Abstract
Background
In recent years, the field of nanotechnology and nanomedicine has transformed the pharmaceutical industry with the development of novel drug delivery systems that overcome the shortcomings of traditional drug delivery systems. Nanostructured lipid carriers (NLCs), also known as the second-generation lipid nanocarriers, are one such efficient and targeted drug delivery system that has gained immense attention all across due to their myriad advantages and applications. Scientific advancements have revolutionized our health system, but still, brain diseases like brain tumour have remained formidable owing to poor prognosis and the challenging drug delivery to the brain tissue. In this review, we highlighted the application and potential of NLCs in brain-specific delivery of chemotherapeutic agents.
Main body
NLCs are lipid-based formulations with a solid matrix at room temperature and offer advantages like enhanced stability, low toxicity, increased shelf life, improved drug loading capacity, and biocompatibility over other conventional lipid-based nanocarriers such as nanoemulsions and solid lipid nanoparticles. This review meticulously articulates the structure, classification, components, and various methods of preparation exemplified with various research studies along with their advantages and disadvantages. The concept of drug loading and release has been discussed followed by a brief about stability and strategies to improve stability of NLCs. The review also summarizes various in vitro and in vivo research studies on NLCs encapsulated with cytotoxic drugs and their potential application in brain-specific drug delivery.
Conclusion
NLCs are employed as an important carrier for the delivery of food, cosmetics, and medicines and recently have been used in brain targeting, cancer, and gene therapy. However, in this review, the applications and importance of NLCs in targeting brain tumour have been discussed in detail stating examples of various research studies conducted in recent years. In addition, to shed light on the promising role of NLCs, the current clinical status of NLCs has also been summarized.
Graphical Abstract

Similar content being viewed by others
Background
A brain tumour is characterized by the development of an abnormal cellular mass in the brain tissue which can be malignant or non-malignant (benign) [1]. Benign tumours show slow growth and do not invade other tissues, while malignant tumours have rapid growth and invade other tissues posing a greater challenge. Gliomas and glioblastoma multiforme are the most common types of malignant brain tumours, accounting for around 80% of the total malignant tumours [2]. Despite decades of study, brain tumours are still one of the most lethal cancers with a dismal prognosis and a high risk of recurrence [3]. The high rate of mortality can be attributed to the rapid progression, late detection due to the presence of common nonspecific symptoms like headache and limited availability of highly specialized equipment required for diagnosis, and limited therapeutic possibilities due to the intricate and complex brain structure. Regardless of the poor prognosis and high mortality of brain tumours, current treatment strategies offer only palliative care [4]. The existence of a blood–brain barrier (BBB) is one of the critical difficulties in treating brain tumours. The blood–brain barrier is a protective and highly selective layer of endothelial cells that limits the entry of pathogenic organisms and unwanted substances/molecules into the brain while allowing the supply of oxygen and other nutrients required for the proper functioning of the brain [5]. The BBB is highly selective and nearly impermeable and comprises various molecular components and transport systems that work together to form efflux mechanisms, or barriers, that prevent medicinal compounds from entering the brain [6]. The structure of BBB gets disrupted in the case of brain tumours and is known as the blood–tumour barrier (BTB). Although BTB was reported to be leakier than BBB, it is still heterogeneously permeable to the medications, allowing only the passage of small-sized molecules to the brain [4]. Additionally, molecular efflux from the central nervous system (CNS) compartment to the blood is also mediated by several membrane transporters like P-glycoprotein situated in the barrier [7]. Drugs with a molecular weight of fewer than 500 daltons and high lipophilicity can be delivered systemically and readily cross the BBB. However, because only 5% of medications fit these criteria, effective drug delivery systems are required to transport the remaining 95% of medications into the brain [8, 9]. The existing traditional drug delivery systems that release the drug into the systemic circulation fail to deliver it effectively to the brain. Even the effective anti-neoplastic medications like methotrexate, paclitaxel, docetaxel, etc., belong to Biopharmaceutical Classification Class-IV and are limited by minimal aqueous solubility, poor permeability across the lipoidal bilayer barrier, erratic absorption, and low bioavailability [10]. Therefore, there is a pressing need to develop and design new approaches for treating brain diseases that specifically and effectively target the brain tissue.
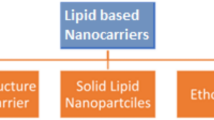
In the search for a novel drug carrier that can cross the blood–brain barrier, researchers have formulated various drug delivery systems ranging from macro- to nanoscale. Some widely explored delivery systems are micro- and nanoemulsion, polymeric nanoparticles, liposomes, transferosomes, and lipid nanoparticles like solid lipid nanoparticles (SLNs) and nanostructured lipid carriers [11]. Although all of these have great applications and are widely used, all these systems have their shortcomings [12,13,14]. Thus, it becomes very challenging to develop a promising delivery system for various cytotoxic drugs and other therapeutic agents to deliver them into the brain. However, lipid nanoparticles owing to their several benefits like small size, high drug loading capacity, high surface-to-volume ratio, easy functionalization, and enhanced permeation across BBB have become a centre of attraction [15].
Main text
Nanostructured lipid carriers
Nanoparticles are a type of particulate system having a size ranging from 10 to 1000 nm [16]. Solid lipid nanoparticles, the first-generation nanocarriers, were designed by Professor R.H. Müller and Professor M. Gasco in the early 1990s [17]. These are the simulation of oil in water nanoemulsions in which the internal oily phase is substituted by the solid fats to minimize the limitations associated with the conventional lipid-based formulations (Fig. 1) and has multitudinous benefits like avoiding the use of organic solvents during preparation, stability against hydrolysis of drug and comparatively stable during storage [18, 19]. However, SLNs as drug carriers were limited by drug expulsion on storage due to their rigid structure, unpredictable gelation tendency, particle growth, and unexpected polymeric transitions (triglycerides used for their fabrication undergo α (alpha), β (beta), and β′ (beta prime) crystal modification during their preparation and storage) [20,21,22].
To overcome the drawbacks associated with the solid lipid nanoparticles, nanostructured lipid carriers were developed. The solid lipids in the SLNs were replaced by the blend of liquid and solid lipids varying in a ratio of 70:30 up to a ratio of 99.9:0.1 [23]. Regardless of the presence of liquid lipids in a high proportion, the NLCs are solid at room temperature. The blend of solid and liquid lipids gives rise to an unstructured matrix with more imperfections that holds a greater number of drug molecules than SLN and thus has high entrapment efficiency. The other advantages of NLC over SLN include low toxicity, drug protection, and reasonably more stability upon storage [24]. Due to the presence of less water content, NLC is less inclined to unexpected gelation which is a significant problem in the case of SLNs [25].
NLCs in brain targeting
BBB limits the delivery of drugs to brain, and hence, strategies to surpass this natural defence of our body are the key factor to deliver drug to brain tissues. The following qualities of NLCs make them a promising tool for brain targeting:
-
(i)
Small size The size in nano ranges enable the NLCs to easily transport and internalize through the microvasculature of brain via endocytosis/transcytosis transport mechanism [26].
-
(ii)
Lipid solubility Almost all drugs for the brain presently in clinical practice are lipid-soluble small molecules. They can cross through lipid-mediated free diffusion across the BBB. It can be used to even coat/load a water-soluble drug and deliver to brain [27].
-
(iii)
Shielding labile drugs from degradation and improving bioavailability NLCs have shown to significantly enhance the encapsulation efficiency for labile hydrophilic and hydrophobic drugs like curcumin. It protects them from degradation in the body, improve their oral bioavailability, and release drug in a controlled manner [28].
-
(iv)
Potential to increase stability and penetration using polymeric coatings The NLCs are rapidly cleared by blood and the reticuloendothelial system (RES). This can be reduced with surface modified by particular hydrophilic polymers. Thus, the penetration and circulating half-life of drugs into BBB can be increased by coating SLNS with hydrophilic polymers like poloxamer, polyethylene glycol (PEG), or amphipathic polymers with the hydrophilic part covering the surface and the lipophilic part inside the core. Increased penetration to BBB and enhanced drug delivery to the CNS were demonstrated by a comparative study of SLNs and PEG-modified SLNs loaded with antitumour drugs like camptothecin and doxorubicin [29].
-
(v)
Active targeting Active targeting involves modification tools such as carriers like proteins/ligands or receptors to allow the carrier or receptor-mediated transport through the BBB. The ligand is chosen to bind to a receptor overexpressed by tumour cells or tumour vasculature and not expressed by normal cells. High drug retention in the tumour tissue along with a reduction in dose-related side effects are the main advantages [30].
-
(vi)
Passive targeting Abnormalities in tumour vessels lead to enhanced vascular permeability and leaky vasculature where the administered nanocarriers extravasate and get concentrated in the interstitial space. This retention by passive phenomenon is termed as ‘Enhanced Permeability and Retention’ effect. This effect was shown by Tsai et al. by developing baicalein-loaded tocol NLC that demonstrated enhanced and sustained brain delivery of baicalein [31].
-
(vii)
Controlled release Unfortunately, the presence of active efflux transporters in BBB limits the therapeutic efficacy of drugs capable of entering the brain. To overcome this, a slow controlled release through NLCs can be used so as to achieve a steady drug concentration [27].
Classification of NLCs
Due to the polymeric transitions of triglycerides to a highly ordered β or β′ state, the drugs expel from the carrier upon storage as it abandons a little space for the active pharmaceutical ingredients. To eschew this problem, the vesicle must contain a controlled nanostructure that creates enough space to accommodate the drug molecules [32]. Based on where the drug is going to incorporate, three different types of structure that can arise (Fig. 2) [33, 34]. These are:
-
NLC Type I, also known as the imperfect type
-
NLC Type II, also known as the multiple types
-
NLC Type III, also known as the amorphous type.
NLC type I
These are also known as imperfect crystal types due to their unstructured matrix. It is these imperfections that create ample space to integrate drugs and has high entrapment efficiency. In this case, the amount of liquid lipid used as compared to solid lipids is less. Solid lipids and the oils are mixed and blended to form an oil/water (o/w) nanoemulsion that yields lipid particles upon cooling to room temperature [35, 36].
NLC type II
In type II NLCs, high concentrations of oils are used compared to solid lipids. As a result of high oil concentration during formulation, a miscibility gap occurs between the two lipids (solid lipid and oil). When these lipids are cooled, phase separation occurs due to the precipitation of small oily nano-compartments which are surrounded by the solid lipid matrix [36]. The type II NLCs are helpful in the controlled release of the drug from the matrix [18].
NLC type III
In type III NLCs, the central matrix is solid but in an amorphous state. The oils and solid lipids are blended in such a manner that the central core remains amorphous. This is done to avoid the crystallinity in the matrix to prevent the drug expulsion or to reduce the process of drug leaking as crystallization often leads to drug expulsion [35, 36]. The special lipids like hydroxyoctacosanyl hydroxy stearate, isopropyl myristate, and dibutyl adipate are used to formulate the type III NLCs as these lipids do not undergo crystallization during the homogenization and cooling of the nanoemulsion [37].
Composition of nanostructured lipid nanocarriers
The composition and process parameters play an essential role in the regulation of particle size, drug entrapment efficiency, and drug release profile. The researchers have cleverly exploited process parameters and composition to achieve desired effects [38]. To exemplify, it has been observed by Muchow et al. that small-sized NLCs (200 nm) showed a higher area under curve values when compared to higher sized NLCs (600 nm) on oral administration in rats due to the higher mucoadhesion capability of small-sized NLC in the body [39]. The degree of crystallization of various lipids used for the formulation also affects the drug entrapment and loading capacity [40].
A variety of lipids comprising both liquid and solid lipids and surfactants are used at a specific ratio for the preparation of NLCs. The materials chosen for the production must be biocompatible, well-tolerated, non-toxic, and biodegradable [18]. The lipid is the primary component responsible for the stability, drug loading capacity, and controlled release behaviour of the NLCs. A variety of lipids including fatty acids, waxes, and glycerides are used to develop NLCs (Table 1) [41, 42].
Methods of preparation of NLCs
Generally, the formulation of NLCs involves the emulsification of the lipophilic phase consisting of a mixture of solid lipids and liquid lipids, with the aqueous phase having surfactant or emulsifiers [52]. The ratio of solid lipids to liquid lipids ranges from 70:30 to 99.9:0.1, and this highly dynamic system is stabilized by surfactant solutions whose concentration lies between 0.5 and 5% [53]. There are several methods used for the preparation of nanostructured lipid carriers. Some of these methods include:
-
High-pressure homogenization (HPH)
-
Solvent emulsification evaporation method
-
Solvent emulsification diffusion method
-
Solvent injection method
-
Microemulsion method
-
Double emulsion technique
-
Ultrasonication or high-speed homogenization
-
Phase inversion method
-
Membrane contractor technique
-
Supercritical fluid (SCF) method
-
Hot-melt extrusion (HME) technology
High-pressure homogenization
It is one of the extensively used methods for the large-scale production of NLCs. In this method, the lipids are pushed through narrow pores under high pressure. The high shear stress on the lipids disrupts the lipids to submicron ranges [54]. Generally, the lipids are within the 5–10% range. High-pressure homogenization can be performed at both elevated temperatures and below room temperature, known as hot high-pressure homogenization and cold high-pressure homogenization, respectively [55].
-
(i)
Hot HPH This method is appropriate for insoluble and hydrophobic drugs and thus is widely exploited for encapsulating the lipophilic drugs into NLCs [56]. The process begins with melting the solid lipids at a temperature of 5–10 °C above their melting point. To this, liquid lipids and the active pharmaceutical ingredient (API) are added, and dispersion is made. This mixture is then dispersed in the aqueous solution of surfactant/emulsifier, which is previously heated at the same temperature with the help of high shear mixer to form a pre-emulsion. The pre-emulsion so formed is then introduced in piston gap homogenizer at controlled temperature and pressure. The nanoemulsion will be formed and cooled at room temperature to yield nanoparticles [57,58,59].
HPH offers several advantages, such as higher processing temperatures resulting in smaller particle sizes due to the lipid phase's reduced viscosity [60]. This method is suitable for both laboratory scale and large scale and has a low polydispersity index. However, this technique has some pitfalls too. This process may lead to the degradation of heat-sensitive drugs [60]. As most of the surfactants have cloud points less than 85°C, this may cause a reduction in the emulsifying capacity of surfactants due to high temperature and hence imparts instability to NLCs [17]. More to above, it was reported that elevated temperature or increased number of the cycles during the process could lead to particle size growth owing to the high kinetic energy of the particles [61]. Another drawback of this approach is the drug's penetration into the aqueous phase during the homogenization and the intricacy of the nanoemulsion crystallization stage [62].
-
(ii)
Cold HPH There are various disadvantages associated with the hot HPH, and to vanquish those demerits, HPH can be carried at below room temperature and is known as cold HPH. This technique involves the solidification of lipid melt along with the drug using liquid nitrogen or dry ice. The solid mass is then milled and grounded to microparticles (50–100 μm) and dispersed in a cold aqueous surfactant solution. This solution is then homogenized to yield nanoparticles [20, 56]. Although this process reduces the thermal exposure, the nanoparticles obtained are of variable sizes [63]. This technique may be utilized for loading both hydrophilic and lipophilic medicines into NLCs due to the low likelihood of drug diffusion into the aqueous phase [64].
Solvent emulsification evaporation method
This method can be employed for sizes ranging from 30 to 100 nm depending upon the types of lipids and surfactants used [65]. In this process, the drug accompanying the lipids is added to organic solvent (water-immiscible) and emulsified with an aqueous solution of surfactant to form an o/w emulsion. The organic solvent is then removed by evaporation at low pressure that eventually forms NLCs due to lipid precipitation by aqueous media on evaporation of the organic solvent (Fig. 3A) [66]. This method is ideal for heat-sensitive medicines since it is devoid of thermal stresses. The most significant limitation of this process is the usage of organic solvents, as sometimes residues of organic solvents remain in the final product, which may produce toxic effects after administration [56]. It was also reported that homogenization effectiveness gets reduced with an increase in the lipid concentration, resulting in highly dilute dispersions with very low lipid particle contents [64].
