Abstract
Background
Combretum paniculatum (Combretaceae) Vent. is commonly used in traditional medicine to treat ulcers and gastrointestinal disorders, including distended spleens and the liver. This study investigated the gastroprotective effects of C. paniculatum leaf extract and its fractions on absolute ethanol-induced gastric ulcers in rats and explored their effects on endogenous antioxidant (SOD, MDA, GSH, and Catalase) levels. Butanol, n-hexane, and ethyl acetate extracts (100 and 200 mg/kg), omeprazole (20 mg/kg), and control (3% Tween 80) were administered orally.
Results
The methanolic extract and fractions of C. paniculatum exhibited varying degrees of ulcer protection. MECP exhibited significant (P < 0.05) ulcer protection (55.56%) at 200 mg/kg; at 100 and 200 mg/kg, HFCP induced considerable (P < 0.01 & 0.001) ulcer reduction (64.44% and 80.00%), respectively; EAFCP offered substantial (P < 0.05) ulcer reduction (57.78%) at 200 mg/kg, whereas BFCP produced significant (P < 0.01) ulcer protection (73.33% and 68.89%) at 100 and 200 mg/kg against absolute ethanol-induced ulcer. MDA levels were substantially reduced after pretreatment with the extract and fractions, whereas SOD, GSH, and catalase levels were significantly enhanced.
Conclusion
These findings suggest that C. paniculatum leaf extract and fractions possess gastroprotective actions against ethanol-induced ulcers and exert these effects through antioxidant mechanisms. Therefore, the traditional use of C. paniculatum leaves in the treatment of ulcers is justified.
Similar content being viewed by others
Background
Peptic ulcer disease (PUD) is caused by a lack of association between stomach defensive factors and offensive physical, chemical, or psychological factors that affect the epithelium of the mucosa [1]. Physical stress, heavy cigarette use, caffeine, some medicines, notably nonsteroidal anti-inflammatory drugs, and Helicobacter pylori infection are among the offensive factors [2]. Furthermore, ethanol intake has been linked to the development of stomach ulcers [3]. So, to screen the anti-ulcer drugs, the experimental model of ethanol-induced stomach ulcer is frequently used [4]. Alcohol-induced mucosal injury begins with oxidative stress and antioxidant diminution [4]. Peptic ulcer disease (PUD) is one of the most prevalent gastrointestinal ailments worldwide, with high mortality and morbidity rates [5]. Gastric ulcers occur at a rate of 0.1–0.3% each year, and the overall prevalence of this condition is 10% in the general population [6]. Ulcers can be treated with a variety of drugs including antibiotics, antacids, proton-pump inhibitors (omeprazole), and H2-receptor blockers. In PUD, the mucosal damage brought on by the gastric acid and pepsin hyper-secretions substantially outweighs the defensive systems of the gastrointestinal mucosa, including the bicarbonate and mucus secretions. The obvious symptom of the illness is a burning, night-waking epigastric discomfort that is typically eased by eating or taking antacids [3]. Bloating, stomach pain, a decrease in appetite, weight loss, nausea, and vomiting are some other signs of gastric ulcer. PUD problems may cause gastroduodenal perforation, bleeding, and blockage if ignored or improperly treated [7].
Unfortunately, owing to their significant side effects, such as gynecomastia, hypoacidity, impotence, osteoporotic bone fracture, hypergastrinemia, and cardiovascular disease risks, these medications are facing serious challenges [7,8,9]. Therefore, natural products with a broad range of biological actions, improved efficacy, and safety are required to replace chemical drugs [10, 11].
Combretum paniculatum Vent. (Combretaceae) is a tropical African shrub with a deep root structure and widely dispersed red blossoms. The plant has been demonstrated to be effective in treating chronic diarrhea, ulcers, flatulence, and enlarged spleen and liver in traditional medicine [12]. It has been documented to have potent cytotoxic effects on breast cancer cells [13], possess antimicrobial activity [14], and is effective in the treatment of ringworm infection and wound healing [15]. Recently, the gastrointestinal effect of pretreatment with Combretum paniculatum methanol leaf extract was demonstrated using experimental antidiarrheal and anti-ulcer models [16]. The current study was undertaken to examine the gastroprotective effects of Combretum paniculatum leaf extract and fractions in a rat model of absolute ethanol-induced ulcer, as well as the probable mechanisms underlying these benefits. The ethnomedical use of Combretum paniculatum for the treatment of colic, diarrhea, vomiting, and leprosy is widespread [13]. Phytochemical compounds such as cholest-5-en-3-ol, 2-phyten-1-ol, quercitrin-3-glucopyranoside, p-coumaric acid, 2, 3, 8-tri-O-methylellagic acid, beta-sitosterol, gallocatechin, apigenin, and apigenin-7-glucoside have been identified from the leaves of C. paniculatum [14]. In addition, two diglucosylated derivatives from cyanidin and pelargonidin (cyanidin 3, 5-O-β-D-diglucopyranoside and pelargonidin 3, 5-O-β-D-diglucopyranoside) have been identified from the flowers [15].
