sera and the results are depicted in Fig. 2a. As a consequence, our findings demonstrated that patients who had hepatic cirrhosis were accompanied by a significant (P < 0.05) increase in the concentration of H. pylori antigen when compared to those with F0 and F1‑F3. Interestingly, patients with F1‑F3 displayed 12.3-fold increase in H. pylori antigen level over patients with F0 (Fig. 2b). On the other hand, cirrhotic patients displayed a 16.52-fold and 1.34-fold increase in H. pylori antigen level over F0 and F1‑F3, respectively, as shown in Fig. 2c, d.
Quantification of H. pylori antigen in addition to its observed fold changes in serum of chronic hepatitis C patients (a). The levels of 58-kDa H. pylori antigen among different METAVIR fibrosis stages (b, c, d). The distribution of observed fold changes for 58-kDa H. pylori antigen among different METAVIR fibrosis stages (e). Prevalence of 58-kDa H. pylori antigen among patients with liver fibrosis and cirrhosis showing an increase in its detection rate with the progression of liver pathology (f). Scatter plot showing the distribution of 58-kDa H. pylori antigen with the progression of liver fibrosis. P > 0.05 is considered non-significant, P < 0.05 is considered significant, and P < 0.0001 is considered extremely significant
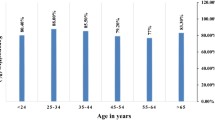
Laboratory characteristics of CHC patients with and without H. pylori infection are summarized in Table 1. Overall, there were 95/249 (38.15%) with no fibrosis (F0), 90/249 (36.15%) with liver fibrosis (F1‑F3), and 64/249 (25.70%) with liver cirrhosis (F4) as seen in Table 2. Next, the characteristics of patients with no fibrosis (F0), liver fibrosis (F1‑F3), and liver cirrhosis (F4) are summarized in Table 2. In this work, our patients were predominantly male (79.19%), with a mean (± SD) age of 39.63 (± 11.61) years at the time of liver biopsy. Patients with no fibrosis (F0) were young as compared to those who developed liver fibrosis (F1‑F3) or liver cirrhosis (F4) with an extremely significant difference (P < 0.0001) based on the analysis of one-way ANOVA followed by Tukey’s post hoc test as presented in Table 2. As anticipated, patients who developed liver cirrhosis (F4) were associated with higher levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), and alpha fetoprotein (AFP) than those who have liver fibrosis (F1‑F3) or those with no fibrosis (F0) with a significant difference (P < 0.05). On the other hand, the mean value of albumin and platelet count decreased with the progression of liver fibrosis being lower in patients who developed liver cirrhosis (F4) than those with no liver fibrosis (F0) and liver fibrosis (F1‑F3).
Furthermore, the prevalence of 58-kDa H. pylori antigen in this category of patients was found to increase with the progression of liver disease as it was 44.45% in liver fibrosis and 71.88% in liver cirrhosis as shown in Fig. 2e. Our findings showed that H. pylori antigen significantly correlated with liver fibrosis stages producing a Spearman’s rank correlation coefficient (r) of 0.501 (P < 0.0001) as depicted in Fig. 2f.
Levels of different biochemical markers were determined in CHC patients with and without H. pylori as shown in Table 3. The results demonstrated that each METAVIR fibrosis group was accompanied by an increase in their levels in case of co-infection compared to patients at the same stage in mono-infection. On the other hand, each fibrosis group was associated with a drop in the levels of both albumin and platelet count in case of co-infection compared to HCV mono-infection but the difference was statistically not significant.
Next, odds ratio was used as a measure of association between 58-kDa H. pylori antigen and different groups of diseases and the results are shown in Table 4. The risk for developing liver fibrosis and cirrhosis was found to increase upon H. pylori co-infection when compared to CHC mono-infected patients. Our findings showed that patients co-infected with H. pylori and HCV are 3.19 times (219%) more likely to experience cirrhosis than those who mono-infected with HCV. This may give a clue that H. pylori infection may have a potential role in liver-disease progression.
