Abstract
Background
Coconut oil, a natural component abundant in terpenoids, possesses various physiological functions. The global concern over the spread of viral infections and antimicrobial-resistant bacteria and fungi has highlighted the need for novel treatments. Coconut oil, with its known antimicrobial properties, presents an attractive candidate for combating these pathogens. This study aims to investigate the potential of coconut oil-loaded silica nanoemulsion (ON@SiO2) as a novel therapeutic agent against viral, antimicrobial-resistant bacteria, and fungal pathogens.
Results
The study synthesized coconut oil-loaded silica nanoemulsion (ON@SiO2) using an eco-friendly, cost-effective method with native coconut oil (CO). Characterization confirmed successful synthesis on the nanoscale with good distribution. Three nanoemulsion samples (ON-1@SiO2, ON-2@SiO2, and ON-3@SiO2) were prepared, with average particle sizes of 193 nm, 200 nm, and 325 nm, respectively. Evaluation of cytotoxicity on Vero-E6 cell lines indicated safety of ON-0@SiO2 and ON-3@SiO2, with CC50 values of 97.5 mg/ml and 89.1 mg/ml, respectively. ON-3@SiO2 demonstrated anti-Herpes I and II (HSV1 and HSV2) activity, with IC50 values of 1.9 mg/ml and 2.1 mg/ml, respectively. Additionally, ON-3@SiO2 exhibited promising antibacterial activity against E. coli, P. aeruginosa, S. aureus, and B. subtilis, with MIC values of 25 mg/ml, 12.5 mg/ml, 25 mg/ml, and 3.12 mg/ml, respectively.
Conclusions
ON-3@SiO2 showed potential antifungal activity against C. albicans, a unicellular fungus, with an MIC of 12.5 mg/ml. Overall, ON@SiO2 possesses antiviral, antibacterial, and antifungal properties.
Similar content being viewed by others
1 Background
Antimicrobial resistance (AMR) is one of the top global public health and development threats. It is estimated that bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths [1]. Unfortunately, the number of deaths attributable to antimicrobial resistance is expected to exceed those caused by cancer by 2050 [2]. The development of drugs resistant to the microbial effect stimulates the search for new alternatives with unique action modes. Virgin coconut oil is derived from the plant species Cocos nucifera Linn (Arecaceae), primarily found in tropical regions [3]. The oil mainly consists of medium-chain fatty acids, particularly lauric acid, and other fatty acids, including oleic and linoleic acids. Coconut oil has been observed to possess a notable capacity for absorption, exhibiting a propensity for enhancing cellular metabolism, promoting wound moisture, and mitigating inflammatory manifestations [4]. Hydrolyzing coconut oil often forms monoglycerides, diglycerides, and free fatty acids. Coconut oil exhibits potential for wound-healing formulations due to its antibacterial and antifungal properties, mainly attributed to monoglycerides, free fatty acids, lauric acid, and monolaurin [5].
Commercial coconut oil the lack of antimicrobial activity [6] corroborates the idea of catalytic need in the antimicrobial properties of coconut oil and coconut milk-derived products. A nano-sized emulsion can enhance functional compounds, such as bioactive lipids, antioxidants, and antimicrobials [7]. Nanoemulsions (NEs) refer to heterogeneous formulations consisting of two immiscible liquids, commonly oil, and water that are stabilized by surfactants, which are surface-active agents. During the process of emulsification, surfactants play a crucial role in minimizing or preventing the coalescence of oil droplets by adsorbing at the interface between oil and water, hence reducing the surface tension. Surfactants have a role in promoting the separation or disruption of dispersed phases by creating a film at the interface between oil and water, which effectively delays mechanisms that lead to destabilization. The selection of surfactants plays a crucial role in the formulation of nanoemulsions since it determines the desired physiochemical characteristics of the final product. Nanoemulsions (NEs) exhibit droplet sizes within the range of 10 to 1000 nm, rendering them kinetically stable but thermodynamically unstable systems. This instability arises from the larger free energy present within the system in comparison with the individual phases [8]. Consequently, the process of phase separation in homogenized NEs is influenced by the presence of kinetic energy barriers. This phenomenon unfolds gradually over time and gives rise to destabilizing processes such as Ostwald ripening and flocculation. Nevertheless, it is possible for nanoemulsions (NEs) to exhibit extended durability or shelf-life, provided the chosen system components are rationalized according to their physiochemical characteristics. The stability of nanoemulsions (NEs) is a critical feature in medical applications since any changes in their physiochemical properties can significantly affect the pharmacological properties of the formulation. NEs are a burgeoning category of colloidal carriers that possess distinct characteristics enabling their effective and cost-efficient utilization in several fields, such as cosmetics [9], food [10], pharmaceuticals [8, 11], and agriculture [12].
Infectious viral diseases and outbreaks are continuously evolving global threats. Despite successive advances in the medical field, the prevention and treatment of viral outbreaks remain challenging due to the innate characteristics of viral particles, such as the high dynamic rate of genetic mutations [13]. Viruses and microorganisms' ability to resist drugs is a problem in chemotherapy. Viruses have many genetic variations and mechanisms for their survival [14, 15]. New methods for developing antiviral drugs are required due to the emergence of virus resistance. As a result, advances in novel medications and antiviral therapeutic techniques continue. New drug research has many prospects thanks to nanotechnologies. The antiviral activity of nonfunctionalized nanoparticles is a crucial finding [16] of specific interest, mainly because the watched activity probably results from a new mechanism of action. The experimental evidence for no functionalized nanoparticles' antiviral activity [17] and the findings shown in this communication allow for an agent based on the proximity interaction of nanoparticles with the viral envelope and its constituent parts.
HSV1 and HSV2 are common human diseases in the alpha herpes virus family [18]. Every herpes virus has an enveloped virion with an icosahedral nucleocapsid that contains the genome's double-stranded linear DNA. HSV's neurovirulence and latency directly impact humans and the illness's progression. This can lead to severe neurological consequences, such as HSV encephalitis and profound disease. HSV creates a prolonged infection by dodging the host's immunological response. The HSV genome is kept in a suppressed condition in the neural cells throughout latency. The viral genome may then be activated and transmitted to the skin by the neuron's axon, leading to viral replication and the regrowth of herpetic sores. Due to the rise in immunocompromised individuals and sexual activity, HSV incidence and severity have grown over the past few decades. Close intimate touch is when HSV1 and HSV2 transmission happens. Most people get latently infected with HSV1 in infancy or early adolescence and carry it with them for the rest of their lives. HSV2 spreads mainly through sexual contact. Although it aids in infection management, administering antiviral medications after latency development will not result in the virus' eradication. Herpes labialis, herpetic gingivostomatitis, herpes genitalis, keratitis, encephalitis, and newborn herpes infection are all brought on by HSV [19]. After initial infection, the virus creates a lifelong latent infection in the sensory and autonomic brain ganglia. HSV can cause life-threatening conditions in infants and those with weakened immune systems, physical disabilities, social marginalization, and psychological suffering [20]. HSV1 and HSV2 infections have affected, respectively, 3.7 billion and 417 million persons worldwide, according to a 2012 World Health Organization (WHO) study [21].