Methods
Solvent, reagents, and chemicals
The solvents, chemicals, and reagents used were of analytical grade. Sigma-Aldrich (St Louis, MO, USA) provided the Bovine serum albumin, epinephrine, 20% tricloroacetic acid, 1% thiobarbituric acid and Dithionitrobenzene. Hematoxylin and eosin were obtained from ScyTek Laboratories Inc. (West Logan, UT, USA). Analytical grade methanol, ethanol, n-hexane, ethylacetate, and butanol were obtained from BDH Chemical Ltd (Poole, England).
Drug
Omeprazole BP 20 mg (OMEFAST-20) Greenlife Pharmaceutical Limited, Lagos, Nigeria.
Experimental animals
Male Wistar rats weighing 120–180 g were obtained from the animal house of the Department of Veterinary Medicine (University of Nigeria Nsukka, Nigeria). They were raised under ideal conditions of temperature (25 °C), humidity (50–60%), and a 12-h light–dark cycle. They were allowed unrestricted access to standard feed and water. They were allowed 14 days to familiarize with the lab conditions prior to the commencement of the experiment. The Faculty of Pharmaceutical Sciences, University of Nigeria’s ethics committee (FPSRE/UNN/19/00015), gave approval of the experimental procedure in accordance with the National Code of Conduct for Animal Research Ethics (NCARE).
Plant collection and preparation
In February 2020, young leaves of C. paniculatum were collected along the bank of a stream during its flowering stage at Obukpa, Nsukka Local Government Area, Enugu State, Nigeria. It was identified, validated, and issued voucher number PCG/UNN/0321 to the plant. Fresh leaves were cleaned twice with water and placed on dry water soaking papers for drying under open, airy, and shady place for five days. The shade-dried leaves were then coarsely milled using a laboratory blender.
Plant extraction and fractionation
Cold maceration in methanol for 48 h with occasional agitation was used to extract crushed leaves (2.6 kg). A filter cloth and No. Whatman filter paper (1) was used to filter the mixture. The marc was then rinsed several times with the new solvent until the filtrate became transparent. To obtain the methanol extract of C. paniculatum (MECP), the filtrate was placed in a stainless tray and left to air-dry. The resultant dry extract was collected, weighed, and stored in an amber-colored container in a refrigerator.
MECP was further fractionated to obtain the n-hexane fraction (HFCP), ethyl acetate fraction (EAFCP), and butanol fraction (BFCP). The MECP (50 g) was weighed and crushed using a mortar and pestle, and a paste was formed using a small quantity of water. A greater quantity of water was then added until the desired consistency was achieved. The resultant solution was transferred into a separating funnel, an equal quantity of n-hexane was added to the separating funnel, and the mixture was shaken properly. The mixture was allowed to stand undisturbed using a retort stand until a clear separation was achieved. Using a beaker, the aqueous phase was separated from the n-hexane phase. This process was repeated until a clear n-hexane phase was obtained. This procedure was repeated for ethyl acetate and butanol.
Qualitative phytochemical screening of extract and fractions
Qualitative phytochemical analysis of powdered plant material samples was performed according to standard methods [17,18,19].
Quantitative phytochemical analysis of extract and fractions
Standard procedures for quantitative phytochemical analyses have been employed [18,19,20,21,22].
Acute toxicity test
The acute toxicity studies on MECP were performed using Lorke’s method, which involves two stages. The toxic range was determined in the first stage by administering 10, 100, and 1000 mg/kg MECP to three groups of mice (n = 3). Treated mice were occasionally monitored for symptoms of toxicity and death for 24 h. The dosages used in the second stage were determined based on the mortality trend of the previous stage. As no death occurred and no signs of toxicity were observed in the first phase, the second phase was initiated. A new group of four mice was orally administered 1000, 1600, 2900, and 5000 mg/kg MECP. The treated mice were monitored intermittently for 24 h to assess the symptoms of toxicity and mortality. The LD50, geometric mean of the highest non-lethal dose, and least toxic dose were obtained [23].