Solvent emulsification diffusion method
This method uses partly water-miscible solvents (such as ethanol, benzyl alcohol, tetrahydrofuran) as a means of dispersing the lipids and the drugs [67]. This process begins with the mutual saturation of the solvent and water so as to maintain the thermodynamic equilibrium. Afterwards, API and lipids are added and emulsified to form an o/w emulsion. The emulsion is then diluted with water in a ratio varying from 1:5 to 1:10 to allow solvent diffusion into a continuous phase, thus precipitating the nanoparticles (Fig. 3B). The excess solvent can be removed by either lyophilization or ultrafiltration after the precipitation of NLCs [57, 67].
Solvent injection method
This technique is also known as the solvent displacement method. It works on the principle of quick diffusion of solvent over lipids interfaced with an aqueous solvent. In this method, both the solid and liquid lipids are added to water-miscible solvent (alcohols like ethanol, isopropyl alcohol) or a mixture of water-miscible solvents and speedily injected into the surfactant solution with continuous stirring. As a result, the lipid nanoparticles get precipitated in the aqueous solution as the solvent migrates quickly through it [68].
This method is versatile and has a faster production rate, low shear stress, and high efficiency without using sophisticated equipment like a high-pressure homogenizer. However, particle size can be a concern with lipophilic solvents as more lipophilic solvents produce larger particles. The possibility of organic solvent residues can be another issue with this method [63, 69].
Microemulsion method
It is a popular method used for both polar and non-polar drugs. It involves the addition of melted lipids to an aqueous solution of the drug along with a surfactant and co-surfactant to form an emulsion, the nature of which depends upon the ratios of hydrophilic and lipophilic phase used. The resulted emulsion is dispersed in chilled water in a ratio from 1:25 to 1:50 under mild agitation, ultimately giving NLC dispersion (Fig. 4) [70,71,72]. Even though this method is simple, time-saving and can be used for thermolabile substances, it is associated with various limitations like usage of large volumes of water for dilution and requires an appreciable quantity of surfactants for formulation [73, 74].
Double emulsion technique
This method is extensively employed for hydrophilic drugs as well as for thermosensitive drugs [75]. In this approach, a hydrophilic drug in aqueous media is emulsified in lipid melt, with lipophilic surfactants to form w/o emulsion. The primary emulsion is then added to an aqueous solution of hydrophilic solvent to form w/o/w emulsion (double emulsion); thereupon, the NLCs are purified from the dispersion by solvent evaporation and ultrafiltration [75, 76]. Although this method is simple, requires a modest energy input and there is no need for sophisticated instruments, it is only suitable for systems with a low lipid content [77].
Ultrasonication or high-speed homogenization
This method works on the principle of cavitation and is one of the least studied techniques. Firstly, the lipids are melted, and the active drug is added to them. This melt is added to the surfactant solution previously heated to the same temperature, followed by emulsification using a high-speed stirrer. The obtained pre-emulsion is further ultrasonicated with the help of a probe ultrasonicator. The dispersion is cooled to get the lipid nanoparticles [78,79,80]. This technique saves both time and energy, but NLCs obtained from ultrasonication suffer from several shortcomings like contamination by metals, clumping of particles on storage, and low stability of NLCs [80,81,82].
Phase inversion temperature method
As the name suggests, this technique is based on the principle of temperature-induced phase inversion of an emulsion. In this process, non-ionic polyoxyethylated surfactants are used whose properties are dependent on the temperature. At low temperatures, the hydrophilic–lipophilic balance (HLB) value of these surfactants is high because of the hydration of the hydrophilic groups. But as the temperature increases, their HLB value starts to decrease because of the dehydration of the ethoxy groups. There is a point (temperature) where the surfactant molecule has an equal affinity towards both lipophilic and hydrophilic phases, and this temperature is known as phase inversion temperature [83,84,85]. When the temperature is above the phase inversion temperature, w/o-type emulsion is formed and vice versa [86]. The lipids, oils, water, and surfactants are mixed and heated above the phase inversion temperature, followed by stirring using a magnetic stirrer to form a w/o emulsion. Subsequently, three cycles of heating and cooling (85 °C–60°C–85 °C) are applied at a rate of 4 °C/min. This hot mixture is then diluted with cold water to allow phase inversion (from w/o emulsion to o/w emulsion) and leads to the formation of NLCs [86, 87]. This is a novel method offering the advantage of incorporating thermolabile drugs without using any organic solvent [88, 89].
Membrane contractor method
It is a relatively recent approach for the production of NLCs. The procedure involves heating the lipid phase to a temperature over its melting point in a pressured tank. The liquid is then passed down a tube and pushed against membrane pores, resulting in the production of tiny droplets. The aqueous phase sweeps away any droplets accumulating at the pore outputs as it circulates inside the membrane module. The dispersion so obtained is cooled to precipitate the NLCs. The particle size is determined by the temperature of the lipid and aqueous phases, the membrane aperture size, and the lipid phase pressure. The advantages of this technique include the ability to regulate particle size by varying the process parameters and the simplicity of scale-up [90, 91]. However, clogging of the membrane is the only problem with this procedure [92].
Supercritical fluid (SCF) method
A wide range of applications, such as extraction, green chemical reactions, and chromatography, have made use of supercritical fluids. Recently, this technology has been explored for the formation of micro- and nanoparticles. However, the use of supercritical fluid technology in particle production is still in its early stages of development.
A supercritical fluid is a liquid or gas that can coexist at temperatures and pressures above the critical temperature and critical pressure. It has characteristics that are distinct from those of gases or liquids under normal circumstances [93]. Supercritical carbon dioxide is one of the widely used SCFs owing to its abundance, inertness, non-flammable, and easily attainable critical conditions (Tc = ~ 31 °C and Pc = 73.8 bar) [94]. Generally, the solid lipids are melted and added to SCF along with the drug and liquid lipids to solubilize them. Either a gas-saturated suspension or a solution is formed depending on the components' solubility in the SCF. Afterwards, the resultant dispersion is atomized and is sprayed in an enclosed chamber, where the decompression and evaporation of the gas lead to the formation of nanostructured lipid carriers [95]. Chattopadhyay et al. employed a different technique (SCF extraction of emulsions) for preparing NLCs using SCF. The research group formed an o/w emulsion, which was added to the extraction column and extracted using supercritical carbon dioxide. There is a rapid and complete removal of the solvent, resulting in the precipitation of NLCs. In addition, it was reported that the NLCs formed had a uniform particle size [96].
SCF method offers numerous benefits, including the avoidance of organic solvents and the production of dry powder particles rather than suspensions. Also, as the density of SCFs fluctuates with pressure, a simple depressurization process with pressure adjustments may be used to separate and recover the solvent [97].
Hot-melt extrusion (HME) technology
It is one of the most widely used processing techniques in the plastic industry. Earlier, the HME method was used for manufacturing tubes, plastic bags, and pipes. However, since the 1980s, there has been a rising interest in the use of HME in the pharmaceutical industry and has now been used for manufacturing tablets, capsules, implants, etc. [98]. This method involves pumping the APIs and excipients with a heated rotating screw (extruder) at a higher pressure and is passed through a die to form uniform-sized nanoparticles. An emulsion is formed when the APIs and excipients are passed through an extruder, and afterwards, the size of the obtained emulsion is reduced by passing through the die [99, 100].
HME method has several advantages, such as no solvents are used in this method; hence, there is no need for the drying process. Also, it is used for enhancing the solubility and bioavailability of hydrophobic drugs. Furthermore, it is a cost-effective method that involves a shorter manufacturing time, fewer stages, and continuous operation. HME is chosen over other fusion processes because the mixture's residence time in the extruder is short, preventing deterioration of heat-sensitive components [99, 101]. HME, on the other hand, is performed at high temperatures that cannot be used to formulate thermolabile compounds. HME requires excipients with high flow properties. Additionally, the equipment is relatively expensive, and the driving unit requires a significant amount of energy. However, the majority of these drawbacks may be mitigated by adjusting process parameters appropriately [99, 101, 102] (Table 2).
Methods of drug loading in NLCs
Depending upon the position of the drug in the nanocarrier, there are three ways by which a drug can be encapsulated in NLC. These three models of drug encapsulation are the homogeneous matrix model, drug-enriched shell model, and drug-enriched core model (Fig. 5).
Homogenous matrix model
This model is also known as the solid solution model. In this system, the drug molecules are homogeneously scattered in the lipid matrix, in the form of either molecules or amorphous clusters [24]. This type of drug encapsulation is seen when the cold homogenization technique is used without surfactants [178]. An example of this model is a betamethasone dipropionate-loaded NLC prepared by Hanna et al., which could release the drug inside the deeper layers of the skin [179].
Drug-enriched shell model
In this type, the drug molecules are concentrated near the shell, while the lipid matrix is free from the drug. This type of drug encapsulation occurs when a phase separates during the cooling of the solution and lipids precipitate out, giving a drug-free lipid core. At the same time, the drug repartitions in liquid lipids, thus concentrating the drug molecules in the outer core [22, 180]. This type of NLCs shows burst release [24, 80]. Uprit et al. synthesized NLCs encapsulated with minoxidil in which the drug is concentrated in the shell and showed an initial burst drug release followed by the sustained release of the drug [181].
Drug-enriched core model
In this system, the drug molecules are condensed in the central core of the nanostructured lipid carriers. These nanoparticles exhibit prolonged release owing to the saturation solubility of API in lipids, and this release is governed by Fick’s first law of diffusion [178]. This system can be formulated when the drug precipitates before the lipid. One way of forming this type of structure is to liquefy the drug in the lipid till its saturation solubility and form a nanoemulsion. When this emulsion is cooled, the drug becomes supersaturated in the lipid melt and precipitates the drug before the precipitation of lipids [180, 182, 183].
Drug release from nanostructured lipid carriers
The drug release from the NLCs depends upon various factors such as partition coefficient of the drug molecule, production temperature, type and concentration of the emulsifier used, and the production technique [45]. Besides these factors, polymer degradation and diffusion of the drug from the matrix are the significant factors governing drug release from NLCs. This release can also be triggered by various impulses like increasing temperature or water evaporation of NLCs [184]. This property is well exploited in the treatment of various skin disorders like psoriasis and eczema. Cyclosporine lipid particles cream is used topically for the treatment of psoriasis. When the cream is rubbed against the skin, it increases the temperature and leads to the evaporation of water from the formulation, leading to better penetration of cyclosporine into the skin [185]. This triggered impulse converts the NLCs into ordered structures, thus expelling the drug from the matrix and initiating the desired burst release. The initial burst is due to the accumulation of the drug in the outer shell followed by a sustained drug release which is due to the drug entrapped in the lipid matrix. This biphasic release is helpful in diseases like cancer, where an initial burst release serves as the primary immediate dose followed by the sustained release of the drug at the tumour site [18, 186, 187]. Melatonin-loaded nanostructured lipid carriers prepared exhibit biphasic drug release in vivo, showing a burst release in the first 2 hours accompanied by sustained release in 48 h in which 92% of the drug is released [188]. In the case where the nanoparticles are coated with polymers, the drug release is then governed by diffusion of drug across the polymeric membrane as the polymeric layer acts as a barrier for the drug [189, 190].
Apart from these, the drug release from NLCs also depends on the following factors:
-
(i)
Particle size The nanoparticles having smaller particle size exhibit faster release rates because of their greater surface area [63]. Additionally, in a study by Loo et al., it was reported that smaller-sized NLCs had greater physical stability than large-sized particles [191].
-
(ii)
Lipid matrix The type of lipid used for the production of NLCs also affects the drug release rate as every lipid has its melting point and HLB value, which in turn affects the affinity of drug binding with lipid. Nanjwade et al. synthesized NLCs using two different solid lipids (Precirol ATO 5 and Compritol 888) and studied their effects on the formulation and drug loading efficiency of NLCs. It was observed that NLCs in which Preciol ATO 5 was used as solid lipid had a smaller particle size with higher drug loading and entrapment efficiency [192]. Similarly, in another study by Teng et al., NLCs fabricated using Precirol ATO 5 as solid lipid were found to be smaller in size and had higher entrapment efficiency than the NLCs prepared using glyceryl monostearate [193].
-
(iii)
Surfactant Surfactants affect the physicochemical properties of the lipid nanoparticles owing to the interactions between lipid and surfactant used. Surfactants reduce the surface tension between the interface of the particles, inducing particle portioning and thus increasing surface area. The surfactant concentration highly influences the particle size of lipid nanoparticles. When a higher surfactant/lipid ratio was selected, smaller particle sizes were observed in general. During storage, a decrease in surfactant concentration may result in an increase in particle size [194]. Mura et al. investigated the effect of different surfactants (Pluronic F68, Tween 80, and Gelucire) on the physical and chemical characteristics of NLCs. The results revealed that when Gelucire was used, NLCs formed were of the smallest size (< 100 nm) as compared to tween 80 (> 500 nm) and Pluronic F68 (300–400 nm). When utilizing Gelucire in conjunction with either tween 80 or pluronic, a further reduction in nanoparticle size was seen along with an increase in homogeneity [195].
-
(iv)
Drug loading The type by which a drug is loaded into NLC affects the drug release. Drug-enriched shell-type drug loading shows immediate release, while the drug-enriched core system shows sustained release [196, 197].
-
(v)
Use of auxiliary ingredients The use of auxiliary ingredients during the formulation can impact the drug release profile of NLCs due to their interaction with the active molecules. In case of an auxiliary ingredient and drug interactions to form a less water-soluble complex, the system will show only sustained release with almost zero burst release [190].
-
(vi)
Stirring time Stirring should be performed for an optimal time to form a smooth nanoemulsion as less stirring results in the formation of larger-sized particles [194].
-
(vii)
Temperature The desired formulating temperature must be 5–10 °C above the melting point of solid lipids. The solid will not melt if the temperature is below the melting point, making it impossible to integrate the drug within NLCs. The lipid, on the other hand, will degrade if the temperature is high [194].
-
(viii)
Preparation method The preparation method used for the fabrication of NLCs influences the particle size of the nanoparticles, which in turn affects the polydispersity index and zeta potential of the formulation. When hot HPH is used, the aqueous solubility of the drug increases, and when the solution is cooled, the lipid phase undergoes repartitioning. At the recrystallization temperature, a solid core forms, and the crystallized core is no longer available for drug repartitioning; thus, the drug accumulates in the shell or onto the surface of the nanoparticles, resulting in burst release. In contrast, NLCs prepared by cold HPH exhibit prolonged drug release due to the formation of core-enriched NLCs [63].
Stability of nanostructured lipid carriers
Although NLCs represent a perfect delivery system for both hydrophilic and hydrophobic drugs, they are still associated with some unresolved issues like an increase in particle size, drug expulsion from the matrix, greater lipid transitions and modification, aggregation due to incompatible lipids, and gelation of the dispersion upon long-term storage, all of which limit their market availability [198]. Measurement of the particle size (by dynamic light scattering, laser diffraction, photon correlation spectroscopy), zeta potential, and thermal analysis (by differential scanning calorimetry) are some of the ways used to determine the physical stability of the NLCs [199].
A major problem with SLNs is their aggregation on long-term storage. When highly concentrated NLC dispersions are stored, they interlink and form a pearl-like network, thereby fixing their position and restricting their movement, making it impossible for them to undergo collision and perikinetic flocculation. When these dispersions are administered, it will get diluted with body fluids like gastrointestinal fluid or plasma depending upon the route of administration and releases single non-aggregated particles (Fig. 6). On the contrary, in less concentrated nanoparticle dispersion, particles collide with each other and aggregate [24, 200].
Stabilization effect in highly concentrated lipid particle dispersions (This figure has been adopted and modified from reference [24])
Strategies used for enhancing NLC stability
-
(i)
Lyophilisation It is one of the most efficient ways to amplify the stability of nanoparticles, especially of NLC loaded with hydrolysable drugs. This is mostly used to prevent Ostwald ripening and to avoid the hydrolysis of moisture-sensitive drugs [201]. However, if the process of lyophilization is used without cryoprotectant, it would result in the aggregation of the lipid particles [201, 202]. Some of the commonly used cryoprotectants are polyhydroxy sugars like sorbitol, glucose, mannitol, lactose, sucrose, mannose, and trehalose [202].
-
(ii)
Spray drying It is an alternative to lyophilization and cheaper also. The lipid nanoparticles are spray-dried for improving their physical and chemical stability. The resultant powder can be stored for a long period of time or can be used to develop other formulations such as tablets or capsules [203]. Care must be taken before the spray drying of NLCs can be done only when the melting point of lipids is greater than the boiling point of the spraying liquid used to prevent the degradation of the lipids. Ethanol–water or polyvinylpyrrolidone–water mixture can be employed instead of pure water to minimize the melting of thermosensitive lipids [204].