HSV infections and reactivation are treated with acyclovir (ACV), penciclovir (PCV), and related pro-drugs [22]. The emergence of medication resistance in high-risk populations, including immunocompromised individuals and transplant recipients, motivated researchers to look for new therapeutic agents with a distinct mode of action [19]. Additionally, antimicrobial resistance occurs when fungi and bacteria evolve to resist the medications created to kill them. The overuse of antibiotics, which has given microorganisms the capacity to form biofilms embedded in the extracellular matrix that make it difficult for antibiotics to enter cells, is one of the primary causes of this resistance [23, 24]. The discovery of innovative approaches for treating infections linked to antimicrobial resistance and biofilm formation in afflicted individuals has been prompted by the capacity of some strains of bacteria and fungi to resist the actions of conventional antibiotics and antifungals. Antimicrobial nanoemulsions are detergent, oil, and water combinations that have been emulsified. They exhibit overall antibacterial effectiveness against fungi, enveloped viruses, and bacteria; the size of the droplets ranges from 100 to 800 nm [25].
In the present study, coconut oil nanoemulsion was prepared with three different concentrations using 1.5, 3, and 6 ml of native coconut oil. An attempt has been made to evaluate them as anti-HSV, antibacterial and antifungal.
2 Methods
2.1 Materials
Coconut oil (CO) was obtained from Tropicana oil, Thailand. Tween®60 was purchased from WIN Lab Co. India. Tetraethyl orthosilicate (TEOS) was purchased from ALPHA CHEMIKA, Mumbai, India.
The chosen strains for evaluating the inhibitory activity of ON-0@SiO2 and ON-3@SiO2 include Escherichia coli ATCC 8739 and Pseudomonas aeruginosa ATCC 15442, which are gram-negative (G −) bacteria, Staphylococcus aureus ATCC 25923 and Bacillus subtilis ATCC 6633 which are gram-positive (G +) bacteria. At the same time, Candida albicans ATCC 10231 is a fungus strain. The strains used in the testing were from the import company Sigma-Aldrich's from the American Type Culture Collection.
2.2 Preparation of coconut oil nanoemulsion
The nanoemulsions containing coconut oil (CO) were prepared as follows: The oil phase was formed by adding (1.5, 3, and 6 ml) of CO to 30 ml H2O containing 1.5 ml of Tween® 60 as surfactant. Meanwhile, the aqueous phase was prepared by dissolving 3 ml of TEOS in 30 H2O. The two phases were separately stirred for 15 min using a homogenizer (1500 rpm). After that, the oil phase was added drop by drop to the aqueous phase (TEOS solution) and vigorously stirred using a high-speed homogenizer for 15 min. At the end of stirring time, the color of the whole solution was changed due to the preparation of CO-loaded SiO2 nanoemulsion. The blank nanoemulsion without oil (ON-0@SiO2) was prepared as previously mentioned, except for adding CO. The other samples of SiO2 loaded with three CO concentrations (1.5, 3, and 6 ml) are coded as ON-1@SiO2, ON-2@SiO2, and ON-3@SiO2, respectively. The formed nanoemulsions were kept in the refrigerator for further characterization and biological studies. The nanoemulsion characterization includes particle shape and topographical features.
2.3 Characterization of coconut oil nanoemulsion
2.3.1 Gas chromatography–mass spectrometry analysis (GC–MS) for phytochemical identification of coconut oil
The phytochemical constituents of coconut oil were determined using GC–MS analysis. After its solubilization in chloroform, the sample was injected into the GC apparatus. The investigation carried out at the Central Laboratories Network, Cairo, Egypt, utilized a GC–MS system from Agilent Technologies. The system consisted of a gas chromatograph (model 7890B) and a mass spectrometer detector (model 5977A). A gas chromatography apparatus was furnished with an HP-5MS column measuring 30 m in length, 0.25 mm in film thickness, and 0.25 mm in internal diameter. With a flow rate of 2.0 ml/min and a splitless injection volume of 1 µl, hydrogen gas was employed as the carrier gas. The investigation commenced with an initial temperature of 50 °C, which was maintained for a period of 5 min. Following this, the temperature was progressively raised until it reached 100 °C, after which it remained at this point for an interval of 0 min at a rate of 5 °C/min. In the end, the temperature was elevated to 320 °C and maintained at that level for 20 min, at a rate of 10 °C/ min. The temperatures of the injector and detector were maintained at 250 °C and 320 °C, correspondingly. With a solvent delay of 4 min, electron ionization at an energy level of 70 eV produced mass spectra spanning the range of m/z 25–700. Despite the Quad's recorded temperature of 150 °C, the mass temperature was determined to be 230 °C. By conducting a comparison between the fragmentation pattern of a spectrum and the data contained in the Wiley and NIST Mass Spectral Libraries, many constituents can be identified.
To determine the particle shape of the prepared nanoemulsion samples (ON-1@SiO2, ON-2@SiO2, and ON-3@SiO2), TEM (JEOL, 2100, Japan) was used. Firstly, the nanoemulsion samples were placed on a copper grid coated with a thin carbon film and dried in the air before TEM investigation. Meanwhile, the droplet size determination of the three prepared nanoemulsion samples was evaluated using Zetasizer Nano-ZS, Malvern (UK).