Absolute ethanol-induced ulcer
The absolute ethanol-induced ulcer study was performed according to previously described methods [3]. The rats were fasted for 24 h but allowed unrestricted access to water prior to the study and were allotted into five groups of six rats each. Group 1 received 3% Tween 80 (5 ml/kg) as a negative control, Group 2 received the standard drug omeprazole (20 ml/kg) with strength 5 mg/ml whereas Groups 3–5 received 100, 200, and 400 mg/kg of methanol extract. After 1 h, the animals received absolute ethanol (1 ml each) and were sacrificed 1 h later using chloroform. The number and length of gastric lesions were determined by dissecting and opening their stomachs along the greater curvature, rinsing them under running water, and pinning them on a corkboard. The ulcer score was further measured using a ruler and divider. An absolute ethanol-induced ulcer scoring method was used.
The lesions were viewed macroscopically using magnifying lens (× 10) and the size of the lesions were measured with the aid of a vernier caliper.
The scoring method of An et al., 2007, was adopted with slight modification [24].
The total score for each stomach divided by a factor of 10 was calculated for each animal and expressed as ulcer index (UI) and the average taken as mean ulcer index for each group. The degree of ulcer protection for each treated group was calculated as a percentage of the mean ulcer index of the negative control group.
A similar study was also performed with solvent fractions at three dose levels (100, 200, and 400 mg/kg).
Oxidative stress
Preparation of tissue homogenate
Following sacrifice, the stomach tissue was immediately excised, weighed, and completely homogenized in phosphate buffer (10 mM KH2PO4-K2HPO4 buffer, pH 7.4; 0.1 mM EDTA). The homogenates were centrifuged at 5000 rpm for 20 min. The supernatant was used to test for oxidative stress markers. Using bovine serum albumin (BSA) as a reference, the protein content of the supernatant was measured using the Lowry et al. technique [25].
Tissue catalase test
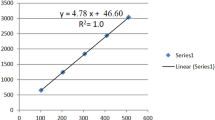
Tissue catalase activity was determined according to a method described previously [26]. When dichromate in acetic acid is heated in the presence of hydrogen peroxide (H2O2), it is reduced to chromic acetate, creating chromic acid as an unstable intermediate. The amount of hydrogen peroxide produced in the reaction was proportional to the amount of chromic acetate produced. The generated chromic acetate was quantified spectrophotometrically at 570 nm. Briefly, 0.04 ml of tissue homogenate was mixed with 2.96 ml of H2O2 (0.2 M)-phosphate buffer (0.01 M, pH 7). Dichromate/acetic acid reagent (2 ml) was added to this mixture to terminate the reaction after a 1 min interval. To eliminate precipitated proteins, the tubes were heated to 100 °C for 10 min, cooled, and centrifuged at 2500×g for 5 min. A spectrophotometer (Jenway 6305; Jenway, Essex, UK) was used to record variations in absorbance at 570 nm against a reagent blank. Tissue catalase activity (µmol H2O2/min/mg protein) was determined from a standard curve prepared similarly with 0–200 mMol H2O2.
Tissue reduced glutathione (GSH)
The presence of reduced glutathione in the tissue was evaluated using a previously described technique [27]. When dithionitrobenzene (DTNB) combines with acid-soluble sulfhydryl groups (non-protein thiols), a yellow-colored complex forms, with reduced glutathione accounting for > 93% of the total. The absorbance of the colored complex was determined at 412 nm. The tissue homogenate (0.5 ml) was combined with 0.1 ml of 25% TCA and placed on ice for a few minutes. The supernatant (0.3 ml) was then combined with 0.7 ml of 0.2 M sodium phosphate buffer (pH 8) and 2 ml of 0.6 mM DTNB after centrifugation at 3000 g for 10 min. A spectrophotometer (Jenway 6305; Jenway, Essex, UK) was used to determine the yellow color acquired after 10 min against a reagent blank at 412 nm. GSH concentrations (0–100 nMoles) were used to generate a standard graph. Using this standard graph, GSH content was computed and represented as nmol/mg protein.