-
(iii)
Addition of Poloxamers Poloxamer is a non-ionic triblock polymer that is made up of poly(ethylene oxide)–poly(propylene oxide)–poly(ethylene oxide) chains [205]. There are different grades of poloxamers used as a stabilizing agent. These are widely used to enhance the stability of nanoparticle gels. Poloxamer 188 increases the mechanical stability of nanoparticles, while poloxamer 407 when comes in contact with organic solvents like ethanol and propylene glycol self-assembles into micellar cubic and hexagonal structures, and these structures are thermodynamically stable [206, 207].
-
(iv)
Addition of PEG Nanoparticles are coated with hydrophilic substances like PEG 4000 as it provides a gut of benefits like [206, 208]
-
Imparts good physical stability
-
Enhances colloidal stability in body fluids
-
Improves dispersibility of colloids
-
Expedites the transport of colloids across tissues
-
Reduces the modification of lipids as well as growth of NLCs
-
Increases blood circulation time
-
Aids in specific drug delivery and drug targeting by modifying the interactions of colloids with the mucosal membrane.
-
In vivo fate of NLCs
The understanding of the in vivo ADME (absorption, distribution, metabolism, and excretion) of NLCs is critical for ensuring their effectiveness, safety, and reliability. In fact, a thorough and systematic investigation of the pharmacokinetic data can lead to [209]
-
A greater grasp of the drug's fundamental pharmacokinetic characteristics, notably in the disease matrix of the target patient population.
-
A greater knowledge of the potential interactions between NLCs and tissues.
-
Evaluation of potential approaches to alter the ADME of nanoparticles in order to improve the drug's safety and effectiveness.
Despite the significant progress made in the production of NLCs, only a few studies have focused on the ultimate fate of these lipid nanoparticles (LNPs) once they enter the body, and hence, there is a dire need for in vivo pharmacokinetics studies to pass the regulatory hurdles as well as for commercialization. The below section illuminates the in vivo fate of LNPs as found in the published literature.
The in vivo fate of LNPs depends upon a number of factors, the route of administration being the most important. It was reported that LNPs have adhesive properties, allowing them to stick to the gut wall and release medicines for direct absorption into the enterocytes [210]. This was confirmed by Beloqui et al. The authors studied the fate of spironolactone NLCs following oral administration. To underline the exact absorption mechanism of prepared NLCs, the authors studied the biodistribution studies using 99mTc radiolabelled NLCs and reported that spironolactone NLCs adhered to the gut wall and were subsequently taken up by the epithelial cells present in the small intestine [211]. In parallel, after oral administration, the LNPs boost the secretion of lipase or co-lipase in the duodenum. Lipases, which are found in numerous organs and tissues, are probably one of the most significant enzymes responsible for the breakdown of LNPs. Triglycerides, an integral component of NLCs, are broken down into diglycerides, which are further broken into monoglycerides and finally into the fatty acid micelles in the GIT (gastrointestinal tract) [212]. These formed micelles resolubilize the drug that is released during the breakdown of LNPs in the GIT. Additionally, the bile salts combine with these micelles to form mixed micelles, that aid in the absorption of these colloidal particles by enterocytes, transporting the medicine into the cells. Together, these absorption mechanisms are referred to as the “Trojan Horse effect” [213]. Following their absorption, these micelles are converted to chylomicrons in the enterocytes by re-esterification via the monoacyl glycerol or phosphatidic acid pathways, followed by phospholipid stabilization. Unfortunately, the penetration of the unstirred water layer and mucin into the GIT are the rate-limiting components. The generated chylomicrons are subsequently transported to the lymphatic system via mesenteric lymph and eventually reach the systemic circulation by lymphatic drainage through the thoracic duct [213]. Although lipolysis is considered as the principal mechanism governing the in vivo fate of LNPs, most lipolysis studies are based on in vitro models rather than in vivo models since identifying LNPs or lipolysates in the GIT is challenging [214]. Apart from the GIT, lipolysis can occur within the cells too, such as degradation of triglycerides of LNPs by lysosomal acid lipase following endocytosis [215]. The other mechanism regulating the fate of LNPs is the surface erosion due to hydrolysis or dissolution of the lipid matrix, particularly for fatty acid-based matrices that are not susceptible to lipolysis. The rate of erosion is normally gradual, and it decreases as the chain length of fatty acids increases. Consequently, the rate of medication release is usually slow. Several surfactants, like sodium dodecyl sulphate and bile salts, are employed to increase the rate of lipid matrix degradation, resulting in faster drug release. In general, surface erosion plays a little role in determining the fate of LNPs [216].
After the systemic injection of LNPs, protein corona comes into play, which starts to form a cover on the surface of LNPs. This protein corona is composed of two layers: a soft corona and a hard corona. During the initial stage, the soft corona layer is composed of low-affinity proteins with a high relative abundance that are in continual interchange with the biological media and LNPs surface starts depositing. Afterwards, in the later stages, low-affinity proteins are gradually replaced with proteins with a lower relative abundance but a greater surface affinity, allowing them to stay near the surface for longer. The creation of the protein corona significantly alters the characteristics of nanosystems, influencing their size, shape, and ultimate surface composition, thereby transforming them into a new biological identity. The inclusion of complement system proteins, also known as opsonins, occurs during the development of the protein corona. The complement system, which is a component of the innate immune system, aids in the identification of LNPs by the mononuclear phagocytic system, resulting in their increased clearance and a decrease in their systemic residence duration [217]. Apart from increased uptake by RES, the protein corona also affects the LNPs in terms of their deactivation and degradation as well as their capability to traverse the BBB [218].
Intravenously injected LNPs have the same fate as noncamouflaged particles, i.e. opsonin adsorption, RES recognition, and accumulation in RES organs such as the liver, spleen, lung, and kidney. The majority of LNPs that reach the liver are degraded and subsequently removed from circulation. PEGylation (coating of NLCs with PEG) prolongs circulation duration and prevents RES absorption, shifting LNPs to non-RES organs, including the brain [216]. Furthermore, PEGylation lowers transendothelial electrical resistance of cells and enhances paracellular transport of NLCs [213]. In a recent study by Fang et al., the authors reported that PEGylation of cysteine-functionalized docetaxel NLCs have doubled the circulation time of docetaxel (24 h) in comparison with the drug solution (12 h) as well as increased the drug plasma levels. The research team further reported that PEGylation inhibited opsonin from attaching to intact NLCs in systemic circulation, thus preventing their macrophage uptake [219].
Applications of nanostructured lipid carriers in the drug delivery to the brain tumours
NLC has a surprisingly wide variety of applications and is an important carrier for the delivery of food, medicines, and cosmetics. NLCs are used to administer pharmaceuticals through nasal, parenteral, ocular, pulmonary, topical, and transdermal routes. However, in this review, we are only focusing on the applications of NLCs in the targeting and treatment of brain tumours.
Several factors such as complexity of the brain structure, insufficient knowledge of the pathophysiology of oncogenesis, lack of accurate biomarkers to keep a check on whether the drug reaches its intended location in the brain, inefficient technology, and a dearth of validated animal models for preclinical studies make brain tumours a lethal malignancy. This is further complicated by BBB and blood–cerebrospinal fluid barrier because of the restricted drug penetration in the CNS and efflux of transported drugs from the brain to the blood circulation [220]. Several delivery mechanisms like disrupting the BBB, intracerebral delivery, use of prodrugs, carrier-mediated transport, receptor-mediated transport, etc., have been reported in the literature for the drug delivery to the brain [221]. However, nanocarriers give a considerable edge to existing BBB penetration methods.
NLCs are the suitable carriers for drug delivery to brain tissues as they can enhance the drug permeation through BBB by both active (through receptor and carrier transport) and passive diffusion (through paracellular and transcellular pathways). However, the transcellular mediated transport was reported to deliver only a limited number of lipophilic drugs [222]. Several studies also revealed that nanostructured lipid carriers can cross the blood–brain barrier by opening the tight junctions present between them and by transcytosis of NLCs through the endothelium layer [222]. Furthermore, the transcellular transport of the drugs across the BBB can be enhanced by coating the surface of NLCs with surfactant or permeation enhancer, which helps in dissolving the lipids present in brain capillary endothelial cells, thereby enhancing the drug delivery [222, 223]. Due to the easy functionalization of NLCs, their surface can be functionalized with peptides such as lactoferrin, transferrin, cell-penetrating peptides, and low-density lipoproteins, which aids the interaction between the lipid particles and receptors present at the blood–brain barrier, thus enhancing the drug penetration and transport in the brain [224]. In order to attain the therapeutic concentrations in the brain, the nanocarriers must be capable of regulating the efflux transporters along with the functionalization or coating of NLCs with specific polymers as the efflux mechanisms are the major roadblock in the drug delivery of cytotoxic drugs across BBB [222]. Figure 7 summarizes the various pathways through which the drug molecules can cross the BBB.
Physiological pathways through the BBB (The figure is reproduced from reference [225], an open access article under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0)
The intranasal route is another viable route recently explored for drug delivery to the brain. The significant advantage of this route is that the medication reaches directly the brain by circumventing the BBB through olfactory and trigeminal nerve pathways [226]. A high permeability, thin endothelium membrane, and high surface area which allow the passage of both small and large molecules make the nasal cavity ideal for drug delivery to the brain [227]. Thus, there has been a great deal of interest in nose-to-brain drug delivery. In addition, this route of drug administration is non-invasive, bypasses the first-pass metabolism, and reduces the exposure of the drug to other organs, which in turn minimizes the adverse effects [228]. Moreover, the drugs and enzymes that are not stable in the gastric fluids and degraded can be easily delivered to the brain via the intranasal route. Compared to the oral route, the nasal cavity's strong vascularization and neural network increase medication absorption and boost bioavailability in the brain [229]. All of the above-stated advantages provoked researchers to further study this route of drug delivery. Many researchers have utilized this pathway to deliver cytotoxic drugs across the BBB, which have been explained later.
In the following section, various research studies have been summarized in which the NLCs encapsulated with cytotoxic drugs have been used for drug delivery to the brain.
Curcumin, a well-known natural antioxidant and the anticancer compound obtained from Curcuma longa, is reported to exhibit its anti-proliferative effects by inducing the apoptotic pathway and by inhibiting several cell signalling pathways such as transcription factors, growth factors, apoptotic proteins, proliferative proteins, protein kinases, genes, and receptors [230, 231]. Despite its excellent medicinal properties, the efficacy of curcumin is restricted by its low bioavailability owing to its low water solubility, instability at basic pH, fast metabolism, and erratic absorption from the GIT [232]. All these factors made drug delivery of curcumin to the brain a challenging task; however, Chen et al. loaded curcumin into NLCs (Cur-NLCs) by hot HPH method for the treatment of brain cancer. The TEM studies had shown that Cur-NLCs had a mean particle size (MPS) of 214 nm and entrapment efficiency (EE) of 88.6%. In vitro cytotoxicity studies were performed on A172 cell lines (human brain cancer cell lines) using MTT assay. It was found that the inhibiting action of curcumin increases as the concentration of the drug increases and the inhibitory effect was found to be maximum (90%) at the concentration of 80 mg/mL. Furthermore, the findings showed a substantial increase in cellular reactive oxygen species (ROS) levels (2.6 times greater than control) which decreased cell viability by triggering A172 cell death. The Cur-NLCs were found to release the drug in a time-dependent manner, which is necessary for an effective anti-proliferative effect. The pharmacokinetics studies of Cur-NLCs were done in female mice having xenografts of human lung cancer. As per the findings, the half-life of curcumin was prolonged from 3.1 to 5.7 h, while the bioavailability was increased by 6.4 times. Moreover, the tumour volume was reduced by 82.3% by Cur-NLCs in a short time span (19 days). The study suggested the potential of NLCs in brain tumour therapy [233]. Likewise, Madane and Mahajan developed curcumin-loaded NLCs for the intranasal delivery to the brain. They fabricated the NLCs by hot HPH method using Precirol ATO5 and Capmul MCM as solid lipid and liquid lipid, respectively, tween 80 as a surfactant, soya lecithin as a stabilizer and mannitol as cryoprotectant. The MPS was reported to be 146.8 nm, while EE was found to be 90.86%. Curcumin was released in two phases from the NLCs, with burst release at the beginning and sustained release afterwards. The permeation and histopathological investigations were done on sheep nasal mucosa and reported that the curcumin loaded lipid nanoparticles permeated swiftly from the nasal mucosa to the brain (around 76.71% in 11 h) in contrast to the drug solution and exhibited no detrimental effects on the nasal mucosa, indicating that NLCs are relatively safe for intranasal drug delivery to the brain. MTT assay was used to assess the cytotoxic potential of Cur-NLCs on U373MG cell lines. NLCs were reported to possess higher antitumour efficacy than drug solution. This could be either due to the adherence of the nanoparticles onto the surface of tumour cells or their transportation into the cells, which releases the curcumin either near or inside the cancerous cells leading to a high local concentration of the drug and, thereby, high antitumour efficacy. Further, in vivo biodistribution investigations reported that curcumin delivery across BBB is significantly enhanced (Cmax = 86,201 ± 8182.1 ng/g at tmax of 2 h) by the use of lipid nanocarriers in contrast to the drug solution. This study explored a new non-invasive route of drug delivery to the brain which might lead to new directions in treating gliomas and glioblastomas [234].
Artemisinin, although is a potent anti-malarial agent, has also shown anticancer potential in solid tumours in various studies [235]. Emami et al. reported the synthesis of artemisinin-loaded NLCs (Art-NLCs), which were then functionalized with transferrin as a targeting ligand. The in vitro studies were done on U87MG cell lines (a type of brain cancer cell line with overexpression of transferrin receptors) employing MTT assay. The prepared NLCs were coated with transferrin to guide the NLCs to the tumour, thereby enhancing the permeation of the drug across BBB. The MPS, EE, and mean release time (MRT) of Art-NLCs were found to be 145 nm, 82.3% and 24 h, respectively. The in vitro cytotoxicity of transferrin-coated Art-NLCs was found to be significantly higher than Art-NLCs and artemisinin solution which is due to enhanced permeation of transferrin Art-NLCs across the brain through receptor-mediated transport. Furthermore, the aqueous solubility, site specificity, drug targeting, and permeation of the artemisinin were reported to be enhanced by encapsulating the drug into NLCs [236]. The same research group also have reported the synthesis of paclitaxel-loaded NLCs conjugated with transferrin by solvent evaporation technique. The pharmacokinetic attributes such as MPS, EE, and MRT of the formulation were observed to be 205.4 nm, 91.8%, and 29.32 h, respectively. The drug release pattern exhibited sustained release of the drug with around 77% release within the 3 days of administration. MTT assay was used to assess the in vitro cytotoxicity of blank NLCs, paclitaxel-loaded NLCs, paclitaxel-loaded NLCs conjugated with transferrin and Anzatax® (a marketed formulation of paclitaxel) on U87 brain cancer cell lines. Even at very high-test doses, blank NLCs showed no significant cytotoxicity on U87 cells. At concentrations less than 0.352 µM, no considerable differences were seen in the anti-proliferative activity of the marketed drug and transferrin-coated paclitaxel NLCs. However, when the concentration of paclitaxel in the NLCs was raised from 0.352 to 1.17 µM, drug-loaded NLCs conjugated with transferrin were found to be more effective. Although the in vitro studies look promising, in vivo investigations are necessary to comment on the efficacy and effectiveness of paclitaxel-loaded NLCs [237].
Sharma and his team employed NLCs for the treatment of meningeal leukaemia. They loaded cytarabine into lipid nanoparticles and further coated them with polysorbate 80 to enhance the drug permeation across BBB. Cytarabine, being highly hydrophilic, cannot cross the brain in the required concentrations; therefore, a very high dose is needed to treat meningeal leukaemia, which leads to severe side effects and cytotoxicity to normal cells. Therefore, a suitable carrier is needed which can enhance the transport of the drug across the BBB. In this study, the researchers formulated cytarabine-loaded NLCs using melt emulsification–ultrasonication and lyophilization, with an average size of 96.94 nm and an EE of 49.5%. In vitro drug release was around 89.90% with 15.8% release in the first hour showing an initial burst release followed by a slow sustained release for 3 days Furthermore, cell viability assay on EL4 cell lines showed higher activity of cytarabine NLCs with around 96–97% cytotoxicity at a concentration of 10 µM in 24 h. Also, no significant changes were reported after storing the formulation for 3 months [238].