2.4 Antiviral activity
The Vero-E6 cells (105 cells/well) were plated on a 6-well tissue culture plate. Following two washes with 1X fetal bovine serum (FBS) at 90% to 100% confluence (one-day post-seeding), the virus was diluted tenfold in a medium containing 2% FBS (Lonza, USA) and 2% antibiotic–antimycotic combination (Lonza, Walkersville. MD, USA). Four hundred microliters of infection media was combined with 100 ul of each dilution before being used to inoculate a single well of Vero-E6 cells. A one-hour incubation period was performed at 37°C and 5% carbon dioxide. To get rid of any lingering inoculum, the wells were sucked. Afterward, 2 ml of 1:1 2X medium and 2% agarose type 1 overlay was quickly poured on each well (Lonza, Basel, Switzerland). The plates then spent three days in a 37°C, 5% CO2 incubator. The plaques were monitored daily under a microscope as they formed. Plaques were seen, and then 1 ml of 10% formaldehyde was added to each well and left there for 2 h at room temperature (TR) to kill the virus and fix the cells. Finally, the plates were washed with water and dried once the formaldehyde had been removed. After adding 1 ml of the staining solution (1% crystal violet and 20% methanol in distilled water) to each well and letting them sit at room temperature for 5 min, the plaques could be seen [26,27,28]. Then, the number of viral plaques was used to determine the titer of the virus using the following formula:
2.4.1 Cytotoxicity by MTT protocol (CC50)
The specimens were diluted by DMEM (Dulbecco's modified Eagle's medium). The test chemicals were dissolved in 10% DMSO in dd H2O to create stock solutions. The cytotoxic activity of the extracts was evaluated on Vero-E6 cells using a modified version of the 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) assay [29, 30]. Briefly, the cells were plated on 96 plates (100 ul/well at a density of 3*105 cells/ml) and incubated at 37 °C and 5% CO2 for 24 h. After 24 h, cells were treated in triplicate with varying doses of the test substances. After a further 72 h, the supernatant was removed, and the cell monolayers were washed three times with 1X phosphate-buffered saline (PBS) before MTT solution (20 ul of a 5 mg/ml stock solution) was added to each well and incubated at 37°C for 4 h, followed by medium aspiration. In each well, 200 ul of DMSO (0.04 M HCl in 100% isopropanol = 0.073 ml HCl in 50 ml isopropanol) was used to dissolve the formazan crystals. Using a multi-well plate reader, the absorbance of formazan solutions was measured at a max of 540 nm and 620 nm as the reference wavelength. The plot of percent cytotoxicity against sample concentration was used to determine the concentration at which 50% cytotoxicity was observed. “The % of cytotoxicity compared to the untreated cells was determined with the following equation:
2.4.2 Screening for antiviral activity by plaque reduction assay
MDCK cells were cultivated for 24 h in a six-well number plate at 37°C. The growth medium was removed from the cell culture plates, and the virus human herpes HSV1 and HSV2 viruses were inoculated (100 µL/well) and incubated at 37°C for one hour. Afterward, the numerous concentrations of ON-0@SiO2, ON-1@SiO2, ON-2@SiO2, and ON-3@SiO2 (100 µl/ well) were injected for one h and incubated at 37°C onto the infected cells. Next, one hour contact time, 1.5 ml of DMEM supplemented with 2% agarose was included in the cell monolayer; plates were left to solidify and incubated at 37°C to prepare the creation of viral plaques (through 3 days). Formalin (10%) was inserted for two hours. Plates were stained with 0.1% crystal violet in distilled water. Control wells were included where the untreated virus was incubated with cells, as studied by [31, 32]. Finally, plaques were enumerated, and the plaque reduction % relative to the control was recorded: \(\text{Inhibition}= {\text{Viral} \text{count}}_{\left(\text{untreated}\right)}- \frac{{\text{Viral} \text{count}}_{\left(\text{treated}\right)}}{{\text{Viral} \text{count}}_{\left(\text{untreated}\right)}}\times 100\).
2.4.3 Inhibitory concentration 50 (IC50) determination
Vero-E6 cells spread equally in a 96-well tissue culture plate (2.4 × 104) and incubated for 24 h in a humidified incubator at 37°C and 5% CO2. At room temperature, the monolayer cells were washed with subject and 1 × PBS for adsorption of a virus. Additionally, the monolayer cells were soaked in DMEM (100 ul), which contained oil-loaded silica nanoemulsion, and incubated for 72 h at 37°C and 5% CO2. Cells were stained with crystal violet (0.1%) for 15 min at RT in distilled water after being fixed in paraformaldehyde (100 ul of 4%) for 20 min. Then, crystal violet dye per well was dissolved by absolute methanol (100 ul) and measured at 570 nm of optical density. The oil-loaded silica nanoemulsion IC50 is a concentration of 50% of virus-induced cytopathic effects reduction relative to virus control [26,27,28].
2.4.4 Mode of action of virus inhibition
The possible mode of action of virus inhibition by the coconut oil-loaded silica nanoemulsion was examined at three potential mechanisms of action: (i) Inhibition of viral replication and budding. (ii) the direct effect of coconut oil-loaded silica nanoemulsion to inactivate the virus viability (virucidal activity) and (iii) The ability of coconut oil-loaded silica nanoemulsion to infected cells-membrane fusion to inhibit the attachment of the virus known as blocking the viral entry (protective activity or viral adsorption). For consistency, each action was repeated three times individually of each other, and the average of the three experiments of each activity was posed. Additionally, the above-mentioned mode of action could account for the recorded antiviral.
2.4.5 Infection Post-infection treatment (viral replication)
The 105 cells/ml vero-E6 cells (6-well plate) were incubated at 37°C for 24 h. The virus was transferred to the cells after being diluted to 10 PFU per well and incubated at 37°C for one hour to ensure complete adsorption. Additionally, wash cells with free medium supplements three times to eliminate unabsorbed viral particles. After one hour of oil-loaded silica nanoemulsion, the cell monolayer was overlaid with DMEM medium supplemented (3 ml) with agarose (2%). The viral plaques were shown after the hardening of plates, which were incubated at 37°C. The cell monolayers were stained with crystal violet dye after being fixed for two hours in 10% formalin. In the negative control well, the virus was incubated with vero-E6 cells without being treated with the oil-loaded silica nanoemulsion; on the other hand, remdesivir was used as positive control. Finally, we recorded the percentage of plaque reduction formation relative to control wells [26,27,28].
2.4.6 Cell pretreatment (protective activity) viral adsorption:
This protocol showed that the virus enters the host cell by preventing attachment to the cell surface. In the 6-well plate, Vero-E6 cells were cultivated at 37°C for 24 h for assay of viral adsorption. The oil-loaded silica nanoemulsion in different concentrations was applied in a medium (200 ul), and then the cell was incubated at 4°C for two hours. The oil-loaded silica nanoemulsion unabsorbed was eliminated by washing three times with a supplemented free medium. The diluted virus was set for one hour with the pretreated cell, adding DMEM increased with agarose (1%). The viral plaques formed after the plates hardened and incubated at 37°C. Fixed, stained, and recorded results, as mentioned above [26,27,28].
2.4.7 Virus pretreatment (virucidal):
In a 6-well plate, the vero-E6 monolayer cells were propagated at 37°C for 24 h for virucidal assy. DMED (200 ul) containing virus was added to nonlethal concentrations of oil-loaded silica nanoemulsion (1:1 V/V). After virus adsorption, incubated for one hour, diluting mixture by free medium each tenfold, whereas viral particles still grow on vero-E6 cells but no excess of oil-loaded silica nanoemulsion was present, then added 100 ul of each dilution to monolayer cells. DMEM was added to the top of the cell monolayer. The viral plaques formed after the plates solidified and incubated at 37 °C. Fixed, stained, and recorded results, as mentioned above [26,27,28].