Tissue malondialdehyde (MDA)
Malondialdehyde levels, a lipid peroxidation end-product, were determined using a spectrophotometric method. The reaction of thiobarbituric acid with MDA produces a persistent chromogen, which can be measured using spectrophotometry. The color intensity of the chromogen was measured at 532 nm, which is directly proportional to MDA concentration. The production of thiobarbituric acid reactive substances (TBARS) was used to measure lipid peroxidation in tissues using the Stocks and Dormandy's approach [28]. At room temperature, an equal volume of tissue homogenate was mixed with 20% trichloroacetic acid (1:1) and incubated. The samples were then centrifuged at 2500×g for 10 min. The samples were then placed in a boiling water bath (100 °C) for 15 min with 1.0 ml of 1% thiobarbituric acid added to the supernatant. The contents were cooled on ice before centrifugation at 2500×g for 15 min. A spectrophotometer (Jenway 6305; Jenway, Essex, UK) was used to measure absorbance (A) of the supernatant against a reagent blank at 532 nm. A standard graph was created using MDA concentrations ranging from 0 to 20 nM (Sigma-Aldrich). Louis, MO, USA). The degree of lipid peroxidation (TBARS) was measured in nanomoles per mg of protein.
Tissue superoxide dismutase (SOD)
The activity of superoxide dismutase (SOD) in tissues was measured as previously described [29]. SOD's capacity to prevent the autoxidation of epinephrine to adrenochrome at pH 10.2 is the basis for the test. The homogenate (0.5 ml) was diluted with an equal volume of distilled water, then 0.25 ml ice-cold ethanol and 0.15 ml ice-cold chloroform were added. This was combined well in a cyclo-mixer before being centrifuged for 10 min at 2500 rpm. 1.5 ml carbonate buffer (0.05 M, pH 10.2) and 0.5 ml 0.5 mM EDTA solution were added to the supernatant. The reaction was started by adding 0.4 ml of 3 mM epinephrine (Sigma, St. Louis, MO, USA) and measuring the change in absorbance per minute at 480 nm against a reagent blank. The enzyme unit was defined as the change in absorbance per minute when superoxide dismutase inhibited the conversion of epinephrine to adrenochrome by 50%. Using 0–195 units of SOD (Sigma, St. Louis, Mo, USA). An enzyme calibration curve was generated. SOD activity was measured in units per mg of protein.
Histopathological studies
Tissue preparation
Histopathological analysis of the stomach sections was performed. Samples were fixed in 10% phosphate-buffered formalin for 48 h. The tissues were subsequently trimmed, dehydrated in four grades of alcohol (70, 80, 90, and absolute alcohol), cleared in three grades of xylene, and embedded in molten wax.
On solidification, the blocks were sectioned, 5 µm thick with a rotary microtome, floated in a water bathe, and incubated at 60 °C for 30 min. The 5-µm-thick sectioned tissues were subsequently cleared in three grades of xylene and rehydrated in three grades of alcohol (90, 80, and 70%). The sections were then stained with hematoxylin for 15 min. Blue was performed using ammonium chloride. Differentiation was performed using 1% acid alcohol before counterstaining with eosin. Permanent mounts were made on degreased glass slides using DPX mountant.
Slide examination
The prepared slides were viewed using ×4, ×10, and ×40 objective lenses on a Motic™ compound light microscope. Photomicrographs were obtained at ×160 magnification with a Motic™ 5.0 megapixels microscope camera.
Statistical analysis
GraphPad Prism version 7.0 was used to analyze the data. One-way ANOVA was used, followed by Dunnett's multiple comparisons post hoc test. Data are presented as mean ± standard error of the mean (SEM). P < 0.05, 0.01, and 0.001 were considered statistically significant.
Results
Percentage yield of extract and fractions of C. paniculatum
The percentage yields of the C. paniculatum methanol extract and fractions are presented in Table 1.
Extract and fractions phytochemical analyses
Alkaloids, tannins, steroids, terpenoids, phenols, and flavonoids were found in HFCP, EFCP, and BFCP, but saponins and glycosides were absent (Table 2). Quantitatively, phenol had the highest concentration, followed by tannins and flavonoids, whereas saponin and steroids had the lowest concentrations (Table 3).
Effects of methanol extract of Combretum paniculatum on absolute ethanol-induced ulcer in rats
The rats developed ulcers one hour after receiving absolute ethanol. MECP demonstrated a dose-dependent level of ulcer prevention, with significance (P < 0.05) observed at 200 mg/kg (55.56%) compared to the negative control. It can also be observed that the percentage ulcer protection offered by 200 mg/kg of MECP is comparable to omeprazole (57.78%) Table 4.
Acute toxicity test (LD50)
Administration of MECP at doses of up to 5000 mg/kg did not result in mortality or significant signs and symptoms of observable toxicity in mice. This indicates that the LD50 was greater than 5000 mg/kg. As a result, MECP is regarded as safe, as proposed by Lorke [23].