In this sequence, to determine the potential of lipid nanoparticles to target a cytotoxic medication across BBB via intranasal route, Khan et al. synthesized a series of NLCs loaded with temozolomide by HPH method using Gelucire as solid lipid, vitamin E as liquid lipid, Transcutol and tween 80 in the ratio of 40:60 as surfactant and mannitol as cryoprotectant. The prepared nanoparticles were optimized using the Box–Behnken design. The optimized NLCs have a size of 131.58 nm with a drug release efficiency of 81.4%. The in vitro drug release studies indicate the prolonged release of temozolomide from the lipid nanoparticles over 24 h, whereas the temozolomide dispersion released 80% of the drug within the initial 8 h. Also, the permeation of NLCs to the brain through the intranasal route was found to be twice more than the drug solution. Concurrently, an increased temozolomide concentration was seen in the mouse brain in the case of drug-loaded NLCs administered via the intranasal route compared to intravenous administration. In a nutshell, on encapsulating temozolomide into NLCs, the brain targeting efficiency rose to 457% if the nanoparticles were given via the intranasal route [239]. Similarly, Qu et al. developed three different types of nanocarriers: polymeric nanoparticles, SLNs, and NLCs for the delivery of temozolomide to the brain. Solvent diffusion technique was used to develop temozolomide-loaded NLCs. U87 MG cells were used to test the drug's cytotoxicity in vitro, and its biodistribution and antitumour efficacy were evaluated in mice with malignant glioma. The particle size and EE of NLCs were reported to be 121.4 nm and 81.4%. Temozolomide-loaded NLCs exhibited a sustained release pattern, and the drug was released over 3 days. As per the cytotoxicity investigations, NLCs were found to be much more effective than the SLNs and polymeric nanoparticles. These results were confirmed by in vivo studies. The tumour growth was significantly inhibited on the administration of drug-loaded NLCs. On the whole, it was observed that NLCs were more effective than other carriers in the treatment of brain tumours [240]. Likewise, Song et al. used the solvent diffusion method to fabricate NLCs encapsulated with temozolomide, which was later functionalized using arginine–glycine–aspartic acid peptide (RGD). The prepared NLCs had an MPS of 118.3 nm and an EE of 84.7%. The RGD-modified NLCs exhibited a controlled release as per the in vitro studies and showed complete release of the drug after 24 h, while in the case of temozolomide-loaded NLCs, it was achieved in 36 h. In addition to this, higher cytotoxicity (10 times) was seen on U87MG cells in the case of RGD-functionalized NLCs compared to the aqueous solution of the drug. The in vivo investigation yielded similar findings, with RGD–temozolomide–NLC demonstrating higher tumour inhibition (83.3%) [241]. These studies profess the potential of NLCs as a novel therapeutic strategy for the treatment of gliomas.
Wu and his colleagues conducted another intriguing study to investigate the brain targeting effectiveness of NLCs. They formulated NLCs and SLNs loaded with two different drugs, temozolomide and vincristine, to assess their synergistic effect on glioma tumour cells and to compare the efficiency of SLNs and NLCs in delivering the drugs to the brain tissue. Both the carriers showed a similar EE of more than 85%, but NLCs had a smaller particle size (117.4 nm) in contrast to SLNs (180 nm). A sustained drug release was observed in both formulations, taking around 48 h to release both the drugs completely from NLCs. On the other hand, vincristine and temozolomide were almost completely released from SLNs after 24 and 36 h, respectively. Overall, the tumour inhibition efficiency of NLCs was higher than SLNs at any concentration. Further, NLCs carrying two drugs (vincristine and temozolomide) were reported to be 2.4 times more cytotoxic to U87MG tumour cells than temozolomide-loaded NLCs. A similar set of outcomes was obtained during the in vivo experiments. Over 80% of tumour development was reduced by temozolomide–vincristine NLCs, compared to 56% for SLNs and 70% for temozolomide-loaded NLCs [242]. On a similar note, Chen and his group prepared NLCs encapsulated with green fluorescence protein plasmid DNA and temozolomide using solvent diffusion technique. The prepared NLCs were 179 nm in size with gene loading and EE of 91% and 83%, respectively. Temozolomide–DNA–NLCs were reported to have four times higher in vitro antitumour activity in contrast to the drug solution. The in vivo studies showed similar results where the NLCs resulted in substantial suppression of cell proliferation (3.3 times higher efficiency than drug solution). According to the findings, temozolomide–DNA–NLCs significantly boosted brain targeting, anti-proliferative activity, and gene transfection efficacy without increasing toxicity [139]. Recently, Shirazi et al. fabricated SN38-loaded NLCs using cetyl palmitate, oleic acid, and polyvinyl alcohol as starting materials. SN38, chemically known as 7-ethyl-10-hydroxycamptothecin, is a metabolite of the anticancer drug irinotecan and is USFDA-approved for colorectal cancer [243]. Although it is a highly effective drug, its clinical use is limited due to its low aqueous solubility. To improve its water solubility and bioavailability, SN38 was encapsulated into NLCs and assessed on U87MG cells to demonstrate its efficacy on glioblastoma multiforme. Around 80% of the drug was released from the NLCs as indicated by the ex vivo drug release study. The drug was released in three phases with a burst release for the first hour, releasing about 30% of the entrapped drug. Following this, a slower and prolonged release was reported for up to 72 h in which 50% of the drug was released, and the remaining 10% of the drug was released constantly for up to 120 h. Regarding the cytotoxicity studies on the U87MG cell line, it was observed that at low concentration (0.01 µg/ml), SN38-loaded NLCs had no discernible cytotoxicity after 24 h of exposure. On the other hand, drug-loaded NLCs showed a substantial increase in cytotoxicity after 48 and 72 h and were found to be highly effective as compared to the free drug. This increase in cytotoxicity could be ascribed to the increased cellular uptake as visible in confocal microscopy [244].
Diet is an important part of living a healthy lifestyle. Natural components in our food, like flavonoids, can slow the growth of cancerous cells and prevent them from spreading further. Quercetin, a commonly found antioxidant in various fruits and vegetables, is reported to have an anticancer effect in addition to anti-inflammatory and anti-allergic activity. The exact mechanism of its cytotoxic activity on brain tumours is not clear; however, it is proposed that quercetin alters the JAK2/STAT3 signalling, decreases MMP‐2 expression, and induces cell death [245]. The poor aqueous solubility limits its use, and to overcome this problem, Patil and Mahajan prepared quercetin-loaded NLCs through the hot HPH technique. The nanoparticles had a mean size of 118.2 nm and an EE of 88.74%. A sustained drug release pattern was observed from NLCs encapsulated with quercetin. The findings from in vitro nasal permeability showed that quercetin diffused at a higher pace from the NLCs via the nasal cavity to the brain than the quercetin solution. A total of 76.71 ± 1.97% of the drug diffused from the NLCs into nasal mucosa after 6 h of the administration, which was threefold more than the amount of the drug diffused from the drug solution (26.73 ± 3.60%). The lipid particles were found to be safe and did not show any adverse effects on the nasal mucosa. The formulation showed the cytotoxicity of U373MG cells at 40 μg/ml. The drug distribution studies on the sheep demonstrated that a high concentration of quercetin was achieved in the case of NLCs (93.63 ± 19.88 μg/g) as compared to drug dispersion (42.26 ± 99.04 μg/g) after 90 min of administration. On the whole, when quercetin-loaded NLCs were administered intranasally, the drug was delivered directly to the CNS by bypassing the BBB, resulting in higher drug concentrations in the brain and enhanced CNS availability [246]. Kumar and his team undertook an amazing piece of work on nose-to-brain drug delivery. The group has reported the synthesis of resveratrol-loaded NLCs and chitosan-coated NLCs having MPS of 317.7 nm and EE of 77.42%. Resveratrol is a naturally occurring antioxidant found in berries, grapes, nuts, and wines. Besides its powerful antioxidant activity, resveratrol has been discovered to possess antitumour potential [247]. The formulation manifested a dual drug release pattern with a burst release initially followed by slow release over the prolonged period. Moreover, when compared to the uncoated formulation and drug solution, the chitosan-coated nanoparticles were reported with the highest cumulative permeation from sheep nasal mucosa possibly due to the interaction of chitosan with biological membranes, leading to weakened intercellular tight junctions and enhanced intracellular permeability to the brain. Although the studies provided good results, further in vivo and preclinical studies are required to comment on their therapeutic potential [248]. Carbone and his group conducted similar research on antioxidants for glioblastoma cancer therapy. The team studied the anti-proliferative effects of ferulic acid (FA)-loaded NLC on human glioblastoma cancer. The NLCs of different compositions were prepared by the phase inversion temperature method. The optimized NLC formulation (NLC O3) had the highest EE of 90.7% and showed slow prolonged release of the drug from the NLCs as compared to other formulations. In vitro cytotoxicity on U87MG cells using MTT assay showed that FA NLCs were most effective at a concentration of 36 µM [249]. This research work was carried forward by Grasso et al. and studied some cellular pathways responsible for the cytotoxic effect of FA-NLCs on U87MG cells. The prepared NLCs were in the range of 150–200 nm size and had a high EE of 90.5%. Furthermore, the NLCs loaded with FA were determined to reduce the levels of ERK1/2 kinases, c-Myc, and Bcl-2 proteins and studied its anti-proliferative effect. Indirect immunofluorescence was used to determine the influence of ferulic acid nanocarriers on the apoptotic cascade by measuring caspase-3 and PARP-1 cleavage. An increase in the activity of caspase-3 was noted in the presence of FA-NLCs. Additionally, significant levels of cleaved PARP-1 were detected in the cytosol and nucleus in U87MG cells upon exposure to NLCs, and all of the cells displayed apoptotic characteristics. Following the pro-apoptotic effects reported in this investigation, FA-NLCs appear to be an effective therapy for brain cancer [250]. In another study, Simão et al. have reported the synthesis of NLCs loaded with hesperetin. Hesperetin belongs to the flavanone class and has hypoglycaemic, cholesterol-lowering, antioxidant, anti-inflammatory, and anti-proliferative actions. However, due to its poor aqueous solubility and degradation by GIT enzymes and microbial flora, NLCs were fabricated to enhance bioavailability. The reported MPS and EE were below 80 nm and 72.7%, respectively. Moreover, the prepared lipid nanoparticles were found to be stable for a year at 25 °C. Using the dialysis bag diffusion method, in vitro drug release pattern was studied, and it was discovered that the drug was released in a sustained manner from the NLCs without any initial burst release. The cytotoxicity of free hesperetin and hesperetin-loaded NLC was tested on the T98G glioblastoma cell line using MTT assay. Overall, the drug-loaded NLCs were found to be more cytotoxic than the free drug at all concentrations. At a concentration of 33.08 and 36.39 µM, hesperetin-loaded NLCs exhibited a highly cytotoxic effect on T986G cells, reducing the cell viability to around 12.5%. Such outcomes stimulate future research into NLCs containing phytochemicals for their application in cancer treatment [251].
Various exciting studies that evaluated the possibility of NLCs as an effective carrier for delivering anticancer drugs to the brain are summarized in Table 3.
Clinical status of NLCs
The last two decades saw a slew of discoveries and innovations that offered up previously unimaginable possibilities to clinicians. One such discovery of lipid nanoparticles in the early 1990s has transformed the currently available therapies and diagnostics. Since then, drug delivery using NLCs has seen steadfast growth. NLCs have been widely used in the pharmaceutical and biomedical fields over the last decade owing to their extraordinary properties such as high drug loading capacity, enhanced stability, ability to target specific tissue, versatile drug release, and easy functionalization. As a result, they can be used for diagnosis, treatment, and control of various diseases such as pain, infections, allergic reactions, cardiovascular diseases, cancer, infections and more [257]. Despite the fact that NLCs have a lot of potential as drug carriers, preclinical and clinical research is still lacking. As a result, there is a need to broaden the scope of their applications to encompass clinical trials in accordance with suitable ethical laws [258]. A serious concern regarding the safety and biocompatibility of the lipid nanoparticles demands more research to precisely assess the safety margins and to successfully bring these carriers into the market [18]. Although a number of patents concerning lipid nanoparticles have been registered in the previous years, currently only NLCs-based cosmetics are available for the public (summarized in Table 4) [34, 259,260,261,262].
Future concerns and perspectives
There has been a steadfast growth in the study and development of NLCs and their heap of biomedical applications, particularly in targeting and treating several neurological disorders. NLCs have been considered as a smart drug delivery cargo and offer a multitudinous advantage such as high drug loading capacity, entrapment of both lipophilic and hydrophilic drugs, burst as well as prolonged drug release, physical and chemical stability, and enhanced permeation across the BBB. Even though NLCs made significant progress in the field of therapeutics and diagnostics, they are not still successful in making their way to preclinical and clinical studies. This might be due to a lack of rigorous investigation on the safety profile of NLCs as drug transporters. For example, because of its cytotoxic effects on normal cells, there is a need to further improve its therapeutic usage as an anticancer drug by more research on normal cells and animal models. Furthermore, additional research into the absorption, distribution, metabolism, and excretion of NLCs will help to confirm their promising properties. Besides, the potential of NLCs must be thoroughly explored at both the preclinical and clinical levels in order to land these carriers in the pharmaceutical market.
Conclusions
Nanostructured lipid carriers have proved to be a promising drug delivery vehicle for enhancing the drug permeation and transportation across the BBB. Having the benefits of other nanocarriers like liposomes, SLNs and by circumventing some of their drawbacks, NLCs have become a centre of attraction for scientists. NLCs as drug carriers offer a high drug loading capacity for drug distribution through a variety of routes, including parenteral, nasal, topical, ophthalmic, and pulmonary routes, while improving the physical and chemical stability of the medications, providing versatile release regulation, shielding them from degradation, and provide improved biopharmaceutical attributes. Because of their many advantages over first-generation systems, future NLC formulations have the potential to boost the lipid carrier system's prosperity. In this review, an outlook of the various research studies of drug-loaded NLCs in the treatment of brain tumours has been briefly discussed, indicating their valuable use in the field of therapeutics and theranostics. Indeed, many in vitro and in vivo studies have shown that NLCs could optimize the administration of anti-neoplastic drugs across the BBB, leading to enhanced safety profiles, effectiveness, and pharmacokinetic characteristics.
Availability of data and materials
Data and materials are available upon request. Figure 7 is reproduced from an open access article under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0) which permits use, sharing, adaptation, distribution, and reproduction in any medium or format, and appropriate credit to the original author(s) and the source is given. All the information in the manuscript has been referred from the included references.