Discussion
There is some evidence to suggest that H. pylori infection may be associated with an increased risk of gastric and extra-gastric malignancies [2, 13,14,15,16]. Many of these studies were depending on detection of H. pylori antibodies in serum by ELISA [4, 17], histopathology methods [18], or on detection of bacterial deoxyribonucleic acid (DNA) in tumor tissues using polymerase chain reaction technique (PCR) [5]. Clearly, the use of antibodies-based methods can lead to ambiguous results especially since antibodies can be detectable a long time after the bacteria have ceased to colonize the gut [19]. The present work preferred to use H. pylori antigen-based method in order to examine the association between H. pylori infection and different liver diseases. In general, more efforts were performed for identifying various H. pylori antigens-based western blot technique, e.g., 125 kDa CagA antigen and 87 kDa VacA antigen [20]. The 58-kDa H. pylori antigen was identified in serum of patients with different gastric and duodenal diseases. The molecular mass of the serum antigen is similar to the 58-kDa fragment of the 87-kDa cytotoxin domain of the VacA protein, the subunit cellular antigen of the native H. pylori catalase, and the H. pylori catalase gene product [9]. In this work, H. pylori antigen enabled the correct identification of H. pylori patients showing an AUC of 0.946 with 90% sensitivity and 90% specificity. These results are almost matching with those of Attallah et al. [9] and Kabir [21] who showed comparable sensitivity (91‑98%) and specificities (83‑100%). So, using a 58-kDa H. pylori antigen-based method was accurate enough for studying the H. pylori association with different gastrointestinal cancers. On the other hand, we also aimed to investigate the 58-kDa H. pylori antigen in sera of patients with different liver pathology to assess the potential cofactor role of H. pylori infection in the progression of HCV-related chronic liver disease. In this work, 58-kDa H. pylori antigen was positive in 71.88% of liver cirrhosis patients compared with 44.45% in liver fibrosis patients. Other studies have evidenced of high seroprevalence of H. pylori antibodies among cirrhotic patients [4, 13]. Our results are very close to that of Dore et al. [13] who detected anti-H. pylori IgG in serum of 39% chronic hepatitis and 58% liver cirrhosis patients. In addition, Rocha et al. [5] found that Helicobacter DNA was high 68% in liver tissue of patients with liver cirrhosis. It was suggested that these bacteria could be implicated in the progression of liver disease to cirrhosis and hepatocellular carcinoma (HCC). In addition and consistent to our findings, Wang et al. found a strong association between H. pylori and chronic hepatitis C, particularly during the HCV progression stage [22]. Surprisingly, Wang et al. showed that the odds ratio for cirrhosis was 4.4 which was almost similar to that obtained in our work. Huang et al. [23] postulated that it is possible for H. pylori to invade the liver and gall bladder via the bile duct. Many theories have been proposed to explain the mechanism of H. pylori involvement in the pathogenesis and progression of cirrhosis, particularly in HCV-infected individuals [24]. Enteric Helicobacter species have been found to produce toxins that might cause hepatocellular damage in vivo. Many studies have tried to explain the mechanisms by increased levels of proinflammatory cytokines such as interleukins 1, 6 (IL-1, IL-6), tumor necrosis factor, and by the presence of lymphocytic mononuclear infiltrate and lymphoid follicle formation [23]. According to Abdel-Hady et al. [25], H. pylori infection might have a role in increasing the circulating levels of ammonia and endotoxins in cirrhotic patients, thus facilitating the onset of hepatic encephalopathy and of hepatic inflammation by stimulating the secretion of proinflammatory cytokines. As H. pylori infection increased hepatic AFP expression level and carbon tetrachloride (CCL4) intoxication increased transforming growth factor-beta1 (TGF-b1) levels, both in serum and tissues, H. pylori chronic infection might contribute to HCC progression from CCL4-induced fibrosis or cirrhosis [26, 27].
Conclusion
In summary, this work showed that the elevated levels of H. pylori-antigen in HCV/H. pylori co-infection suggest increased susceptibility of co-infected patients for promoting hepatic fibrosis progression. This suggests the importance of H. pylori screening of patients with CHC, particularly those with HCV-related cirrhosis, in order to choose the proper treatment.
Availability of data and materials
Not applicable.
Abbreviations
- AFP:
-
Alpha fetoprotein
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- CCL4 :
-
Carbon tetrachloride
- CHC:
-
Chronic hepatitis C
- DNA:
-
Deoxyribonucleic acid
- H. pylori :
-
Helicobacter pylori
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- IL:
-
Interleukins
- PCR:
-
Polymerase chain reaction technique
- RNA:
-
Ribonucleic acid
- TGF-b1:
-
Transforming growth factor-beta1
References
Peek RM, Blaser MJ (2002) Helicobacter pylori and gastrointestinal tract adenocarcinomas. Nat Rev Cancer 2(1):28–37
Kim SS, Ruiz VE, Carroll JD et al (2011) Helicobacter pylori in the pathogenesis of gastric cancer and gastric lymphoma. Cancer Lett 305(2):228–238