Effects of C. paniculatum fractions on absolute ethanol-induced ulcer in rats
The C. paniculatum fractions showed varying degrees of ulcer protection and significance relative to the negative control. The HFCP offered the highest ulcer protection (80.00%) at 200 mg/kg; HFCP 100 mg/kg, BFCP 100, and 200 mg/kg gave significance (P < 0.01), whereas EAFCP 200 mg/kg and omeprazole caused 57.78% ulcer protection in comparison with the negative control (Table 5).
Effects of methanol extract and fractions of C. paniculatum on gastric malondialdehyde
The extract and fractions significantly reduced gastric MDA levels compared to the negative control. MECP (100 and 200 mg/kg), HFCP (100 mg/kg), EAFCP (100 mg/kg), and BFCP (100 and 200 mg/kg) significantly (P < 0.001) reduced gastric MDA levels as well as EAFCP 200 mg/kg) (P < 0.01) relative to the negative control. HFCP (200 mg/kg) lowered MDA levels; however, the difference was statistically insignificant compared to the negative control (Table 6).
Effects of methanol extract and fractions of C. paniculatum on superoxide dismutase
Compared to the negative control, oral treatment with MECP (100 and 200 mg/kg), HFCP (100 and 200 mg/kg), and EAFCP (200 mg/kg) resulted in substantial (P < 0.001 and P < 0.01) decreases in serum SOD levels. It was also discovered that EAFCP (100 mg/kg) and BFCP (100, 200 mg/kg) had no significant lowering of SOD levels Table 7.
Effects of the methanol extract and fractions of C. paniculatum on catalase levels
The extract and fractions significantly increased the catalase activity. HFCP (200 mg/kg) caused the greatest increase (621.00 ± 44.50), whereas BFCP produced the least increase (211.00 ± 15.70). The increase in catalase levels caused by the extract and fractions was also dose dependent (Table 8).
Effect of methanol extract and fractions of C. paniculatum on reduced glutathione levels
In comparison with the control, pretreatment with MECP (100 and 200 mg/kg) resulted in a substantial (P < 0.05; 0.001) dose-related increase in GSH levels. The HFCP, EAFCP, and BFCP, on the other hand, caused no substantial rise in serum GSH level. The increase in reduced glutathione caused by 200 mg/kg MECP (18.10 ± 1.43) was higher than omeprazole (15.10 ± 1.50). The increase in reduced glutathione caused by the extract and fractions was also dose dependent (Table 9).
Macroscopical findings
The stomachs of normal control rats were macroscopically examined and revealed an entirely healthy pink gastric mucosa with typical mucosal thickness (Fig. 1K). Elaborate tissue responses were observed in the negative control group, including significant dark red submucosal hemorrhagic streaks of various sizes and mucosal thickening (Fig. 1J). The hemorrhagic vascular response was reduced in the omeprazole-treated group, but the mucosa remained slightly congested and inflamed (Fig. 1I). Pretreatment with C. paniculatum extract and fractions at 100 and 200 mg/kg resulted in moderate toxicity, hemorrhage, and congestion of the gastric mucosa (Fig. 1A, B, F, G) as well as normal non-congested gastric mucosa with normal thickness (Fig. 1C, D, E, H).
Histopathological examination
Pretreatment of ethanol-induced rats with C. paniculatum extract and fractions at 100 and 200 mg/kg resulted in tiny regions of moderate necrosis and bleeding restricted to the upper layers of the stomach mucosa, according to histopathological findings (Fig. 2A–H). Similar changes were observed in the omeprazole-treated group (Fig. 2I). The gastric mucosa of the negative control group exhibited many large ulcers with extensive necrosis of the epithelial and glandular cells, bleeding, and varied infiltration of inflammatory cells (Fig. 2J). A normal structure of the gastric mucosa (Fig. 2K) was also observed. The findings reveal mucosal necrosis (black arrow), blood vessel congestion in the lamina propria (red arrow), epithelial cell desquamation, and necrosis (white arrow).
Effects of C. paniculatum extract and fractions on histopathological changes in the stomach of rats with ethanol-induced gastric ulcers. Histopathological changes were analyzed by staining with H&E, followed by observation at ×160 magnification. MECP 100, 200 mg/kg (A, B); HFCP 100, 200 mg/kg (C, D); EFCP 100, 200 mg/kg (E, F); BFCP 100, 200 mg/kg (G, H); omeprazole 20 mg/kg (I); 3% Tween 80 (J); and normal control (K)
Discussion
Peptic ulcers are known to result from an imbalance between offensive and defensive factors [1]. The gastroprotective activity of C. paniculatum methanol extract and its fractions against ethanol-induced ulcers was investigated in this study.