Abbreviations
- ADME:
-
Absorption, distribution, metabolism, and excretion
- API:
-
Active pharmaceutical ingredient
- BBB:
-
Blood–brain barrier
- BTB:
-
Blood–tumour barrier
- CNS:
-
Central nervous system
- DNA:
-
Deoxyribonucleic acid
- EE:
-
Entrapment efficiency
- FA:
-
Ferulic acid
- GIT:
-
Gastrointestinal tract
- HLB:
-
Hydrophilic–lipophilic balance
- HME:
-
Hot melt extrusion
- HPH:
-
High-pressure homogenization
- LNPs:
-
Lipid nanoparticles
- MPS:
-
Mean particle size
- MTT:
-
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay
- NLCs:
-
Nanostructured lipid carriers
- o/w:
-
Oil/water
- PEG:
-
Polyethylene glycol
- RES:
-
Reticuloendothelial system
- RGD:
-
Arginine–glycine–aspartic acid peptide
- ROS:
-
Reactive oxygen species
- SCF:
-
Supercritical fluid
- SLNs:
-
Solid lipid nanoparticles
- TEM:
-
Transmission electron microscopy
References
Lapointe S, Perry A, Butowski NA (2018) Primary brain tumours in adults. Lancet 392:432–446. https://doi.org/10.1016/S0140-6736(18)30990-5
Weller M, Wick W, Aldape K et al (2015) Glioma. Nat Rev Dis Prim 1:15017. https://doi.org/10.1038/nrdp.2015.17
Tzeng SY, Green JJ (2013) Therapeutic nanomedicine for brain cancer. Ther Deliv 4:687–704. https://doi.org/10.4155/tde.13.38
Karathanasis E, Ghaghada KB (2016) Crossing the barrier: treatment of brain tumors using nanochain particles. Wiley Interdiscip Rev Nanomed Nanobiotechnol 8:678–695. https://doi.org/10.1002/WNAN.1387
Sahni JK, Doggui S, Ali J et al (2011) Neurotherapeutic applications of nanoparticles in Alzheimer’s disease. J Control Release 152:208–231. https://doi.org/10.1016/J.JCONREL.2010.11.033
Bhowmik A, Khan R, Ghosh MK (2015) Blood brain barrier: a challenge for effectual therapy of brain tumors. Biomed Res Int 2015:1–20. https://doi.org/10.1155/2015/320941
Neves AR, Queiroz JF, Weksler B et al (2015) Solid lipid nanoparticles as a vehicle for brain-targeted drug delivery: two new strategies of functionalization with apolipoprotein E. Nanotechnology 26:495103. https://doi.org/10.1088/0957-4484/26/49/495103
Abbott NJ, Patabendige AAK, Dolman DEM et al (2010) Structure and function of the blood–brain barrier. Neurobiol Dis 37:13–25. https://doi.org/10.1016/j.nbd.2009.07.030
Haumann R, Videira JC, Kaspers GJL et al (2020) Overview of current drug delivery methods across the blood-brain barrier for the treatment of primary brain tumors. CNS Drugs 34:1121–1131. https://doi.org/10.1007/s40263-020-00766-w
Ghadi R, Dand N (2017) BCS class IV drugs: highly notorious candidates for formulation development. J Control Release 248:71–95. https://doi.org/10.1016/J.JCONREL.2017.01.014
Dinda S, Pattnaik G (2013) Nanobiotechnology-based drug delivery in brain targeting. Curr Pharm Biotechnol 14:1264–1274. https://doi.org/10.2174/1389201015666140608143719
Amiri M, Jafari S, Kurd M et al (2021) Engineered solid lipid nanoparticles and nanostructured lipid carriers as new generations of blood–brain barrier transmitters. ACS Chem Neurosci 12:4475–4490. https://doi.org/10.1021/acschemneuro.1c00540
Fang C-L, Al-Suwayeh SA, Fang J-Y (2013) Nanostructured lipid carriers (NLCs) for drug delivery and targeting. Recent Pat Nanotechnol 7:41–55. https://doi.org/10.2174/187221013804484827
Akhavan S, Assadpour E, Katouzian I, Jafari SM (2018) Lipid nano scale cargos for the protection and delivery of food bioactive ingredients and nutraceuticals. Trends Food Sci Technol 74:132–146. https://doi.org/10.1016/j.tifs.2018.02.001
Weber S, Zimmer A, Pardeike J (2014) Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) for pulmonary application: a review of the state of the art. Eur J Pharm Biopharm 86:7–22. https://doi.org/10.1016/j.ejpb.2013.08.013
Mukherjee S, Ray S, Thakur R (2009) Solid lipid nanoparticles: a modern formulation approach in drug delivery system. Indian J Pharm Sci 71:349–358. https://doi.org/10.4103/0250-474X.57282
Chauhan I, Yasir M, Verma M, Singh AP (2020) Nanostructured lipid carriers: a groundbreaking approach for transdermal drug delivery. Adv Pharm Bull 10:150. https://doi.org/10.34172/APB.2020.021
Haider M, Abdin SM, Kamal L, Orive G (2020) Nanostructured lipid carriers for delivery of chemotherapeutics: a review. Pharmaceutics 12:288. https://doi.org/10.3390/pharmaceutics12030288
Bakthavachalam A, Remya PN, Damodharan N (2020) Review on solid lipid nanoparticles. Res J Pharm Technol 13:4434. https://doi.org/10.5958/0974-360X.2020.00783.0
Paliwal R, Paliwal SR, Kenwat R et al (2020) Solid lipid nanoparticles: a review on recent perspectives and patents. Expert Opin Ther Pat 30:179–194. https://doi.org/10.1080/13543776.2020.1720649
Duan Y, Dhar A, Patel C et al (2020) A brief review on solid lipid nanoparticles: part and parcel of contemporary drug delivery systems. RSC Adv 10:26777–26791. https://doi.org/10.1039/D0RA03491F
Muchow M, Maincent P, Müller RH (2008) lipid nanoparticles with a solid matrix (SLN®, NLC®, LDC®) for oral drug delivery. Drug Dev Ind Pharm 34:1394–1405. https://doi.org/10.1080/03639040802130061
Sarhadi S, Gholizadeh M, Moghadasian T, Golmohamadzadeh S (2020) Moisturizing effects of solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) using deionized and magnetized water by in vivo and in vitro methods. Iran J Basic Med Sci 23:337–343. https://doi.org/10.22038/IJBMS.2020.39587.9397
Jaiswal P, Gidwani B, Vyas A (2016) Nanostructured lipid carriers and their current application in targeted drug delivery. Artif Cells Nanomed Biotechnol 44:27–40. https://doi.org/10.3109/21691401.2014.909822
Hommoss A (2008) Nanostructured lipid carriers (NLC) in dermal and personal care formulations. Freie Universität
Vilella A, Tosi G, Grabrucker AM et al (2014) Insight on the fate of CNS-targeted nanoparticles. Part I: Rab5-dependent cell-specific uptake and distribution. J Control Release 174:195–201. https://doi.org/10.1016/j.jconrel.2013.11.023
Pardridge WM (2012) Drug transport across the blood–brain barrier. J Cereb Blood Flow Metab 32:1959–1972. https://doi.org/10.1038/jcbfm.2012.126
Fang M, Jin B et al (2012) In vitro characterization and in vivo evaluation of nanostructured lipid curcumin carriers for intragastric administration. Int J Nanomed 2012:5395. https://doi.org/10.2147/IJN.S36257
Yang S, Zhu J, Lu Y et al (1999) Body distribution of camptothecin solid lipid nanoparticles after oral administration. Pharm Res 16:751–757. https://doi.org/10.1023/A:1018888927852
Danhier F, Feron O, Préat V (2010) To exploit the tumor microenvironment: passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J Control Release 148:135–146. https://doi.org/10.1016/j.jconrel.2010.08.027
Tsai M-J, Wu P-C, Huang Y-B et al (2012) Baicalein loaded in tocol nanostructured lipid carriers (tocol NLCs) for enhanced stability and brain targeting. Int J Pharm 423:461–470. https://doi.org/10.1016/j.ijpharm.2011.12.009
Selvamuthukumar S, Velmurugan R (2012) Nanostructured lipid carriers: a potential drug carrier for cancer chemotherapy. Lipids Health Dis 11:1–8. https://doi.org/10.1186/1476-511X-11-159
Dhiman N, Awasthi R, Sharma B et al (2021) Lipid nanoparticles as carriers for bioactive delivery. Front Chem 9:268. https://doi.org/10.3389/FCHEM.2021.580118
Battaglia L, Ugazio E (2019) Lipid nano- and microparticles: an overview of patent-related research. J Nanomater 2019:1–22. https://doi.org/10.1155/2019/2834941
Shah R, Eldridge D, Palombo E, Harding I (2015) Composition and Structure. Lipid nanoparticles: production, characterization and stability, 1st edn. Springer, pp 11–22
Sharma A, Baldi A (2018) Nanostructured lipid carriers: a review. J Dev Drugs. https://doi.org/10.4172/2329-6631.1000191
Faheim S, Gardouh A, Nouh A, Ghorab M (2018) Review article on nanoemulsions and nanostructured lipid carriers. Rec Pharm Biomed Sci 2:23–31. https://doi.org/10.21608/rpbs.2018.5223.1011
Poonia N, Kharb R, Lather V, Pandita D (2016) Nanostructured lipid carriers: versatile oral delivery vehicle. Futur Sci OA 2:FSO35. https://doi.org/10.4155/fsoa-2016-0030
Muchow M, Maincent P, Müller RH, Keck CM (2011) Production and characterization of testosterone undecanoate-loaded NLC for oral bioavailability enhancement. Drug Dev Ind Pharm 37:8–14. https://doi.org/10.3109/03639045.2010.489559
Noor NM, Sheikh K, Somavarapu S, Taylor KMG (2017) Preparation and characterization of dutasteride-loaded nanostructured lipid carriers coated with stearic acid-chitosan oligomer for topical delivery. Eur J Pharm Biopharm 117:372–384. https://doi.org/10.1016/J.EJPB.2017.04.012
Subramaniam B, Siddik ZH, Nagoor NH (2020) Optimization of nanostructured lipid carriers: understanding the types, designs, and parameters in the process of formulations. J Nanoparticle Res 22:1–29. https://doi.org/10.1007/S11051-020-04848-0
Tamjidi F, Shahedi M, Varshosaz J, Nasirpour A (2013) Nanostructured lipid carriers (NLC): a potential delivery system for bioactive food molecules. Innov Food Sci Emerg Technol 19:29–43. https://doi.org/10.1016/J.IFSET.2013.03.002
Naseri N, Valizadeh H, Zakeri-Milani P (2015) Solid lipid nanoparticles and nanostructured lipid carriers: structure, preparation and application. Adv Pharm Bull 5:305–313. https://doi.org/10.15171/APB.2015.043
Kaur S, Nautyal U, Singh R et al (2015) Nanostructure lipid carrier (NLC): the new generation of lipid nanoparticles. Asian Pac J Health Sci 2:76–93. https://doi.org/10.21276/apjhs.2015.2.2.14
Fang C-L, Al-Suwayeh AS, Fang J-Y (2012) Nanostructured lipid carriers (NLCs) for drug delivery and targeting. Recent Pat Nanotechnol 7:41–55. https://doi.org/10.2174/1872210511307010041
Rajalakshmi G, Dhanapal CK, Sundhararajan R (2020) an insight to nanostructured lipid carrier system. J Drug Deliv Ther 10:173–182. https://doi.org/10.22270/JDDT.V10I6-S.4589
Czajkowska-Kośnik A, Szekalska M, Winnicka K (2019) Nanostructured lipid carriers: a potential use for skin drug delivery systems. Pharmacol Reports 71:156–166. https://doi.org/10.1016/J.PHAREP.2018.10.008
Montenegro L, Lai F, Offerta A et al (2016) From nanoemulsions to nanostructured lipid carriers: a relevant development in dermal delivery of drugs and cosmetics. J Drug Deliv Sci Technol 32:100–112. https://doi.org/10.1016/J.JDDST.2015.10.003
Arunkumar N, Deecaraman M, Rani C (2014) Nanosuspension technology and its applications in drug delivery. Asian J Pharm 3:168–173. https://doi.org/10.22377/AJP.V3I3.261
Wen J, Chen G, Chen S (2018) Nanostructured lipid carriers. In: Roohinejad S, Greiner R, Oey I, Wen J (eds) Emulsion-based systems for delivery of food active compounds: formation, application, health and safety. Wiley, Hoboken, pp 139–159
Severino P, Andreani T, Macedo AS et al (2012) Current state-of-art and new trends on lipid nanoparticles (SLN and NLC) for oral drug delivery. J Drug Deliv 2012:1–10. https://doi.org/10.1155/2012/750891
Beloqui A, Solinís MÁ, Rodríguez-Gascón A et al (2016) Nanostructured lipid carriers: promising drug delivery systems for future clinics. Nanomed Nanotechnol Biol Med 12:143–161. https://doi.org/10.1016/J.NANO.2015.09.004
Souto EB, Baldim I, Oliveira WP et al (2020) SLN and NLC for topical, dermal, and transdermal drug delivery. Expert Opin Drug Deliv 17:357–377. https://doi.org/10.1080/17425247.2020.1727883
Iqbal MA, Md S, Sahni JK et al (2012) Nanostructured lipid carriers system: recent advances in drug delivery. J Drug Target 20:813–830. https://doi.org/10.3109/1061186X.2012.716845
Samimi S, Maghsoudnia N, Eftekhari RB, Dorkoosh F (2019) Lipid-based nanoparticles for drug delivery systems. In: Mohapatra SS, Ranjan S, Dasgupta N et al (eds) Characterization and biology of nanomaterials for drug delivery: nanoscience and nanotechnology in drug delivery. Elsevier, pp 47–76
Salvi VR, Pawar P (2019) Nanostructured lipid carriers (NLC) system: a novel drug targeting carrier. J Drug Deliv Sci Technol 51:255–267. https://doi.org/10.1016/J.JDDST.2019.02.017
Ganesan P, Narayanasamy D (2017) Lipid nanoparticles: Different preparation techniques, characterization, hurdles, and strategies for the production of solid lipid nanoparticles and nanostructured lipid carriers for oral drug delivery. Sustain Chem Pharm 6:37–56. https://doi.org/10.1016/J.SCP.2017.07.002
Jain P, Rahi P, Pandey V et al (2017) Nanostructure lipid carriers: a modish contrivance to overcome the ultraviolet effects. Egypt J Basic Appl Sci 4:89–100. https://doi.org/10.1016/J.EJBAS.2017.02.001
Lammari N, Tarhini M, Miladi K et al (2021) Encapsulation methods of active molecules for drug delivery. In: Chappel E (ed) Drug delivery devices and therapeutic systems. Academic Press, pp 289–306
Garud A, Singh D, Garud N (2012) Solid lipid nanoparticles (SLN): method, characterization and applications. Int Curr Pharm J 1:384–393. https://doi.org/10.3329/ICPJ.V1I11.12065
Sastri KT, Radha GV, Pidikiti S, Vajjhala P (2020) Solid lipid nanoparticles: preparation techniques, their characterization, and an update on recent studies. J Appl Pharm Sci 10:126–141. https://doi.org/10.7324/JAPS.2020.10617
Qushawy M, Nasr A (2019) Solid lipid nanoparticles (SLNs) as nano drug delivery carriers: preparation, characterization and application. Int J Appl Pharm 12:1–9. https://doi.org/10.22159/ijap.2020v12i1.35312
Khosa A, Reddi S, Saha RN (2018) Nanostructured lipid carriers for site-specific drug delivery. Biomed Pharmacother 103:598–613. https://doi.org/10.1016/J.BIOPHA.2018.04.055
Shah MR, Imran M, Ullah S (2017) Solid lipid nanoparticles. Lipid-based nanocarriers for drug delivery and diagnosis. William Andrew Publishing, pp 1–35
Mehnert W, Mäder K (2012) Solid lipid nanoparticles: production, characterization and applications. Adv Drug Deliv Rev 64:83–101. https://doi.org/10.1016/J.ADDR.2012.09.021
Kumar R (2019) Lipid-based nanoparticles for drug-delivery systems. In: Mohapatra SS, Ranjan S, Dasgupta N et al (eds) Nanocarriers for drug delivery. Elsevier, pp 249–284
Svilenov H, Tzachev C (2014) Solid lipid nanoparticles-a promising drug delivery system. In: Seifalian A, de Mel A, Kalaskar DM (eds) Nanomedicine. One Central Press, pp 187–237
Schubert MA, Müller-Goymann CC (2003) Solvent injection as a new approach for manufacturing lipid nanoparticles—evaluation of the method and process parameters. Eur J Pharm Biopharm 55:125–131. https://doi.org/10.1016/S0939-6411(02)00130-3
Amandeep BS, Kumar M et al (2020) Recent advances in the development of the nanostructured lipid carriers for the topical fungal infections. J Reports Pharm Sci 9:271. https://doi.org/10.4103/jrptps.JRPTPS_99_19