2.5 Antibacterial and antifungal
2.5.1 Antimicrobial Activity
The antimicrobial activity of ON-0@SiO2 and ON-3@SiO2 against bacteria and fungi of clinical interest was tested. The technique was healthy diffusion using a slightly modified variation of the procedure mentioned by [33, 34]. The Petri dishes used for the test were sterilized and prepared with Sabouraud agar (SDA) medium for the growth of C. albicans and Muller–Hinton agar (MHA) medium for bacterial strain growth. The agar surface was inoculated using a sterile spreader with a microbe suspension adjusted to 0.5 McFarland's standard (equivalent to 108 CFU/ml for bacteria and 106 CFU/ml for C. albicans). A 6 mm-diameter hole was made using a sterile cork borer, and 100 μl of each microbe suspension was introduced to the well using a micropipette. Four concentrations of ON-0@SiO2 and ON-3@SiO2 were investigated, containing 100, 50, 25, and 12.5 mg/ml. The negative control was carried out with saline (0.85%), while the positive control was carried out by tetracycline for bacteria and ketoconazole for fungi. For bacterial strains, the plates were incubated at 37°C for 24 h and at 28°C for 72 h; for fungus, zones of inhibition for all plates were determined.
2.5.2 Determination MIC (minimum inhibitory concentration):
Using a standard broth microdilution method according to [35] in Muller–Hinton broth medium and a slightly altered form of the technique in Sabouraud broth medium for tested microorganisms.
Sterile distilled water was added to the wells, serving as the negative control using the Broth Micro dilution procedure. The same sort of suitable broth medium for bacteria and fungus was added to 100 µl (ul) plates to prepare them. A concentration of 100 to 3.12 mg/ml of the tested chemical was obtained by serial dilution. The control wells were left out, and each well received 20 ul of microbial suspension (0.5 McFarland standards) (control wells contained broth only and distilled water only). The absorbance of the plates was measured before and during incubation at 37°C after 24 h for bacteria and after 48 h at 28°C for fungi using an automated ELISA microplate reader (Sun Rise-TECAN, Inc. ®, USA) set at 600 (nm). The data were plotted versus concentration to assess the absorbencies and identify any changes in growth. Inhibiting bacterial or fungal growth at the lowest measured extract concentration was recorded as the MIC [35].
2.5.3 Determination of minimum bactericidal concentration (MBC) and minimum fungicidal concentration (MFC):
The wells of MICs obtained from the previous experiment were taken to be re-cultured on new media of MHA for bacteria and SDA for fungi. Plates of bacteria and fungi were incubated for appropriate time and temperature, depending on the organism type. The bactericidal endpoint (MBC) is the lowest concentration and eliminates 99.9% of the remaining germs [36]. MFC is the lowest drug concentration, killing ≥ 99.9% of cells [37]. The determination of MBC and MFC may be clinically more significant than the MIC of some antibacterial and antifungal drugs to effectively treat bacterial and fungal infections.
3 Results
3.1 GC–MS for the phytochemical identification of coconut oil
The study of bioactive phyto-compounds in coconut oil involved GC–MS analysis, revealing 17 compounds with diverse chemical structures and potential biological activities (Table 1 and Fig. 1). These compounds include 2(3H)-Furanone, dihydro-5-pentyl-, dodecanoic acid, oleic acid, 9,12-Octadecadienoyl chloride, dodecanoic acid, 3-hydroxy, oxiraneundecanoic acid, 7-Methyl-Z-tetradecen-1-ol acetate, 9-Hexadecenoic acid, 3-(Octanoyloxy)propane-1,2-diyl bis(decanoate), dodecanoic acid, 1-(hydroxymethyl)-1,2-ethanediyl ester, laurin, 1,2,3-propanetriyl ester, cyclobarbital, cyclobarbital, cyclobarbital, dodecyl cis-9,10-epoxyoctadecanoate, and Octadecanal, 2-bromo.
3.2 Characterization of coconut oil nanoemulsion
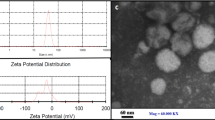
Our naked eye first investigated the as-prepared coconut oil nanoemulsion with different concentrations. It was observed that the prepared nanoemulsion samples were formed as a milky color with one phase. The absence of separation between nanoemulsion components confirmed the successful preparation. A high-speed homogenizer can potentially prepare coconut oil nanoemulsion with good distribution and blending of nanoemulsion components (TEOS, coconut oil, and Tween®60). Then, TEM was used to examine the shape of nanoemulsion particles (Fig. 2). Some samples were taken at two different magnifications to investigate the distribution of particles. It can be observed that the nanoemulsion sample (ON-1@SiO2) that was prepared using a low concentration of coconut oil (1.5 ml) has a spherical shape with uniform distribution (Fig. 2a, b) and is free to disperse without co free to distribute without aggregation. Increasing the concentration of coconut oil to 3 ml for the preparation of ON-2@SiO2 (Fig. 2c) leads to the formation of particles with nearly spherical shapes but with less distribution than ON-1@SiO2. However, high-speed homogenizer still has an efficient power to prepare uniformly nanoemulsion with small size. As observed from (Fig. 2a, c), there is no significant change regarding the particle shape or their distributions. On the contrary, increasing the concentration of coconut oil to 6 ml significantly affects the particle shape and distribution of the formed nanoemulsion. It can be observed that ON-3@SiO2 (Fig. 2d) does not have a specific condition as in the other two samples (ON-1@SiO2 and ON-2@SiO2). As seen from the TEM image (Fig. 2d), these particles have formed large aggregations, which can be attributed to using coconut oil with a high concentration (6 ml).
Dynamic light scattering was used to calculate the average size (200 nm) of coconut oil nanoemulsions (ON-1@SiO2 and ON-2@SiO2 and ON-3@SiO2), and the data were obtained as shown in Fig. 3a–c. It was observed that ON-1@SiO2 (Fig. 3a) has an average particle size of around 193.1 nm with a high percentage (97.5%), and there are about 2.5%with 4985 nm. The average particle size of the ON-2@SiO2 sample is 200 nm with a high percent (87.1%), and the other peak illustrates another size (5560 nm) with 12.9%. Moving on to the third nanoemulsion sample (ON-3@SiO2), it was found that the volume had increased significantly and recorded a value of 325.7 nm, with a percentage of 84.7%. While it was found that the sample has another size at 4985 nm, but with a small rate (2.5%), from the preceding, it can be said that the obtained results are broadly consistent with the results of TEM.