Flavonoids, phenols, tannins, alkaloids, saponins, and terpenoids were found in the phytochemical analysis of the C. paniculatum extract and fractions. These phytoconstituents, particularly flavonoids and tannins, were previously established to be among the possible cytoprotective agents involved in reducing gastric ulcer [30, 31]. The presence of these phytochemicals in the extract and fractions of C. paniculatum may account for its use in the treatment of ulcers.
In this in vivo study, absolute ethanol was deleterious to gastric tissue because it enters the gastric mucosa quickly and readily, causing gastric ulcers [32]. As a result, the ethanol-stimulated gastric lesion model is frequently used to study the etiology of stomach ulcers and assess the gastroprotective actions of medicines [4]. The etiology and progression of ethanol-induced gastric ulcers are linked to increased formation of reactive oxygen species (ROS) and antioxidant (SOD, GSH, CAT) diminution [33, 34]. Superoxide radicals are converted to hydrogen peroxide by superoxide dismutase (SOD), whereas hydrogen peroxide is converted to water and oxygen by catalase (CAT) [35]. GSH acts as a ROS scavenger and a cofactor for GSH peroxidase in the neutralization of hydrogen peroxide by reacting non-enzymatically with superoxide, nitric oxide, hydroxyl radicals, and peroxynitrite [36]. MDA is a frequently used oxidative stress marker formed by the breakdown of cell membrane lipids [37]. The current investigation showed that ethanol induced substantial reductions in GSH concentration as well as SOD and CAT activities. However, pretreatment with C. paniculatum extract and fractions significantly enhanced SOD and CAT activities while simultaneously replenishing diminished GSH levels and lowering MDA levels.
In a recent investigation, we found that the extract of C. paniculatum prevented ulcers from being caused by indomethacin and reduced gastrointestinal motility [16]. As a result, it was hypothesized that C. paniculatum might treat digestive disorders. In the current work, we showed that C. paniculatum extract and fractions prevented damage to the gastric mucosa caused by an ethanol-induced ulceration model, as shown by macroscopic assessment of ulcer lesions, biochemical studies, and histopathologic evaluation. It was discovered that ethanol-induced stomach ulcers responded therapeutically to the extract and fractions of C. paniculatum in a dose-dependent manner.
This confirmed that the C. paniculatum extract and fractions had gastroprotective activities against the formation of ethanol-induced ulcers, demonstrating its antioxidant activity. The substantial free radical scavenging activity of the C. paniculatum extract and fractions may be related to the presence of a considerable number of potent antioxidants, flavonoids, and phenolic compounds.
The negative control group showed severe gastric lesions one hour after absolute ethanol administration, according to the macroscopic and histopathological findings of the gastric tissues. Necrotic tissue injury, loss of gastric mucosa integrity, and an inflammatory response marked by infiltration of inflammatory cells (neutrophils and eosinophils) characterize this damage. However, in animals pre-treated with extract and fractions of C. paniculatum, the microscopic investigation revealed a lower level of infiltration by inflammatory cells, less hemorrhage, and a more regular architecture in the gastric mucosa.
Conclusion
The methanol leaf extract and fractions of C. paniculatum possess significant gastroprotective activity against ethanol-induced ulcers, which further justifies its use in the treatment of ulcers.
Availability of data and materials
Data will be available by corresponding author upon reasonable request.