Bornare AS, Saudagar RB (2017) Nanostructured lipid carrier (NLC): a modern approach for transdermal drug delivery. Res J Pharm Technol 10:2784–2792. https://doi.org/10.5958/0974-360X.2017.00493.0
Kotmakçı M, Akbaba H, Erel G et al (2016) Improved method for solid lipid nanoparticle preparation based on hot microemulsions: preparation, characterization, cytotoxicity, and hemocompatibility evaluation. AAPS PharmSciTech 18:1355–1365. https://doi.org/10.1208/S12249-016-0606-Z
Xia Q, Hao X, Lu Y et al (2008) Production of drug-loaded lipid nanoparticles based on phase behaviors of special hot microemulsions. Colloids Surfaces A Physicochem Eng Asp 313–314:27–30. https://doi.org/10.1016/J.COLSURFA.2007.04.067
Hanumanaik M, Patel SK, Sree KR (2013) Solid lipid nanoparticles; a review. Int J Pharm Sci Res 4:928–940. https://doi.org/10.13040/IJPSR.0975-8232.4(3).928-40
Surender V, Deepika M (2016) Solid lipid nanoparticles: a comprehensive review. J Chem Pharm Res 8:102–114
Iqbal M, Zafar N, Fessi H, Elaissari A (2015) Double emulsion solvent evaporation techniques used for drug encapsulation. Int J Pharm 496:173–190. https://doi.org/10.1016/J.IJPHARM.2015.10.057
Kanojia N, Sharma N, Gupta N, Singh S (2021) Applications of nanostructured lipid carriers: recent advancements and patent review. Biointerface Res Appl Chem 12:638–652. https://doi.org/10.33263/BRIAC121.638652
Rawal SU, Patel MM (2018) Lipid nanoparticulate systems: modern versatile drug carriers. In: Grumezescu AM (ed) Lipid nanocarriers for drug targeting. William Andrew Publishing, pp 49–138
Li Q, Cai T, Huang Y et al (2017) A review of the structure, preparation, and application of NLCs, PNPs, and PLNs. Nanomaterials 7:122. https://doi.org/10.3390/nano7060122
Reddy SH, Umashankar MS, Damodharan N (2018) Formulation, characterization and applications on solid lipid nanoparticles—a review. Res J Pharm Technol 11:5691–5700. https://doi.org/10.5958/0974-360X.2018.01031.4
Das S, Chaudhury A (2011) Recent advances in lipid nanoparticle formulations with solid matrix for oral drug delivery. AAPS PharmSciTech 12:62–76. https://doi.org/10.1208/S12249-010-9563-0
Hua X, Xu S, Wang M et al (2017) Effects of high-speed homogenization and high-pressure homogenization on structure of tomato residue fibers. Food Chem 232:443–449. https://doi.org/10.1016/J.FOODCHEM.2017.04.003
Puglia C, Bonina F (2012) Lipid nanoparticles as novel delivery systems for cosmetics and dermal pharmaceuticals. Expert Opin Drug Deliv 9:429–441. https://doi.org/10.1517/17425247.2012.666967
Anton N, Benoit JP, Saulnier P (2008) Design and production of nanoparticles formulated from nano-emulsion templates—a review. J Control Release 128:185–199. https://doi.org/10.1016/J.JCONREL.2008.02.007
Ren G, Sun Z, Wang Z et al (2019) Nanoemulsion formation by the phase inversion temperature method using polyoxypropylene surfactants. J Colloid Interface Sci 540:177–184. https://doi.org/10.1016/J.JCIS.2019.01.018
Jintapattanakit A (2018) Preparation of nanoemulsions by phase inversion temperature (PIT) method. Pharm Sci Asia 45:1–12. https://doi.org/10.29090/PSA.2018.01.001
Duong V-A, Nguyen T-T-L, Maeng H-J (2020) Preparation of solid lipid nanoparticles and nanostructured lipid carriers for drug delivery and the effects of preparation parameters of solvent injection method. Molecules 25:4781. https://doi.org/10.3390/MOLECULES25204781
Patil D, Pattewar S, Palival S et al (2019) Nanostructured lipid carriers: A platform to lipophilic drug for oral bioavailability enhancement. J Drug Deliv Ther 9:758–764. https://doi.org/10.22270/JDDT.V9I3-S.2750
Corrias F, Lai F (2011) New methods for lipid nanoparticles preparation. Recent Pat Drug Deliv Formul 5:201–213. https://doi.org/10.2174/187221111797200597
Friberg SE, Corkery RW, Blute IA (2011) Phase inversion temperature (PIT) emulsification process. J Chem Eng Data 56:4282–4290. https://doi.org/10.1021/JE101179S
Mahant S, Rao R, Nanda S (2018) Nanostructured lipid carriers: Revolutionizing skin care and topical therapeutics. Design of nanostructures for versatile therapeutic applications. William Andrew Publishing, pp 97–136
Shidhaye S, Vaidya R, Sutar S et al (2008) Solid lipid nanoparticles and nanostructured lipid carriers—innovative generations of solid lipid carriers. Curr Drug Deliv 5:324–331. https://doi.org/10.2174/156720108785915087
Harde H, Das M, Jain S (2011) Solid lipid nanoparticles: an oral bioavailability enhancer vehicle. Expert Opin Drug Deliv 8:1407–1424. https://doi.org/10.1517/17425247.2011.604311
Chakravarty P, Famili A, Nagapudi K, Al-Sayah MA (2019) Using Supercritical fluid technology as a green alternative during the preparation of drug delivery systems. Pharmaceutics 11:629. https://doi.org/10.3390/PHARMACEUTICS11120629
Meziani MJ, Pathak P, Sun Y-P (2009) Supercritical fluid technology for nanotechnology in drug delivery. In: de Villiers MM, Aramwit P, Kwon GS (eds) Nanotechnology in drug delivery. Biotechnology: pharmaceutical aspects. Springer, New York, pp 69–104
Carneiro SP, dos Santos ODH (2020) Nanostructured lipid carrier-based drug delivery systems for tuberculosis treatment. In: Kesharwani P (ed) Nanotechnology based approaches for tuberculosis treatment. Academic Press, pp 193–205
Chattopadhyay P, Shekunov BY, Yim D et al (2007) Production of solid lipid nanoparticle suspensions using supercritical fluid extraction of emulsions (SFEE) for pulmonary delivery using the AERx system. Adv Drug Deliv Rev 59:444–453. https://doi.org/10.1016/J.ADDR.2007.04.010
Akbari Z, Amanlou M, Karimi-Sabet J et al (2020) Application of supercritical fluid technology for preparation of drug loaded solid lipid nanoparticles. Int J Nanosci Nanotechnol 16:13–33
Maniruzzaman M, Boateng JS, Snowden MJ, Douroumis D (2012) A Review of hot-melt extrusion: process technology to pharmaceutical products. ISRN Pharm 2012:1–9. https://doi.org/10.5402/2012/436763
Adler C (2017) New lipid-based formulation approaches and characterization tools for hot-melt extrusion. University of Basel
Bhagurkar AM, Repka MA, Murthy SN (2017) A novel approach for the development of a nanostructured lipid carrier formulation by hot-melt extrusion technology. J Pharm Sci 106:1085–1091. https://doi.org/10.1016/j.xphs.2016.12.015
Crowley MM, Zhang F, Repka MA et al (2007) Pharmaceutical applications of hot-melt extrusion: part I. Drug Dev Ind Pharm 33:909–926. https://doi.org/10.1080/03639040701498759
Patil H, Tiwari RV, Repka MA (2016) Hot-melt extrusion: from theory to application in pharmaceutical formulation. AAPS PharmSciTech 17:20–42. https://doi.org/10.1208/s12249-015-0360-7
Brito Raj S, Chandrasekhar KB, Reddy KB (2019) Formulation, in-vitro and in-vivo pharmacokinetic evaluation of simvastatin nanostructured lipid carrier loaded transdermal drug delivery system. Futur J Pharm Sci 5:1–14. https://doi.org/10.1186/S43094-019-0008-7
Youssef A, Dudhipala N, Majumdar S (2020) Ciprofloxacin loaded nanostructured lipid carriers incorporated into in-situ gels to improve management of bacterial endophthalmitis. Pharmaceutics 12:572. https://doi.org/10.3390/PHARMACEUTICS12060572
Avasatthi V, Pawar H, Dora CP et al (2015) A novel nanogel formulation of methotrexate for topical treatment of psoriasis: optimization, in vitro and in vivo evaluation. Pharm Dev Technol 21:554–562. https://doi.org/10.3109/10837450.2015.1026605
Mohammadi M, Pezeshki A, Abbasi MM et al (2017) Vitamin D3-loaded nanostructured lipid carriers as a potential approach for fortifying food beverages; in vitro and in vivo evaluation. Adv Pharm Bull 7:61. https://doi.org/10.15171/APB.2017.008
Seabra CL, Nunes C, Brás M et al (2018) Lipid nanoparticles to counteract gastric infection without affecting gut microbiota. Eur J Pharm Biopharm 127:378–386. https://doi.org/10.1016/J.EJPB.2018.02.030
Hajipour H, Hamishehkar H, Nazari Soltan Ahmad S et al (2018) Improved anticancer effects of epigallocatechin gallate using RGD-containing nanostructured lipid carriers. Artif Cells Nanomed Biotechnol 46:283–292. https://doi.org/10.1080/21691401.2017.1423493
Bashiri S, Ghanbarzadeh B, Ayaseh A et al (2020) Preparation and characterization of chitosan-coated nanostructured lipid carriers (CH-NLC) containing cinnamon essential oil for enriching milk and anti-oxidant activity. LWT 119:108836. https://doi.org/10.1016/j.lwt.2019.108836
EhSuk VR, Latif MF, Teo YY, Misran M (2020) Development of nanostructured lipid carrier (NLC) assisted with polysorbate nonionic surfactants as a carrier for l-ascorbic acid and Gold Tri.E 30. J Food Sci Technol 57:3259–3266. https://doi.org/10.1007/S13197-020-04357-X
Tirumalesh C, Suram D, Dudhipala N, Banala N (2020) Enhanced pharmacokinetic activity of zotepine via nanostructured lipid carrier system in Wistar rats for oral application. Pharm Nanotechnol 8:148–160. https://doi.org/10.2174/2211738508666200225113359
Cao C, Wang Q, Liu Y (2019) Lung cancer combination therapy: doxorubicin and β-elemene co-loaded, pH-sensitive nanostructured lipid carriers. Drug Des Devel Ther 13:1087. https://doi.org/10.2147/DDDT.S198003
Ameeduzzafar QM, Alruwaili NK et al (2020) BBD-based development of itraconazole loaded nanostructured lipid carrier for topical delivery. in vitro evaluation and antimicrobial assessment. J Pharm Innov 16:85–98. https://doi.org/10.1007/S12247-019-09420-5
Patwekar SL, Pedewad SR, Gattani S (2017) Development and evaluation of nanostructured lipid carriers-based gel of isotretinoin. Part Sci Technol 36:832–843. https://doi.org/10.1080/02726351.2017.1305026
Bahrami MA, Farhadian N (2019) Experimental study and mathematical modeling for encapsulation of fentanyl citrate drug in nanostructured lipid carrier. J Biomol Struct Dyn 38:1263–1271. https://doi.org/10.1080/07391102.2019.1599732
Bahrami MA, Farhadian N, Karimi M et al (2020) Improvement of pain relief of fentanyl citrate drug encapsulated in nanostructured lipid carrier: drug formulation, parameter optimization, in vitro and in vivo studies. Drug Des Devel Ther 14:2033–2045. https://doi.org/10.2147/DDDT.S235474
Gujjar S, Madhavi BLR, Karki R (2019) Formulation and evaluation of topical gel containing nanostructured lipid carriers dispersion of an antifungal drug. Acta Pharm Sci 57:57–75. https://doi.org/10.23893/1307-2080.APS.05724
Karmakar G, Nahak P, Guha P et al (2018) Role of PEG 2000 in the surface modification and physicochemical characteristics of pyrazinamide loaded nanostructured lipid carriers. J Chem Sci 130:42. https://doi.org/10.1007/s12039-018-1448-x
Esposito E, Sguizzato M, Drechsler M et al (2017) Progesterone lipid nanoparticles: scaling up and in vivo human study. Eur J Pharm Biopharm 119:437–446. https://doi.org/10.1016/j.ejpb.2017.07.015
Noori Siahdasht F, Farhadian N, Karimi M, Hafizi L (2020) Enhanced delivery of melatonin loaded nanostructured lipid carriers during in vitro fertilization: NLC formulation, optimization and IVF efficacy. RSC Adv 10:9462–9475. https://doi.org/10.1039/C9RA10867J
Sathe P, Saka R, Kommineni N et al (2019) Dithranol-loaded nanostructured lipid carrier-based gel ameliorate psoriasis in imiquimod-induced mice psoriatic plaque model. Drug Dev Ind Pharm 45:826–838. https://doi.org/10.1080/03639045.2019.1576722
Noh GY, Suh JY, Park SN (2017) Ceramide-based nanostructured lipid carriers for transdermal delivery of isoliquiritigenin: development, physicochemical characterization, and in vitro skin permeation studies. Korean J Chem Eng 34:400–406. https://doi.org/10.1007/s11814-016-0267-3
Duong VA, Nguyen TTL, Maeng HJ, Chi SC (2019) Nanostructured lipid carriers containing ondansetron hydrochloride by cold high-pressure homogenization method: preparation, characterization, and pharmacokinetic evaluation. J Drug Deliv Sci Technol 53:101185. https://doi.org/10.1016/J.JDDST.2019.101185
Zadeh BSM, Niro H, Rahim F, Esfahani G (2018) Ocular delivery system for propranolol hydrochloride based on nanostructured lipid carrier. Sci Pharm 86:16. https://doi.org/10.3390/SCIPHARM86020016
Madan JR, Khobaragade S, Dua K, Awasthi R (2020) Formulation, optimization, and in vitro evaluation of nanostructured lipid carriers for topical delivery of Apremilast. Dermatol Ther 33:e13370. https://doi.org/10.1111/DTH.13370
Raj SB, Chandrasekhar K, Reddy K (2017) Design, development and invivo pharmacokinetic evaluation of cardiovascular drug loaded nano structured lipid carrier system. Int J Drug Deliv Technol 7:190–209. https://doi.org/10.25258/IJDDT.V7I03.9563
Amer RI, Yassin GE, Mohamed RA, Fayez AM (2021) Pharmaceutical and pharmacological evaluation of the effect of nano-formulated spironolactone and progesterone on inflammation and hormonal levels for managing hirsutism experimentally induced in rats. AAPS PharmSciTech 22:1–11. https://doi.org/10.1208/S12249-021-02003-Z
Abdolahpour S, Mahdieh N, Jamali Z et al (2017) Development of doxorubicin-loaded nanostructured lipid carriers: preparation, characterization, and in vitro evaluation on MCF-7 cell line. Bionanoscience 7:32–39. https://doi.org/10.1007/S12668-016-0391-X
Abdolahpour S, Toliyat T, Omidfar K et al (2017) Targeted delivery of doxorubicin into tumor cells by nanostructured lipid carriers conjugated to anti-EGFRvIII monoclonal antibody. Artif Cells Nanomed Biotechnol 46:89–94. https://doi.org/10.1080/21691401.2017.1296847
Khan S, Shaharyar M, Fazil M et al (2016) Tacrolimus-loaded nanostructured lipid carriers for oral delivery—optimization of production and characterization. Eur J Pharm Biopharm 108:277–288. https://doi.org/10.1016/J.EJPB.2016.07.017
Karakash I, Vasileska J, Shalabalija D et al (2020) Freeze-drying of nanostructured lipid carriers loaded with Salvia off. Extract for Alzheimer’s disease treatment. Maced Pharm Bull 66:219–220. https://doi.org/10.33320/maced.pharm.bull.2020.66.03.109
Lee SG, Kim CH, Sung SW et al (2018) RIPL peptide-conjugated nanostructured lipid carriers for enhanced intracellular drug delivery to hepsin-expressing cancer cells. Int J Nanomedicine 13:3263–3278. https://doi.org/10.2147/IJN.S166021
Kim CH, Kang TH, Kim BD et al (2020) Enhanced docetaxel delivery using sterically stabilized RIPL peptide-conjugated nanostructured lipid carriers: In vitro and in vivo antitumor efficacy against SKOV3 ovarian cancer cells. Int J Pharm 583:119393. https://doi.org/10.1016/J.IJPHARM.2020.119393