3.3 Cytotoxicity and antiviral of nanoemulsion evaluations
3.3.1 Cytotoxicity
Vero cell monolayers were incubated with various concentrations (0, 20, 50, 80, 150 mg/ml) of coconut oil and (0, 20, 50, 80, and 100 mg/ml) of ON-0@SiO2 and ON-3@SiO2 for multiple periods to rule out the possibility that the cellular toxicity of ON-0@SiO2 and ON-3@SiO2 brought on the reduction in infectivity. Data indicate that three experiments express values, value, mean, and standard deviation. After 48-h incubation, the MTT findings showed that coconut oil, ON-0@SiO2, and ON-3@SiO2 at concentrations up to 0, 20, 50, and 80 mg/ml did not cause cell death.
The study measured the cytotoxic activity of ON-0@SiO2 and ON-3@SiO2 in Vero-E6 cells using an MTT assay. The concentration which exhibited 50% cytotoxic concentration (CC50) was calculated and was found to be equal to 107.6 mg/ml for coconut oil (Fig. 4A), 97.5 mg/ml for ON-0@SiO2 (Fig. 4B), while CC50 was 89.1 mg/ml for ON-3@SiO2 (Fig. 4C).
3.4 Antiviral evaluation
In the current study, in searching for new anti-HSV1 and anti-HSV2 agents, the antiviral effects of ON-0@SiO2, ON-1@SiO2, ON-2@SiO2, and ON-3@SiO2 compared with Acyclovir (stander drug) after being measured using a plaque reduction assay. The antiviral effects were 28.3, 60.9, 73.9, and 76% for HSV1 with concentrations of 0, 20, 50, and 80 mg/ml, respectively, compared with Acyclovir was 80.4%. On the other hand, they were 21.1, 68.9, 75.3, and 76.4% for HSV2 with concentrations of 0, 20, 50, and 80 mg/ml, respectively, compared with Acyclovir at 87.9% (Table 2).
3.5 Mode of action
The possible mode of action for ON-0@SiO2, ON-1@SiO2, ON-2@SiO2, ON-3@SiO2, and Acyclovir may be investigated at three different levels: inhibition of viral replication, virucidal activity, and viral adsorption. Herein, the mode of action for the coconut oil-loaded silica nanoemulsion with different safe concentrations was illustrated for ON-0@SiO2, ON-1@SiO2, ON-2@SiO2, and ON-3@SiO2 (Fig. 5).
Percent inhibition for each mode of action is shown in Fig. 5. Interestingly, the results showed that the best mechanism of action for antiviral activity was the adsorption effect for ON-3@SiO2. ON-3@SiO2 had a combination of viral inhibitory effects on HSV1 and HSV2 at different viral stages. ON-3@SiO2 showed 68 and 63% virucidal results, indicating that it possibly acts directly on the virion, causing inactivation. Additionally, it showed 86 and 90% inhibitory effects during the viral adsorption stage. It indicated 62 and 67% inhibitory effects during the viral replication stage against HSV1 and HSV2, respectively. Furthermore, the ON-2@SiO2 exhibited a virucidal impact with a 66 and 62% viral inhibitory effect. Additionally, it showed 83 and 82% inhibitory effects during the viral adsorption stage. It indicated 50 and 61% inhibitory effects during the viral replication stage against HSV1 and HSV2, respectively. ON-1@SiO2 showed almost 37 and 40% inhibitory effects on virucidal and 49 and 51% virus adsorption. And 21 and 29 virus replications against HSV1 and HSV2, respectively. Conversely, ON-0@SiO2 displayed the virucidal effect with a 26 and 31% viral inhibitory effect, 50 and 48% virus adsorption, and 28 and 20 virus replications against HSV1 and HSV2, respectively. This result confirmed the results of the crystal violet assay, which gave IC50 equal 1.9 and 5.5 mg/ml for ON-3@SiO2, ON-0@SiO2, for HSV1, and 2.1 and 6.2 for HSV2, respectively (Table 3).
3.6 Evaluations of antimicrobial activity
Figure 6 clearly shows that the coconut oil showed an effect against both E. coli and B. subtilis at a concentration of 100 mg/ml, but it did not show any effect against P. aeruginosa, S. aureus, and C. albicans. Antimicrobial susceptibility tests were performed against bacterial and fungal strains to examine the antimicrobial activity of the synthesized ON-0@SiO2 and ON-3@SiO2. Firstly, ON-0@SiO2 showed a weak effect against only E. coli, S. aureus, and B. subtilis (Fig. 7). In contrast, ON-3@SiO2 showed the highest antimicrobial activity against all the tested bacteria and fungi with a dose-dependent manner of the following zone sizes: 27, 26, 17, and 0 mm for E. coli; 13, 11, 7, and 1 mm for P. aeruginosa; 12, 10, 1 and 0 mm for S. aureus; 27, 26, 23 and 21 mm for B. subtilis and 13, 10, 7 and 2 mm for C. albicans at concentrations 100, 50, 25 and 12.5 mg/ml, respectively. All strains responded to ON-3@SiO2 in a dose-dependent manner. As the concentration of ON-3@SiO2 was diluted, the size of the inhibition zone decreased significantly with all bacterial and fungal strains. Both E. coli and B. subtilis are more sensitive to ON-3@SiO2 than P. aeruginosa, S. aureus, and C. albicans. Negative control does not show any effect, while positive control showed a higher impact against gram-negative strains than gram-positive ones. The present study evaluated the MIC, MBC, and MFC of ON-3@SiO2 against several microorganisms. Generally, the MIC, MBC, and MFC values for the tested bacteria and fungi were found to be 3.12 to 25 mg/ml. The MIC against E. coli, P. aeruginosa, S. aureus, B. subtilis, and C. albicans were 25, 12.5, 25, 3.12, and 12.5 mg/ml, respect regarding MBC, all bacterial strains showed an MBC value of 25 mg/ml except for B. subtilis. Regarding MBC, all bacterial strains showed an MBC value of 25 mg/ml except for B. subtilis, which had an MBC value of 6.25 mg/ml. Also, C. albicans showed an MFC value of 25 mg/ml. All these findings are summarized in Tables 4 and 5 and Figs. 7, 8, and 9.