Abbreviations
- SOD:
-
Superoxide dismutase
- MDA:
-
Malondialdehyde
- GSH:
-
Glutathione
- MECP:
-
Methanol extract of C. paniculatum
- HFCP:
-
N-hexane fraction
- EAFCP:
-
Ethyl acetate fraction
- BFCP:
-
Butanol fraction
- BSA:
-
Bovine serum albumin
- H2O2 :
-
Hydrogen peroxide
- DTNB:
-
Dithionitrobenzene
- TBARS:
-
Thiobarbituric acid reactive substances
- CAT:
-
Catalase
- ROS:
-
Reactive oxygen specie
References
Ugwah MO, Ugwah-Oguejiofor CJ, Etuk EU, Bello SO, Aliero AA (2019) Evaluation of the antiulcer activity of the aqueous stem bark extract of Balanites aegyptiaca L Delile in Wistar rats. J Ethnopharmacol 239:111931. https://doi.org/10.1016/j.jep.2019.111931
Yegen BC (2018) Lifestyle and peptic ulcer disease. Curr Pharm Des 24(18):2034–2040
Simões S, Lopes R, Campos MCD, Marruz MJ, da Cruz MEM, Corvo L (2019) Animal models of acute gastric mucosal injury: macroscopic and microscopic evaluation. Anim Model Exp Med 2(2):121–126
Wu X, Huang Q, Xu N, Cai J, Luo D, Zhang Q, Su Z, Gao C, Liu Y (2019) Antioxidative and anti-Inflammatory effects of water extract of Acrostichum aureum linn: against ethanol-induced gastric ulcer in rats. Biomed Pharmacother 110:554–560
Daniel VT, Wiseman JT, Flahive J, Santry HP (2017) Predictors of mortality in the elderly after open repair for perforated peptic ulcer disease. J Surg Res 215:108–113
Lanas A, Chan FK (2017) Peptic ulcer disease. Lancet 390(10094):613–624
Chakravarty K, Gaur S (2019) Role of probiotics in prophylaxis of Helicobacter pylori infection. Curr Pharm Biotechnol 20(2):137–145
Zhou D, Yang Q, Tian T, Chang Y, Li Y, Duan LR, Li H, Wang S (2020) Gastroprotective effect of gallic acid against ethanol-induced gastric ulcer in rats: Involvement of the Nrf2/HO-1 signaling and anti-apoptosis role. Biomed Pharmacother 126:110075
Benvenutti RC, Dalla Vecchia CA, Locateli G, Serpa PZ, Lutinski JA, Junior SAR, Corralo V, Gutiérrez MV, Vilegas W, Somensi LB, Longo B (2020) Gastroprotective activity of hydroalcoholic extract of the leaves of Urera baccifera in rodents. J Ethnopharmacol 250:112473
Duran Y, Karaboğa I, Polat FR, Polat E, Erboğa ZF, Ovalı MA, Öztopuz RÖ, Çelikkol A, Yılmaz A (2020) Royal jelly attenuates gastric mucosal injury in a rat ethanol-induced gastric injury model. Mol Biol Rep 47:8867–8879
Wang GY, Chen SY, Chen YY, Hong CJ, Hsu YH, Yen GC (2021) Protective effect of rosmarinic acid-rich Trichodesma khasianum clarke leaves against ethanol-induced gastric mucosal injury in vitro and in vivo. Phytomedicine 80:153382
Abera B (2014) Medicinal plants used in traditional medicine by Oromo people, Ghimbi District, Southwest Ethiopia. J Ethnobiol Ethnomedicine 10(1):1–15
Birhanu B, Fikre M, Milkyas E, Addisu D (2018) Phenolic glycoside and steroid from the roots of Combretum Paniculatum. J Nat Sci Res 8:15
.Samdumu FB (2007) Characterization of antimicrobial compounds from Combretum paniculatum, a plant with anti-HIV replication activity. Ph.D thesis, University of Pretoria, South Africa
Hema A, Pale E, Duez P, Luhmer M, Nacro M (2012) Two diglucosylated anthocyanins from Combretum paniculatum flowers. Nat Sci 4(3):166–169
Peter IE, Aroh CM, Shere UG, Ani NI, Adaka IC, Asogwa FK, Isiogugu NO, Abonyi CU, Onwuka AM (2020) Pharmacological actions of methanol leaf extract of Combretum paniculatum Vent. (Combretaceae) on the gastrointestinal system. Trop J Nat Prod Res 4(7):270–275. https://doi.org/10.26538/tjnpr/v4i7.3
Harborne AJ (1998) Phytochemical methods a guide to modern techniques of plant analysis. Springer, Berlin
Sofowora A (2008) Medicinal plants and traditional medicines in Africa. Spectrum books Ltd, Ibadan, p 289
Evans WC (2009) Trease and Evans' Pharmacognosy E-book. Elsevier Health Sciences
Ghorai N, Chakraborty S, Gucchait S, Saha SK, Biswas S (2012) Estimation of total terpenoids concentration in plant tissues using a monoterpene, linalool as standard reagent. Protocol Exchange. https://doi.org/10.1038/protex.2012.055
Marinova D, Ribarova F, Atanassova M (2005) Total phenolics and total flavonoids in Bulgarian fruits and vegetables. J Univ Chem Technol Metall 40(3):255–260
Singleton VL, Rossi JA (1965) Colorimetry of total phenolics with phosphomolybdic-phosphotungstic acid reagents. Am J Enol Vitic 16(3):144–158