Gao X, Zhang J, Xu Q et al (2017) Hyaluronic acid-coated cationic nanostructured lipid carriers for oral vincristine sulfate delivery. Drug Dev Ind Pharm 43:661–667. https://doi.org/10.1080/03639045.2016.1275671
Anand A, Singh G, Saraf SA (2018) Plackett-Burman design as a tool for screening and process optimization of rivastigmine-loaded lipid nanocarriers. Asian J Pharm Clin Res 11:155–158. https://doi.org/10.22159/AJPCR.2018.V11I12.28066
Anand A, Arya M, Singh G et al (2017) Design and development of resveratrol NLCs and their role in synaptic transmission of acetylcholine in C. elegans model. Curr Drug ther 12:134–148. https://doi.org/10.2174/1574885512666170529114325
Abd El-Halim SM, Abdelbary GA, Amin MM et al (2020) Stabilized oral nanostructured lipid carriers of Adefovir Dipivoxil as a potential liver targeting: estimation of liver function panel and uptake following intravenous injection of radioiodinated indicator. DARU J Pharm Sci 28:517–532. https://doi.org/10.1007/S40199-020-00355-8
Ghasemiyeh P, Azadi A, Daneshamouz S et al (2019) Cyproterone acetate-loaded nanostructured lipid carriers: effect of particle size on skin penetration and follicular targeting. Pharm Dev Technol 24:812–823. https://doi.org/10.1080/10837450.2019.1596133
Chen Z, Lai X, Song S et al (2015) Nanostructured lipid carriers based temozolomide and gene co-encapsulated nanomedicine for gliomatosis cerebri combination therapy. Drug Deliv 23:1369–1373. https://doi.org/10.3109/10717544.2015.1038857
Jawahar N, Hingarh PK, Radhakrishnan A et al (2018) Enhanced oral bioavailability of an antipsychotic drug through nanostructured lipid carriers. Int J Biol Macromol 110:269–275. https://doi.org/10.1016/J.IJBIOMAC.2018.01.121
Jiang H, Geng D, Liu H et al (2016) Co-delivery of etoposide and curcumin by lipid nanoparticulate drug delivery system for the treatment of gastric tumors. Drug Deliv 23:3665–3673. https://doi.org/10.1080/10717544.2016.1217954
Eleraky NE, Omar MM, Mahmoud HA, Abou-Taleb HA (2020) Nanostructured lipid carriers to mediate brain delivery of temazepam: design and in vivo study. Pharmaceutics 12:451. https://doi.org/10.3390/PHARMACEUTICS12050451
Duong V-A, Nguyen T-T-L, Maeng H-J, Chi S-C (2019) Preparation of ondansetron hydrochloride-loaded nanostructured lipid carriers using solvent injection method for enhancement of pharmacokinetic properties. Pharm Res 36:1–12. https://doi.org/10.1007/S11095-019-2672-X
Poonia N, Narang JK, Lather V et al (2019) Resveratrol loaded functionalized nanostructured lipid carriers for breast cancer targeting: systematic development, characterization and pharmacokinetic evaluation. Colloids Surfaces B Biointerfaces 181:756–766. https://doi.org/10.1016/J.COLSURFB.2019.06.004
Abd El-Hamid BN, Swarnakar NK, Soliman GM et al (2018) High payload nanostructured lipid carriers fabricated with alendronate/polyethyleneimine ion complexes. Int J Pharm 535:148–156. https://doi.org/10.1016/J.IJPHARM.2017.10.064
Wavikar P, Pai R, Vavia P (2017) Nose to brain delivery of rivastigmine by in situ gelling cationic nanostructured lipid carriers: enhanced brain distribution and pharmacodynamics. J Pharm Sci 106:3613–3622. https://doi.org/10.1016/J.XPHS.2017.08.024
Zhang S, Lu C, Zhang X et al (2016) Targeted delivery of etoposide to cancer cells by folate-modified nanostructured lipid drug delivery system. Drug Deliv 23:1838–1845. https://doi.org/10.3109/10717544.2016.1141258
Garg NK, Sharma G, Singh B et al (2017) Quality by Design (QbD)-enabled development of aceclofenac loaded-nano structured lipid carriers (NLCs): an improved dermatokinetic profile for inflammatory disorder(s). Int J Pharm 517:413–431. https://doi.org/10.1016/J.IJPHARM.2016.12.010
Beg S, Saini S, Bandopadhyay S et al (2017) QbD-driven development and evaluation of nanostructured lipid carriers (NLCs) of Olmesartan medoxomil employing multivariate statistical techniques. Drug Dev Ind Pharm 44:407–420. https://doi.org/10.1080/03639045.2017.1395459
Andrade LM, Rocha KAD, De Sá FAP et al (2016) Voriconazole-loaded nanostructured lipid carriers for ocular drug delivery. Cornea 35:866–871. https://doi.org/10.1097/ICO.0000000000000825
Pradhan M, Singh D, Singh MR (2017) Fabrication, optimization and characterization of Triamcinolone acetonide loaded nanostructured lipid carriers for topical treatment of psoriasis: application of Box Behnken design, in vitro and ex vivo studies. J Drug Deliv Sci Technol 41:325–333. https://doi.org/10.1016/J.JDDST.2017.07.024
Yu G, Ali Z, Khan AS et al (2021) Preparation, pharmacokinetics, and antitumor potential of miltefosine-loaded nanostructured lipid carriers. Int J Nanomedicine 16:3255. https://doi.org/10.2147/IJN.S299443
Sadati Behbahani E, Ghaedi M, Abbaspour M et al (2019) Curcumin loaded nanostructured lipid carriers: in vitro digestion and release studies. Polyhedron 164:113–122. https://doi.org/10.1016/J.POLY.2019.02.002
Tran TH, Chu DT, Truong DH et al (2016) Development of lipid nanoparticles for a histone deacetylases inhibitor as a promising anticancer therapeutic. Drug Deliv 23:1335–1343. https://doi.org/10.3109/10717544.2014.991432
Suksaeree J, Treelop A, Veeravatanayothin P et al (2020) Stability test of nanostructured lipid carriers-loaded mefenamic acid prepared by microemulsion technique. IOP Conf Ser Mater Sci Eng 840:012001. https://doi.org/10.1088/1757-899X/840/1/012001
Galvão JG, Santos RL, Silva ARST et al (2020) Carvacrol loaded nanostructured lipid carriers as a promising parenteral formulation for leishmaniasis treatment. Eur J Pharm Sci 150:105335. https://doi.org/10.1016/J.EJPS.2020.105335
Kharkar PB, Talkar SS, Patravale VB (2020) An industrially viable technique for fabrication of docetaxel NLCs for oncotherapy. Int J Pharm 577:119082. https://doi.org/10.1016/J.IJPHARM.2020.119082
Otarola JJ, Cobo Solis AK, Farias ME et al (2020) Piroxicam-loaded nanostructured lipid carriers gel: design and characterization by square wave voltammetry. Colloids Surfaces A Physicochem Eng Asp 606:125396. https://doi.org/10.1016/J.COLSURFA.2020.125396
Otarola J, Molina PG, Garrido M, Correa NM (2021) Spectroscopic characterization and general features of piroxicam encapsulated in nanostructured lipid carriers. Colloids Surfaces A Physicochem Eng Asp 616:126340. https://doi.org/10.1016/J.COLSURFA.2021.126340
Kaur N, Sharma K, Bedi N (2018) Topical nanostructured lipid carrier based hydrogel of mometasone furoate for the treatment of psoriasis. Pharm Nanotechnol 6:133–143. https://doi.org/10.2174/2211738506666180523112513
Ebrahimi S, Farhadian N, Karimi M, Ebrahimi M (2020) Enhanced bactericidal effect of ceftriaxone drug encapsulated in nanostructured lipid carrier against gram-negative Escherichia coli bacteria: drug formulation, optimization, and cell culture study. Antimicrob Resist Infect Control 9:28. https://doi.org/10.1186/s13756-020-0690-4
Ghani SMA, Roslan NZI, Muda R, Abdul-Aziz A (2021) Encapsulation of Ficus deltoidea extract in nanostructured lipid carrier for anti-melanogenic activity. Bionanoscience 11:8–20. https://doi.org/10.1007/s12668-020-00786-2
Amasya G, Badilli U, Aksu B, Tarimci N (2016) Quality by design case study 1: design of 5-fluorouracil loaded lipid nanoparticles by the W/O/W double emulsion—Solvent evaporation method. Eur J Pharm Sci 84:92–102. https://doi.org/10.1016/j.ejps.2016.01.003
Lee H-J, Jeong M, Na Y-G et al (2020) An EGF- and curcumin-co-encapsulated nanostructured lipid carrier accelerates chronic-wound healing in diabetic rats. Molecules 25:4610. https://doi.org/10.3390/molecules25204610
Ghasemian E, Vatanara A, Navidi N, Rouini MR (2017) Brain delivery of baclofen as a hydrophilic drug by nanolipid carriers: characteristics and pharmacokinetics evaluation. J Drug Deliv Sci Technol 37:67–73. https://doi.org/10.1016/j.jddst.2016.06.012
Baruah UK, Gowthamarajan K, Ravisankar V et al (2018) Optimisation of chloroquine phosphate loaded nanostructured lipid carriers using Box-Behnken design and its antimalarial efficacy. J Drug Target 26:576–591. https://doi.org/10.1080/1061186X.2017.1390671
Maurya VK, Aggarwal M (2019) Fabrication of nano-structured lipid carrier for encapsulation of vitamin D3 for fortification of ‘Lassi’; a milk based beverage. J Steroid Biochem Mol Biol 193:105429. https://doi.org/10.1016/j.jsbmb.2019.105429
Shinde UA, Parmar SJ, Easwaran S (2019) Metronidazole-loaded nanostructured lipid carriers to improve skin deposition and retention in the treatment of rosacea. Drug Dev Ind Pharm 45:1039–1051. https://doi.org/10.1080/03639045.2019.1569026
Montenegro L, Messina C, Manuguerra S et al (2019) In vitro antioxidant activity and in vivo topical efficacy of lipid nanoparticles co-loading idebenone and tocopheryl acetate. Appl Sci 9:845. https://doi.org/10.3390/app9050845
Carbone C, Caddeo C, Grimaudo MA et al (2020) Ferulic acid-NLC with Lavandula essential oil: a possible strategy for wound-healing? Nanomaterials 10:898. https://doi.org/10.3390/nano10050898
Takalkar D, Desai N (2018) Nanolipid gel of an antimycotic drug for treating vulvovaginal candidiasis—development and evaluation. AAPS PharmSciTech 19:1297–1307. https://doi.org/10.1208/s12249-017-0918-7
Gomes GVL, Sola MR, Rochetti AL et al (2019) β-carotene and α-tocopherol coencapsulated in nanostructured lipid carriers of murumuru (Astrocaryum murumuru) butter produced by phase inversion temperature method: characterisation, dynamic in vitro digestion and cell viability study. J Microencapsul 36:43–52. https://doi.org/10.1080/02652048.2019.1585982
Ha E-S, Sim W-Y, Lee S-K et al (2019) Preparation and evaluation of resveratrol-loaded composite nanoparticles using a supercritical fluid technology for enhanced oral and skin delivery. Antioxidants 8:554. https://doi.org/10.3390/antiox8110554
Shadambikar G, Marathe S, Ji N et al (2021) Formulation development of itraconazole PEGylated nano-lipid carriers for pulmonary aspergillosis using hot-melt extrusion technology. Int J Pharm X 3:100074. https://doi.org/10.1016/J.IJPX.2021.100074
Selvaraj K, Yoo B-K (2019) Curcumin-loaded nanostructured lipid carrier modified with partially hydrolyzed ginsenoside. AAPS PharmSciTech 20:252. https://doi.org/10.1208/s12249-019-1467-z
Mishra RK, Ahmad A, Kumar A et al (2020) Lipid-based nanocarrier-mediated targeted delivery of celecoxib attenuate severity of ulcerative colitis. Mater Sci Eng C 116:111103. https://doi.org/10.1016/J.MSEC.2020.111103
Ghodrati M, Farahpour MR, Hamishehkar H (2019) Encapsulation of Peppermint essential oil in nanostructured lipid carriers: In-vitro antibacterial activity and accelerative effect on infected wound healing. Colloids Surfaces A Physicochem Eng Asp 564:161–169. https://doi.org/10.1016/J.COLSURFA.2018.12.043
Nobari Azar FA, Pezeshki A, Ghanbarzadeh B et al (2020) Nanostructured lipid carriers: promising delivery systems for encapsulation of food ingredients. J Agric Food Res 2:100084. https://doi.org/10.1016/j.jafr.2020.100084
Hanna PA, Ghorab MM, Gad S (2019) Development of betamethasone dipropionate-loaded nanostructured lipid carriers for topical and transdermal delivery. Antiinflamm Antiallergy Agents Med Chem 18:26–44. https://doi.org/10.2174/1871523017666181115104159
Mishra V, Bansal K, Verma A et al (2018) Solid lipid nanoparticles: emerging colloidal nano drug delivery systems. Pharmaceutics 10:191. https://doi.org/10.3390/pharmaceutics10040191
Uprit S, Kumar Sahu R, Roy A, Pare A (2013) Preparation and characterization of minoxidil loaded nanostructured lipid carrier gel for effective treatment of alopecia. Saudi Pharm J 21:379–385. https://doi.org/10.1016/j.jsps.2012.11.005
Mohammadi M, Assadpour E, Jafari SM (2019) Encapsulation of food ingredients by nanostructured lipid carriers (NLCs). In: Jafari SM (ed) Lipid-based nanostructures for food encapsulation purposes. Elsevier, pp 217–270
Ezzati Nazhad Dolatabadi J, Valizadeh H, Hamishehkar H (2015) Solid lipid nanoparticles as efficient drug and gene delivery systems: recent breakthroughs. Adv Pharm Bull 5:151–159. https://doi.org/10.15171/apb.2015.022
Purohit DK, Nandgude TD, Poddar SS (2016) Nano-lipid carriers for topical application: current scenario. Asian J Pharm 10:S1–S9. https://doi.org/10.22377/AJP.V10I1.544
Chandana KV, Gupta NV, Kanna S (2019) Nanostructured lipid carriers: The frontiers in drug delivery. Asian J Pharm Clin Res 12:8–12. https://doi.org/10.22159/ajpcr.2019.v12i7.33595
Dai W, Zhang D, Duan C et al (2010) Preparation and characteristics of oridonin-loaded nanostructured lipid carriers as a controlled-release delivery system. J Microencapsul 27:234–241. https://doi.org/10.3109/02652040903079526
Luan J, Zhang D, Hao L et al (2013) Design and characterization of Amoitone B-loaded nanostructured lipid carriers for controlled drug release. Drug Deliv 20:324–330. https://doi.org/10.3109/10717544.2013.835007
Siahdasht FN, Farhadian N, Karimi M, Hafizi L (2020) Enhanced delivery of melatonin loaded nanostructured lipid carriers during in vitro fertilization: NLC formulation, optimization and IVF efficacy. RSC Adv 10:9462–9475. https://doi.org/10.1039/C9RA10867J
Singh R, Lillard JW Jr (2009) Nanoparticle-based targeted drug delivery. Exp Mol Pathol 86:215. https://doi.org/10.1016/J.YEXMP.2008.12.004
Kadam VB, Dhanawade KB, Salunkhe VA, Ubale AT (2014) Nanoparticle-novel drug delivery system. J Curr Pharma Res 4:1318–1335
Loo C, Basri M, Ismail R et al (2012) Effect of compositions in nanostructured lipid carriers (NLC) on skin hydration and occlusion. Int J Nanomedicine 8:13–22. https://doi.org/10.2147/IJN.S35648
Nanjwade BK, Kadam VT, Manvi FV (2013) Formulation and characterization of nanostructured lipid carrier of ubiquinone (Coenzyme Q10). J Biomed Nanotechnol 9:450–460. https://doi.org/10.1166/jbn.2013.1560
Teng Z, Yu M, Ding Y et al (2018) Preparation and characterization of nimodipine-loaded nanostructured lipid systems for enhanced solubility and bioavailability. Int J Nanomed 14:119–133. https://doi.org/10.2147/IJN.S186899
Gaba B, Fazil M, Ali A et al (2014) Nanostructured lipid (NLCs) carriers as a bioavailability enhancement tool for oral administration. Drug Deliv 22:691–700. https://doi.org/10.3109/10717544.2014.898110
Mura P, Maestrelli F, D’Ambrosio M et al (2021) Evaluation and comparison of solid lipid nanoparticles (SLNs) and nanostructured lipid carriers (NLCs) as vectors to develop hydrochlorothiazide effective and safe pediatric oral liquid formulations. Pharmaceutics 13:437. https://doi.org/10.3390/pharmaceutics13040437