4 Discussion
Coconut oil contains several phyto-compounds with antiviral properties, as discovered by GC–MS research. Laurine, also known as monolaurin or 2-capri-1,3-di, is an ester of lauric acid and has been shown to be effective against lipid-enveloped viruses like influenza, HIV, and herpes simplex virus (HSV). It disrupts the lipid bilayer of the viral envelope, preventing viral growth and penetration into host cells [38]. Dodecyl gallate, also known as dodecyl cis-9,10-epoxyoctadecanoate, has shown antiviral efficacy against various viruses, including enteroviruses, hepatitis C virus (HCV), and herpes viruses. Its mechanism is believed to be interfering with glycoproteins used by the virus to bind to cell receptors [39]. Glycerol monolaurate, also known as glycerol monolaurate or monolaurin, has broad-spectrum antiviral action against enveloped viruses like HIV, HSV, and respiratory syncytial virus [40]. Notably, Furfural, also known as 2(3H)-Furanone, has antiviral properties against influenza, adenovirus, and HSV by inhibiting viral protein synthesis and replication.
Decanoic acid (DA) is a saturated medium- fatty acid, also known as capric acid [41]. Its antiviral properties are attributed to its ability to disrupt the lipid bilayer of the viral enveloped, similar to lauric acid and its derivative monolaurin. Decanoic acid has been studied for its potential antiviral effects, particularly against herpes simplex virus (HSV) and other lipid-enveloped viruses [42].
Virus mutations and bacterial antibiotic resistance are serious problems that are common worldwide, so most researchers try to solve this problem by discovering novel drugs [14, 43]. It is worth noting that HSV1 and HSV2 herpes viruses pose a significant risk to public health worldwide and can spread globally and start pandemics [22, 44]. The discovery of novel and potent anti-herpes medicines is urgently needed since the effectiveness of the present antiviral treatments against herpes is compromised by their severe side effects and the rising occurrence of drug-resistant strains during treatment [45]. Using nanoparticles for therapeutics has several benefits over traditional therapies, including potent antiviral efficacy against drug-resistant viruses, cost-effective manufacturing, and compatibility with various coating types [23, 46,47,48].
The MTT findings showed that coconut oil, ON-0@SiO2 and ON-3@SiO2 at concentrations up to 0, 20, 50, and 80 mg/ml did not cause cell death [49], and also our result indicated that according to the results of the cytotoxicity assay, the doses of 80, 50, and 20 mg/ml as different safe concentrations were selected to begin assays of plaque reduction for ON-0@SiO2 and ON-3@SiO2, both Human herpes HSV1 and HSV2 viruses’ propagation, as well as antibacterial and antifungal activities [50].
It is worth noting that HSV1 and HSV2 herpes viruses pose a significant risk to public health worldwide and can spread globally and start pandemics. The discovery of novel and potent anti-herpes medicines is urgently needed since the effectiveness of the present antiviral treatments against herpes is compromised by their severe side effects and the rising occurrence of drug-resistant strains during treatment [51,52,53]. Using nanoparticles for therapeutics has several benefits over traditional therapies, including potent antiviral efficacy against drug-resistant viruses, cost-effective manufacturing, and compatibility with various coating types [23, 46,47,48].
Generally, antiviral compounds inhibit the formation of new viruses by blocking crucial steps of viral replication or directly acting on the virus [54]. Understanding of the antiviral mechanism of action of nanoemulsion is therefore essential for target-oriented and efficient development of new antiviral strategies exploiting nanoparticles. Nevertheless, their antiviral mechanisms are still under investigation and seem to depend on the synthesis of nanoemulsion, with many factors such as size, shape and surface functionalization influencing the antiviral activity. This suggested that the nanoemulsion acted as an inhibitor as it emulated cellular receptors, or virus receptor inducing the virus to bind nanoemulsion. These nanoemulsions have been applied to an HSV inhibition test, but they potentially can be used to hinder other viruses, since functional groups present on the nanoemulsion surface and different basic materials can attract and inhibit different types of viruses [23].
Our results indicated that coconut oil-loaded silica nanoemulsion inhibited herpes viruses; additionally, nanoemulsion may decrease viral replications in host cells by blocking viral attachment on host cells. However, it has been proposed that the antiviral action of nanoemulsion is caused by two different processes that prevent viral replication: 1. nanoemulsion may interact with viral components and double-strand breaks when they traverse cell membranes. 2. Nanoemulsion can attach to sulfur-containing residues on the surface glycoproteins of viruses, preventing viral-host penetration and cell binding and leaving the virus in the extracellular space where it cannot spread [55,56,57,58]. Nano-loaded natural products have been recognized as a significant therapeutic approach within traditional medicine, particularly in addressing the worldwide pandemic and facilitating the recuperation of those afflicted with COVID-19 [59]. Numerous plants synthesize secondary metabolites and several other compounds as a defense mechanism against the intrusion of pathogens, including viruses. NEs have been shown to specifically target certain types of infections, while others effectively deliver active antivirals and vaccinations [60, 61]. According to previous studies [62, 63], it has been found that Leptospermum scoparium and Chamomilla essential oils and nanoemulsion have notable efficacy as antiviral agents specifically targeting the herpes simplex viruses HSV1 and HSV2, respectively.
Our results indicated that the coconut oil-loaded silica nanoemulsion has antiviral properties against HSV1 and 2, which prevent the virus from entering the cell by blocking the cell or virus receptors, so the high results appear in adsorption mode. Viruses are classified as a diminutive obligatory intracellular parasite. Extracellular virions facilitate the dissemination of these entities outside host cells, where they exist in an inert state. The interactions between the pathogen and the host cell mostly involve receptor-ligand interactions [64]. The antiviral properties of several natural items have demonstrated significant potential in inhibiting the entry of pathogenic viruses into cells and interacting with their pathogenicity [62]. Viral features, which are essential for the entrance into host cells or adsorption, might be either concealed or directly impeded to hinder viral infection [65, 66].
Despite the coconut oil having antimicrobial activity against many bacterial and fungal strains [67], it showed a weak effect on the isolates used compared to the positive control. Antimicrobial resistance pathways can be divided into four major groups as shown in Fig. 10. First, reducing medication uptake by gram-negative bacteria's lipopolysaccharide (LPS) layer [45]. Secondly, modifying a drug target, e.g., inhibiting cell wall synthesis, ribosomal mutation, inhibiting metabolic pathways via enzyme mutations, and modifying DNA gyrase or topoisomerase [68]. Thirdly, there are two main ways to inactivate a drug: by actual drug degradation or by adding a chemical group to the drug. Acetyl, phosphoryl, and adenyl groups are the most frequently added [69], or the drug is hydrolyzed by, e.g., β-lactamase [70]. Fourthly, active drug efflux [71]. Gram-negative bacteria use all four main mechanisms [72]. Our data showed that ON-0@SiO2 showed little effect on the tested strains; this may be due to the need for materials with potent activity against pathogenic bacteria in antibacterial treatments or surfaces may be the reason for this. Nude silica nanoparticles showed no detrimental effects on bacteria [73]. In contrast, all bacterial and fungal strains responded to ON-3@SiO2; this may be due to the energy held in the oil-and-detergent emulsion being released and destabilizing the lipid membrane, leading to the antibacterial activity of Nanoemulsions, which function by fusing with lipid bilayers of cell membranes. [74]. The tested bacteria and fungi are responsible for many surface and local infections, which need specific treatment for each condition, and contrary to antibiotics, Nanoemulsions antibacterial activity is nonspecific, allowing for broad-spectrum activity while reducing the development of resistance. Due to these characteristics, Nanoemulsion can treat wounds and clean surfaces [74].