Mamun Al M (2010) State of the globe: helicobacter pylori and hepatitis C together hamper health. J Global Infect Dis 2(1):1–3
Esmat G, El-Bendary M, Zakarya S et al (2012) Role of Helicobacter pylori in patients with HCV-related chronic hepatitis and cirrhosis with or without hepatocellular carcinoma: possible association with disease progression. J Viral Hepat 19(7):473–479
Rocha M, Avenaud P, Menard A et al (2005) Association of Helicobacter species with hepatitis C cirrhosis with or without hepatocellular carcinoma. Gut. 54(3):396–401
Trikudanathan G, Philip A, Dasanu CA et al (2011) Association between Helicobacter pylori infection and pancreatic cancer. A cumulative meta-analysis. J Pancreas 12(1):26–31
Krüttgen A, Horz H-P, Weber-Heynemann J et al (2012) Study on the association of Helicobacter species with viral hepatitis-induced hepatocellular carcinoma. Gut Microbes 3(3):228–233
Eslick GD (2000) Helicobacter pylori infection transmitted sexually via oral-genital contact: a hypothetical model. Sex Transm Infect 76(6):489–492
Attallah AM, Ismail H, Ibrahim GG et al (2004) Use of a novel enzyme immunoassay based on detection of circulating antigen in serum for diagnosis of Helicobacter pylori infection. Clin Diagn Lab Immunol 11(4):775–779
Mao H, Li R (2014) Changes in serum pepsinogen in patients with liver cirrhosis and portal hypertensive gastropathy. Nan Fang Yi Ke Da Xue Xue Bao 34(1):141–143
Queiroz DMM, Rocha AMC, Rocha GA et al (2006) Association between Helicobacter pylori infection and cirrhosis in patients with chronic hepatitis C virus. Dig Dis Sci 51(2):370–373
Goodman ZD (2007) Grading and staging systems for inflammation and fibrosis in chronic liver diseases. J Hepatol 47(4):598–607
Dore MP, Realdi G, Mura D et al (2002) Helicobacter infection in patients with HCV-related chronic hepatitis, cirrhosis, and hepatocellular carcinoma. Dig Dis Sci 47(7):1638–1643
Buso AG, Rocha HLOG, Diogo DM et al (2009) Seroprevalence of Helicobacter pylori in patients with colon adenomas in a Brazilian university hospital. Arq Gastroenterol 46(2):97–9101
Stolzenberg-Solomon RZ, Blaser MJ, Limburg PJ et al (2001) Helicobacter pylori seropositivity as a risk factor for pancreatic cancer. J Natl Cancer Inst 93(12):937–941
de Martel C, Llosa AE, Friedman GD et al (2008) Helicobacter pylori infection and development of pancreatic cancer. Cancer Epidemiol Biomark Prev 17(5):1188–1194
Strofilas A, Lagoudianakis EE, Seretis C et al (2012) Association of Helicobacter pylori infection and colon cancer. J Clin Med Res 4(3):172–176
Soylu A, Ozkara S, Alis H et al (2008) Immunohistochemical testing for Helicobacter pylori existence in neoplasms of the colon. BMC Gastroenterol 8:35–40
Jones M, Helliwell P, Pritchard C et al (2007) Helicobacter pylori in colorectal neoplasms: is there an aetiological relationship? World J Surg Oncol 5:51–57
Abdel-Raouf M, Attallah A, Omran M et al (2014) The detection of a Helicobacter pylori antigen in some different types of gastrointestinal cancers patients. J Am Sci 10(7s):19–24
Kabir S (2001) Detection of Helicobacter pylori in faeces by culture, PCR and enzyme immunoassay. J Med Microbiol 50(12):1021–1029
Wang J, Li W-T, Zheng Y-X et al (2016) The association between Helicobacter pylori infection and chronic hepatitis C: a meta-analysis and trial sequential analysis. Gastroenterol Res Pract 2016:8780695
Huang Y, Tian XF, Fan XG et al (2009) The pathological effect of Helicobacter pylori infection on liver tissues in mice. Clin Microbiol Infect 15(9):843–849
Ceelen L, Decostere A, Verschraegen G et al (2005) Prevalence of Helicobacter pullorum among patients with gastrointestinal disease and clinically healthy persons. J Clin Microbiol 43(6):2984–2986
Abdel-Hady H, Zaki A, Badra G et al (2007) Helicobacter pylori infection in hepatic encephalopathy: relationship to plasma endotoxins and blood ammonia. Hepatol Res 37(12):1026–1033
Ki MR, Goo MJ, Park JK et al (2010) Helicobacter pylori accelerates hepatic fibrosis by sensitizing transforming growth factor-beta1-induced inflammatory signaling. Lab Investig 90(10):1507–1516
Berasain C, Perugorria MJ, Latasa MU et al (2009) The epidermal growth factor receptor: a link between inflammation and liver cancer. Exp Biol Med 234(7):713–725
Acknowledgements
The authors would like to thank staff of Biotechnology Research Center, New Damietta, Egypt, for kind help during the study. This study has been completely carried out at Biotechnology Research Center, New Damietta, Egypt.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AM and MF designed the study. AM and MS carried out literature search, designing, and editing of the manuscript. MS wrote and drew all the figures of the manuscript. SE, MM, and AA carried out the experimental work. All authors contributed to the final manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of the Mansoura University hospitals, Mansoura University, Egypt. The consent to participate was verbally and approved by Ethics Committee.
Consent for publication
The consent to publish had been taken verbally from each participant in this work.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Attallah, A.M., Albannan, M.S., Ghaly, M.F. et al. Prevalence of Helicobacter pylori infection in patients with chronic hepatitis C. J Genet Eng Biotechnol 20, 13 (2022). https://doi.org/10.1186/s43141-021-00293-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43141-021-00293-1