Üner M, Yener G (2007) Importance of solid lipid nanoparticles (SLN) in various administration routes and future perspectives. Int J Nanomedicine 2:289
Lacatusu I, Badea N, Stan R, Meghea A (2012) Novel bio-active lipid nanocarriers for the stabilization and sustained release of sitosterol. Nanotechnology 23:455702. https://doi.org/10.1088/0957-4484/23/45/455702
Sapkota M, Karmakar G, Nahak P et al (2015) Effect of polymer charge on the formation and stability of anti-inflammatory drug loaded nanostructured lipid carriers: physicochemical approach. RSC Adv 5:65697–65709. https://doi.org/10.1039/C5RA11066A
Pinheiro M, Ribeiro R, Vieira A et al (2016) Design of a nanostructured lipid carrier intended to improve the treatment of tuberculosis. Drug Des Devel Ther 10:2467–2475. https://doi.org/10.2147/DDDT.S104395
Singh B, Bandyopadhyay S, Kapil R, Katare OP (2009) Novel nanostructured lipidic drug delivery systems. Pharma Rev 7:118–122
Nandvikar NY, Lala RR, Shinde AS (2019) Nanostructured lipid carrier: the advanced lipid carriers. Int J Pharm Sci Res 10:5252–5265. https://doi.org/10.13040/IJPSR.0975-8232.10(12).5252-65
Al-Qushawi A, Rassouli A, Atyabi F et al (2016) Preparation and characterization of three tilmicosin-loaded lipid nanoparticles: physicochemical properties and in-vitro antibacterial activities. Iran J Pharm Res 15:676
Xia D, Shrestha N, van de Streek J et al (2016) Spray drying of fenofibrate loaded nanostructured lipid carriers. Asian J Pharm Sci 11:507–515. https://doi.org/10.1016/J.AJPS.2016.01.001
Zhang X, Pan W, Gan L et al (2008) Preparation of a Dispersible PEGylate Nanostructured Lipid Carriers (NLC) loaded with 10-hydroxycamptothecin by spray-drying. Chem Pharm Bull 56:1645–1650. https://doi.org/10.1248/CPB.56.1645
Bodratti A, Alexandridis P (2018) Formulation of poloxamers for drug delivery. J Funct Biomater 9:11. https://doi.org/10.3390/jfb9010011
Sahoo L (2020) Nanostructured lipid carrier (NLC)—a promising drug delivery for transdermal application. J Pharm Sci Res 12:475–487
Devi DR, Sandhya P, Vedha Hari B (2013) Poloxamer: a novel functional molecule for drug delivery and gene therapy. J Pharm Sci Res 5:159–165
Karmakar G, Nahak P, Guha P et al (2018) Role of PEG 2000 in the surface modification and physicochemical characteristics of pyrazinamide loaded nanostructured lipid carriers. J Chem Sci 130:1–9. https://doi.org/10.1007/S12039-018-1448-X
Hamidi M, Azadi A, Rafiei P, Ashrafi H (2013) A Pharmacokinetic overview of nanotechnology-based drug delivery systems: an ADME-oriented approach. Crit Rev Ther Drug Carr Syst 30:435–467. https://doi.org/10.1615/CRITREVTHERDRUGCARRIERSYST.2013007419
Mehnert W, Mäder K (2012) Solid lipid nanoparticles. Adv Drug Deliv Rev 64:83–101. https://doi.org/10.1016/j.addr.2012.09.021
Beloqui A, Solinís MÁ, Delgado A et al (2014) Fate of nanostructured lipid carriers (NLCs) following the oral route: design, pharmacokinetics and biodistribution. J Microencapsul 31:1–8. https://doi.org/10.3109/02652048.2013.788090
McClements DJ (2013) Edible lipid nanoparticles: digestion, absorption, and potential toxicity. Prog Lipid Res 52:409–423. https://doi.org/10.1016/j.plipres.2013.04.008
Poovi G, Damodharan N (2018) Lipid nanoparticles: a challenging approach for oral delivery of BCS Class-II drugs. Futur J Pharm Sci 4:191–205. https://doi.org/10.1016/j.fjps.2018.04.001
Feeney OM, Crum MF, McEvoy CL et al (2016) 50 years of oral lipid-based formulations: provenance, progress and future perspectives. Adv Drug Deliv Rev 101:167–194. https://doi.org/10.1016/j.addr.2016.04.007
Xue HY, Wong HL (2011) Tailoring nanostructured solid-lipid carriers for time-controlled intracellular siRNA kinetics to sustain RNAi-mediated chemosensitization. Biomaterials 32:2662–2672. https://doi.org/10.1016/j.biomaterials.2010.12.029
Qi J, Zhuang J, Lu Y et al (2017) In vivo fate of lipid-based nanoparticles. Drug Discov Today 22:166–172. https://doi.org/10.1016/j.drudis.2016.09.024
Scioli Montoto S, Muraca G, Ruiz ME (2020) Solid lipid nanoparticles for drug delivery: pharmacological and biopharmaceutical aspects. Front Mol Biosci. https://doi.org/10.3389/fmolb.2020.587997
Tosi G, Musumeci T, Ruozi B et al (2016) The “fate” of polymeric and lipid nanoparticles for brain delivery and targeting: Strategies and mechanism of blood–brain barrier crossing and trafficking into the central nervous system. J Drug Deliv Sci Technol 32:66–76. https://doi.org/10.1016/j.jddst.2015.07.007
Fang G, Tang B, Chao Y et al (2015) Cysteine-functionalized nanostructured lipid carriers for oral delivery of docetaxel: a permeability and pharmacokinetic study. Mol Pharm 12:2384–2395. https://doi.org/10.1021/acs.molpharmaceut.5b00081
Khosa A, Saha RN, Singhvi G (2019) Drug delivery to the brain. In: Grumezescu AM (ed) Nanomaterials for drug delivery and therapy. William Andrew Publishing, pp 461–514
Martin-Banderas L, Holgado MA, Venero JL et al (2011) Nanostructures for drug delivery to the brain. Curr Med Chem 18:5303–5321. https://doi.org/10.2174/092986711798184262
Agrawal M, Saraf S, Saraf S et al (2020) Recent strategies and advances in the fabrication of nano lipid carriers and their application towards brain targeting. J Control Release 321:372–415. https://doi.org/10.1016/J.JCONREL.2020.02.020
Alexander A, Ajazuddin M, Swarna M et al (2011) Polymers and permeation enhancers: specialized components of mucoadhesives. Stamford J Pharm Sci 4:91–95. https://doi.org/10.3329/SJPS.V4I1.8878
Gao H (2016) Progress and perspectives on targeting nanoparticles for brain drug delivery. Acta Pharm Sin B 6:268–286. https://doi.org/10.1016/J.APSB.2016.05.013
Lombardo SM, Schneider M, Türeli AE, Günday Türeli N (2020) Key for crossing the BBB with nanoparticles: the rational design. Beilstein J Nanotechnol 11:866–883. https://doi.org/10.3762/bjnano.11.72
Crowe TP, Greenlee MHW, Kanthasamy AG, Hsu WH (2018) Mechanism of intranasal drug delivery directly to the brain. Life Sci 195:44–52. https://doi.org/10.1016/J.LFS.2017.12.025
Veronesi MC, Alhamami M, Miedema SB et al (2020) Imaging of intranasal drug delivery to the brain. Am J Nucl Med Mol Imaging 10:31
Kumar H, Mishra G, Sharma AK et al (2017) Intranasal drug delivery: a non-invasive approach for the better delivery of neurotherapeutics. Pharm Nanotechnol 5:1–12. https://doi.org/10.2174/2211738505666170515113936
Alexander A, Agrawal M, Bhupal Chougule M et al (2020) Nose-to-brain drug delivery. In: Shegokar R (ed) Nanopharmaceuticals. Elsevier, pp 175–200
Tomeh MA, Hadianamrei R, Zhao X (2019) A review of curcumin and its derivatives as anticancer agents. Int J Mol Sci 20:1033. https://doi.org/10.3390/IJMS20051033
Giordano A, Tommonaro G (2019) Curcumin and cancer. Nutrients 11:2376. https://doi.org/10.3390/NU11102376
Lopresti AL (2018) The problem of curcumin and its bioavailability: could its gastrointestinal influence contribute to its overall health-enhancing effects? Adv Nutr 9:41–50. https://doi.org/10.1093/ADVANCES/NMX011
Chen Y, Pan L, Jiang M et al (2015) Nanostructured lipid carriers enhance the bioavailability and brain cancer inhibitory efficacy of curcumin both in vitro and in vivo. Drug Deliv 23:1383–1392. https://doi.org/10.3109/10717544.2015.1049719
Madane RG, Mahajan HS (2016) Curcumin-loaded nanostructured lipid carriers (NLCs) for nasal administration: design, characterization, and in vivo study. Drug Deliv 23:1326–1334. https://doi.org/10.3109/10717544.2014.975382
Slezakova S, Ruda-Kucerova J (2017) Anticancer activity of artemisinin and its derivatives. Anticancer Res 37:5995–6003. https://doi.org/10.21873/ANTICANRES.12046
Emami J, Yousefian H, Sadeghi H (2018) Targeted nanostructured lipid carrier for brain delivery of artemisinin: design, preparation, characterization, optimization and cell toxicity. J Pharm Pharm Sci 21:225–241. https://doi.org/10.18433/JPPS30117
Emami J, Rezazadeh M, Sadeghi H, Khadivar K (2016) Development and optimization of transferrin-conjugated nanostructured lipid carriers for brain delivery of paclitaxel using Box-Behnken design. Pharm Dev Technol 22:370–382. https://doi.org/10.1080/10837450.2016.1189933
Sharma P, Dube B, Sawant K (2011) Development and evaluation of nanostructured lipid carriers of cytarabine for treatment of meningeal leukemia. J Nanosci Nanotechnol 11:6676–6682. https://doi.org/10.1166/JNN.2011.4235
Khan A, Imam SS, Aqil M et al (2016) Brain targeting of temozolomide via the intranasal route using lipid-based nanoparticles: brain pharmacokinetic and scintigraphic analyses. Mol Pharm 13:3773–3782. https://doi.org/10.1021/ACS.MOLPHARMACEUT.6B00586
Qu J, Zhang L, Chen Z et al (2016) Nanostructured lipid carriers, solid lipid nanoparticles, and polymeric nanoparticles: which kind of drug delivery system is better for glioblastoma chemotherapy? Drug Deliv 23:3408–3416. https://doi.org/10.1080/10717544.2016.1189465
Song S, Mao G, Du J, Zhu X (2015) Novel RGD containing, temozolomide-loading nanostructured lipid carriers for glioblastoma multiforme chemotherapy. Drug Deliv 23:1404–1408. https://doi.org/10.3109/10717544.2015.1064186
Wu M, Fan Y, Lv S et al (2015) Vincristine and temozolomide combined chemotherapy for the treatment of glioma: a comparison of solid lipid nanoparticles and nanostructured lipid carriers for dual drugs delivery. Drug Deliv 23:2720–2725. https://doi.org/10.3109/10717544.2015.1058434
Bala V, Rao S, Boyd BJ, Prestidge CA (2013) Prodrug and nanomedicine approaches for the delivery of the camptothecin analogue SN38. J Control Release 172:48–61. https://doi.org/10.1016/J.JCONREL.2013.07.022
Shirazi AS, Varshochian R, Rezaei M et al (2021) SN38 loaded nanostructured lipid carriers (NLCs); preparation and in vitro evaluations against glioblastoma. J Mater Sci Mater Med 32:1–12. https://doi.org/10.1007/S10856-021-06538-2
Rauf A, Imran M, Khan IA et al (2018) Anticancer potential of quercetin: A comprehensive review. Phyther Res 32:2109–2130. https://doi.org/10.1002/PTR.6155
Patil NL, Mahajan HS (2017) Quercetin loaded nanostructured lipid carriers for nose to brain delivery. In vitro and in vivo studies. Am J Adv Drug Deliv 6:9–20. https://doi.org/10.21767/2321-547X.1000022
Ko J-H, Sethi G, Um J-Y et al (2017) The role of resveratrol in cancer therapy. Int J Mol Sci 18:2589. https://doi.org/10.3390/IJMS18122589
Kumar N, Gupta GD, Arora D (2021) DoE directed optimization, development and characterization of resveratrol loaded Nlc system for the nose to brain delivery in the management of glioblastoma multiforme. Res Sq 9:99. https://doi.org/10.21203/RS.3.RS-572155/V1
Carbone C, Campisi A, Musumeci T et al (2014) FA-loaded lipid drug delivery systems: preparation, characterization and biological studies. Eur J Pharm Sci 52:12–20. https://doi.org/10.1016/J.EJPS.2013.10.003
Grasso R, Dell’Albani P, Carbone C et al (2020) Synergic pro-apoptotic effects of Ferulic Acid and nanostructured lipid carrier in glioblastoma cells assessed through molecular and delayed luminescence studies. Sci Rep 10:1–13. https://doi.org/10.1038/s41598-020-61670-3
Simão DO, Honorato TD, Gobo GG et al (2020) Preparation and cytotoxicity of lipid nanocarriers containing a hydrophobic flavanone. Colloids Surfaces A Physicochem Eng Asp 601:124982. https://doi.org/10.1016/j.colsurfa.2020.124982
Dana P, Yostawonkul J, Chonniyom W et al (2021) Nanostructured lipid base carrier for specific delivery of garlic oil through blood brain barrier against aggressiveness of glioma. J Drug Deliv Sci Technol 64:102651. https://doi.org/10.1016/J.JDDST.2021.102651
Zwain T, Alder JE, Sabagh B et al (2021) Tailoring functional nanostructured lipid carriers for glioblastoma treatment with enhanced permeability through in-vitro 3D BBB/BBTB models. Mater Sci Eng C 121:111774. https://doi.org/10.1016/j.msec.2020.111774
Chen M, Cui Y, Hao W et al (2021) Ligand-modified homologous targeted cancer cell membrane biomimetic nanostructured lipid carriers for glioma therapy. Drug Deliv 28:2241–2255. https://doi.org/10.1080/10717544.2021.1992038
Talkar SS, Kharkar PB, Patravale VB (2020) Docetaxel loaded pomegranate seed oil based nanostructured lipid carriers: a potential alternative to current formulation. AAPS PharmSciTech 21:295. https://doi.org/10.1208/s12249-020-01839-1
Chang L, Zhang Y, Li M et al (2021) Nanostructured lipid carrier co-delivering paclitaxel and doxorubicin restrains the proliferation and promotes apoptosis of glioma stem cells via regulating PI3K/Akt/mTOR signaling. Nanotechnology 32:225101. https://doi.org/10.1088/1361-6528/abd439
Nasirizadeh S, Malaekeh-Nikouei B (2020) Solid lipid nanoparticles and nanostructured lipid carriers in oral cancer drug delivery. J Drug Deliv Sci Technol 55:101458. https://doi.org/10.1016/J.JDDST.2019.101458
Elmowafy M, Al-Sanea MM (2021) Nanostructured lipid carriers (NLCs) as drug delivery platform: advances in formulation and delivery strategies. Saudi Pharm J 29:999–1012. https://doi.org/10.1016/J.JSPS.2021.07.015
Müller RH, Petersen RD, Hommoss A, Pardeike J (2007) Nanostructured lipid carriers (NLC) in cosmetic dermal products. Adv Drug Deliv Rev 59:522–530. https://doi.org/10.1016/J.ADDR.2007.04.012
Ghasemiyeh P, Mohammadi-Samani S (2018) Solid lipid nanoparticles and nanostructured lipid carriers as novel drug delivery systems: applications, advantages and disadvantages. Res Pharm Sci 13:303. https://doi.org/10.4103/1735-5362.235156
Pardeike J, Hommoss A, Müller RH (2009) Lipid nanoparticles (SLN, NLC) in cosmetic and pharmaceutical dermal products. Int J Pharm 366:170–184. https://doi.org/10.1016/J.IJPHARM.2008.10.003
Montenegro L (2017) Lipid-Based nanoparticles as carriers for dermal delivery of antioxidants. Curr Drug Metab 18:469–480. https://doi.org/10.2174/1389200218666170222152038
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JG conceptualized and drafted the manuscript. KP was a major contributor in editing and revising. SPS substantively reviewed the draft. SVP conceptualized and reviewed the draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Garg, J., Pathania, K., Sah, S.P. et al. Nanostructured lipid carriers: a promising drug carrier for targeting brain tumours. Futur J Pharm Sci 8, 25 (2022). https://doi.org/10.1186/s43094-022-00414-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43094-022-00414-8