5 Conclusion
Coconut oil-loaded silica nanoemulsion was prepared using Tween 60 as a surfactant and stabilizing agent. In addition, a high-speed homogenizer was used for dispersion. It was concluded that the nanoemulsions nominated as ON-1@SiO2 and ON-2@SiO2 were obtained with uniform distribution and spherical shape. The size of both nanoemulsions was around 200 nm. Our results showed that ON-3@SiO2 had promised as anti-HSV1 and HSV2 because the selective index is 51.3 and 42.4 and inhibition of them 76.0 and 76.4%. ON-3@SiO2 had a combination of viral inhibitory effects on HSV1 and HSV2 at different viral stages. it showed 86 and 90% inhibitory effects during the viral adsorption stage. On other hand, ON-3@SiO2 showed the highest antimicrobial activity against all the tested bacteria and fungi with a dose-dependent manner of the following zone sizes: 27, 26, 17, and 0 mm for E. coli; 13, 11, 7, and 1 mm for P. aeruginosa; 12, 10, 1 and 0 mm for S. aureus; 27, 26, 23 and 21 mm for B. subtilis and 13, 10, 7 and 2 mm for C. albicans at concentrations 100, 50, 25 and 12.5 mg/ml, respectively. However, the final formulation of coconut oil-loaded silica nanoemulsion exhibited significant activity against HSV1, HSV2, P. aeruginosa, C. albicans, B. subtilis, and E. coli, and it could be new antiviral, antibacterial, and antifungal agents with significant potential usage in both wound treatment and surface decontamination.
Availability of data and materials
Not applicable.
Abbreviations
- MTT:
-
3-(4, 5-Dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide
- ACV:
-
Acyclovir
- CLSI:
-
Clinical and Laboratory Standards Institute
- CO:
-
Coconut oil
- ON@SiO2 :
-
Coconut oil-loaded silica nanoemulsion
- CFU:
-
Colony-forming unit
- CC:
-
Cytotoxicity concentration
- DW:
-
Distilled water
- DMEM:
-
Dulbecco’s modified eagle’s medium
- ELISA:
-
Enzyme-linked immunosorbent assay
- FBS:
-
Fetal bovine serum
- GC–MS:
-
Gas chromatography–mass spectrometry analysis
- HCV:
-
Hepatitis C virus
- HSV:
-
Herpes virus
- HIV:
-
Human immunodeficiency virus
- IC:
-
Inhibitory concentration
- LPS:
-
Lipopolysaccharide
- MDCK:
-
Madin–Darby canine kidney
- MBC:
-
Minimum bactericidal concentration
- MFC:
-
Minimum fungicidal concentration
- MIC:
-
Minimum inhibitory concentration
- MHA:
-
Muller–Hinton agar
- MDR:
-
Multidrug-resistant
- NEs:
-
Nanoemulsions
- nm:
-
Nanometer
- NCCLS:
-
National Committee for Clinical Laboratory Standards
- NC:
-
Negative control
- ON:
-
Oil nanoemulsion
- PCV:
-
Penciclovir
- PBS:
-
Phosphate-buffered saline
- PFU:
-
Plaque forming unit
- PC:
-
Positive control
- RT:
-
Room temperature
- SDA:
-
Sabouraud agar
- TEOS:
-
Tetraethyl orthosilicate
- TEM:
-
Transmission electron microscopy
- WHO:
-
World Health Organization
References
Collaborators AR (2022) Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 399(10325):629–655. https://doi.org/10.1016/S0140-6736(21)02724-0
Memariani H, Memariani M, Shahidi-Dadras M, Nasiri S, Akhavan MM, Moravvej H (2019) Melittin: from honeybees to superbugs. Appl Microbiol Biotechnol 103:3265–3276. https://doi.org/10.1007/s00253-019-09698-y
Sumarny R, Rahayu L, Sandhiutami NMD, LM, (2013) Efek Stimulansia Infus Lada Hitam (Piperis nigri fructus) pada Mencit. J Ilmu Kefarmasian Indones 11:142–146
Nevin KG, Rajamohan T (2004) Beneficial effects of virgin coconut oil on lipid parameters and in vitro LDL oxidation. Clin Biochem 37:830–835. https://doi.org/10.1016/j.clinbiochem.2004.04.010
Bergsson G, Arnfinnsson J, Steingrimsson O, Thormar H (2001) Killing of Gram-positive cocci by fatty acids and monoglyceridesNote. APMIS 109:670–678. https://doi.org/10.1034/j.1600-0463.2001.d01-131.x
de Oliveira SF, Lôbo IP, da Cruz RS, Andrioli JL, da Mata CPSM, Soares GA, Santos E, do C, Aguiar-Oliveira E, Franco M, da Conceição AO, (2018) Antimicrobial activity of coconut oil-in-water emulsion on Staphylococcus epidermidis and Escherichia coli EPEC associated to Candida kefyr. Heliyon. https://doi.org/10.1016/j.heliyon.2018.e00924
Marhamati M, Ranjbar G, Rezaie M (2021) Effects of emulsifiers on the physicochemical stability of Oil-in-water Nanoemulsions: a critical review. J Mol Liq 340:117218. https://doi.org/10.1016/j.molliq.2021.117218
Wilson RJ, Li Y, Yang G, Zhao C-X (2022) Nanoemulsions for drug delivery. Particuology 64:85–97. https://doi.org/10.1016/j.partic.2021.05.009
Tiwari U, Ganesan NG, Junnarkar J, Rangarajan V (2022) Toward the formulation of bio-cosmetic nanoemulsions: from plant-derived to microbial-derived ingredients. J Dispers Sci Technol 43:1061–1078. https://doi.org/10.1080/01932691.2020.1847664
Jamali SN, Assadpour E, Feng J, Jafari SM (2021) Natural antimicrobial-loaded nanoemulsions for the control of food spoilage/pathogenic microorganisms. Adv Colloid Interface Sci 295:102504. https://doi.org/10.1016/j.cis.2021.102504
Al Saihati HA, Hussein HAM, Thabet AA, Wardany AA, Mahmoud SY, Farrag ES, Mohamed TIA, Fathy SM, Elnosary ME, Sobhy A, Ahmed AE, El-Adly AM, El-Shenawy FS, Elsadek AA, Rayan A, Zahran ZAM, El-Badawy O, El-Naggar MGM, Afifi MM, Zahran AM (2023) Memory T cells discrepancies in COVID-19 patients. Microorganisms 11:2737. https://doi.org/10.3390/microorganisms11112737