Lorke D (1983) A new approach to practical acute toxicity testing. Arch Toxicol 54:275–287
An SM, Park CH, Heo JC, Park JY, Woo SW, Seo JH, Lee MS, Cho KH, Shin HM, Lee SH (2007) Gastrodia elata Blume protects against stress-induced gastric mucosal lesions in mice. Int J Mol Med 20:209–215
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the folin phenol reagent. J Biol Chem 193:265–275
Sinha AK (1972) Colorimetric assay of catalase. Anal Biochem 47(2):389–394
Moron MS, Depierre JW, Mannervik B (1979) Levels of glutathione, glutathione reductase and glutathione S-transferase activities in rat lung and liver. Biochim Biophys Acta 582(1):67–78. https://doi.org/10.1016/0304-4165(79)90289-7
Stocks J, Dormandy TL (1971) The autoxidation of human red cell lipids induced by hydrogen peroxide. Br J Haematol 20(1):95–111. https://doi.org/10.1111/j.1365-2141.1971.tb00790
Misra HP, Fridovich I (1972) The role of superoxide anion in the autoxidation of epinephrine and a simple assay for superoxide dismutase. J Biol Chem 247(10):3170–3175
Bhoumik D, Masresha B, Mallik A (2017) Antiulcer properties of herbal drugs: a review. Int J Biomed Res 8(3):116–124
Yahia M, Yahia M, Benhouda A, Benbia S, Khadraoui H (2017) New gastroprotective activity of methanolic extracts of Hyoscyamus albus (Solanaceae) and Umbilicus rupestris leaves (Crassulaceae) against gastric mucosal injury induced by ethanol in rats. BioTechnol Indian J 13(1):122
Sidahmed HM, Azizan AH, Mohan S, Abdulla MA, Abdelwahab SI, Taha MM, Hadi AH, Ketuly KA, Hashim NM, Loke MF, Vadivelu J (2013) Gastroprotective effect of desmosdumotin C isolated from Mitrella kentia against ethanol-induced gastric mucosal hemorrhage in rats: possible involvement of glutathione, heat-shock protein-70, sulfhydryl compounds, nitric oxide, and anti-helicobacter pylori activity. BMC Complement Altern Med 13:183
Kan J, Hood M, Burns C, Scholten J, Chuang J, Tian F, Pan X, Du J, Gui M (2017) A novel combination of wheat peptides and fucoidan attenuates ethanol-induced gastric mucosal damage through antioxidant, anti-inflammatory, and pro-survival mechanisms. Nutrients 9(9):E978
Liu R, Hao YT, Zhu N, Liu XR, Kang JW, Mao RX, Hou C, Li Y (2020) The gastroprotective effect of small molecule oligopeptides isolated from Walnut (Juglans regia L) against ethanol-induced gastric mucosal injury in rats. Nutrients 12:1138
Vemo BN, Kenfack A, Ngoula F, Nantia EA, Kodjio N, Guiekep AJ, Tsambou AM, Teguia A (2017) Effects of ethanol extract of Bersama engleriana leaves on oxidative stress and reproductive parameters in male Guinea pig (Cavia porcellus) exposed to cypermethrin. Int J Biol Chem Sci 11(5):2243–2253
Beiranvand M, Bahramikia S (2020) Ameliorating and protective effects mesalazine on ethanol-induced gastric ulcers in experimental rats. Eur J Pharmacol 888:173573
Dursun H, Bilici M, Albayrak F, Ozturk C, Saglam MB, Alp HH, Süleyman H (2009) Antiulcer activity of fluvoxamine in rats and its effect on oxidant and antioxidant parameters in stomach tissue. BMC Gastroenterol 9:36
Acknowledgements
We want to acknowledge the contributions of all the academic and non-academic staff of the Department of Pharmacology and Toxicology, Faculty of Pharmaceutical Sciences, University of Nigeria Nsukka.
Funding
No financial support.
Author information
Authors and Affiliations
Contributions
PIE designed the study, U. CS performed the experiment and collected the data. PIE, UCS, OAM, MFN, OMN, OCA, and PFU prepared and edited the manuscript. Statistical analysis was performed by PIE and OAM. Similarity check was performed by PIE and OAM. All authors have read and agreed to the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The experimental procedures were approved by the Faculty of Pharmaceutical Sciences, University of Nigeria's ethics committee (FPSRE/UNN/19/00015) and were in accordance with the National Code of Conduct for Animal Research Ethics (NCARE).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Emmanuel, P.I., Sandra, U.C., Marytheresa, O.A. et al. Gastroprotective effects of Combretum paniculatum (Combretaceae) leaf extract and fractions on absolute ethanol-induced gastric ulcer in rats. Futur J Pharm Sci 8, 54 (2022). https://doi.org/10.1186/s43094-022-00442-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43094-022-00442-4