Kaur P, Gupta S, Kaur K, Kaur N, Kumar R, Bhullar MS (2021) Nanoemulsion of Foeniculum vulgare essential oil: a propitious striver against weeds of Triticum aestivum. Ind Crops Prod 168:113601. https://doi.org/10.1016/j.indcrop.2021.113601
Tayeb HH, Felimban R, Almaghrabi S, Hasaballah N (2021) Nanoemulsions: formulation, characterization, biological fate, and potential role against COVID-19 and other viral outbreaks. Colloids Interface Sci Commun 45:100533. https://doi.org/10.1016/j.colcom.2021.100533
Irwin KK, Renzette N, Kowalik TF, Jensen JD (2016) Antiviral drug resistance as an adaptive process. Virus Evol 2:vew014. https://doi.org/10.1093/ve/vew014
Phan T (2020) Genetic diversity and evolution of SARS-CoV-2. Infect Genet Evol 81:104260
Lysenko V, Lozovski V, Lokshyn M, Gomeniuk YV, Dorovskih A, Rusinchuk N, Pankivska Y, Povnitsa O, Zagorodnya S, Tertykh V, Bolbukh Y (2018) Nanoparticles as antiviral agents against adenoviruses. Adv Nat Sci Nanosci Nanotechnol 9:25021. https://doi.org/10.1088/2043-6254/aac42a
Lozovski VZ, Lysenko VS, Rusinchuk NM (2020) Near-field interaction explains features of antiviral action of non-functionalized nanoparticles. Adv Nat Sci Nanosci Nanotechnol 11:15014. https://doi.org/10.1088/2043-6254/ab7910
Gaikwad S, Ingle A, Gade A, Rai M, Falanga A, Incoronato N, Russo L, Galdiero S, Galdiero M (2013) Antiviral activity of mycosynthesized silver nanoparticles against herpes simplex virus and human parainfluenza virus type 3. Int J Nanomed 8:4303–4314. https://doi.org/10.2147/IJN.S50070
Koelle DM, Corey L (2008) Herpes simplex: insights on pathogenesis and possible vaccines. Annu Rev Med 59:381–395. https://doi.org/10.1146/annurev.med.59.061606.095540
Elnosary ME, Aboelmagd HA, Habaka MA, Salem SR, El-Naggar ME (2023) Synthesis of bee venom loaded chitosan nanoparticles for anti-MERS-COV and multi-drug resistance bacteria. Int J Biol Macromol 224:871–880. https://doi.org/10.1016/j.ijbiomac.2022.10.173
Herpes simplex Retrieved June 3, 2023, from https://www.who.int/news-room/fact-sheets/detail/herpes-simplex-virus
Field HJ, Biswas S (2011) Antiviral drug resistance and helicase-primase inhibitors of herpes simplex virus. Drug Resist Updat 14:45–51. https://doi.org/10.1016/j.drup.2010.11.002
Elnosary M, Aboelmagd H, Sofy M, Sofy A, Elshazly E (2022) Antiviral and antibacterial properties of synthesis silver nanoparticles with Nigella arvensis aqueous extract. Egypt J Chem. https://doi.org/10.21608/ejchem.2022.159976.6894
Almuhayawi MS, Alruhaili MH, Gattan HS, Alharbi MT, Nagshabandi M, Al JS, Selim S, Alanazi A, Alruwaili Y, Faried OA, Elnosary ME (2023) Staphylococcus aureus induced wound infections which antimicrobial resistance, methicillin-and vancomycin-resistant: assessment of emergence and cross sectional study. Infect Drug Resist 16:5335–5346. https://doi.org/10.2147/IDR.S418681
Hwang YY, Ramalingam K, Bienek DR, Lee V, You T, Alvarez R (2013) Antimicrobial activity of nanoemulsion in combination with cetylpyridinium chloride in multidrug-resistant acinetobacter baumannii. Antimicrob Agents Chemother 57:3568–3575. https://doi.org/10.1128/AAC.02109-12
Kutkat O, Moatasim Y, Al-Karmalawy AA, Abulkhair HS, Gomaa MR, El-Taweel AN, Abo Shama NM, GabAllah M, Mahmoud DB, Kayali G, Ali MA, Kandeil A, Mostafa A (2022) Robust antiviral activity of commonly prescribed antidepressants against emerging coronaviruses: in vitro and in silico drug repurposing studies. Sci Rep 12:12920. https://doi.org/10.1038/s41598-022-17082-6
Mahmoud A, Kotb E, Alqosaibi AI, Al-Karmalawy AA, Al-Dhuayan IS, Alabkari H (2021) In vitro and in silico characterization of alkaline serine protease from Bacillus subtilis D9 recovered from Saudi Arabia. Heliyon. https://doi.org/10.1016/j.heliyon.2021.e08148
Kandeil A, Mostafa A, Kutkat O, Moatasim Y, Al-Karmalawy AA, Rashad AA, Kayed AE, Kayed AE, El-Shesheny R, Kayali G, Ali MA (2021) bioactive polyphenolic compounds showing strong antiviral activities against severe acute respiratory syndrome coronavirus 2. Pathogens 10:758. https://doi.org/10.3390/pathogens10060758
Abo Elmaaty A, Eldehna WM, Khattab M, Kutkat O, Alnajjar R, El-Taweel AN, Al-Rashood ST, Abourehab MAS, Binjubair FA, Saleh MA, Belal A, Al-Karmalawy AA (2022) Anticoagulants as potential SARS-CoV-2 Mpro inhibitors for COVID-19 patients: in vitro, molecular docking, molecular dynamics, DFT, and SAR studies. Int J Mol Sci 23:12235. https://doi.org/10.3390/ijms232012235
Alnajjar R, Mostafa A, Kandeil A, Al-Karmalawy AA (2020) Molecular docking, molecular dynamics, and in vitro studies reveal the potential of angiotensin II receptor blockers to inhibit the COVID-19 main protease. Heliyon. https://doi.org/10.1016/j.heliyon.2020.e05641
Abouaitah K, Allayh AK, Wojnarowicz J, Shaker YM, Swiderska-Sroda A, Lojkowski W (2021) Nanoformulation composed of ellagic acid and functionalized zinc oxide nanoparticles inactivates dna and rna viruses. Pharmaceutics 13:2174. https://doi.org/10.3390/pharmaceutics13122174
Ahmed HB, El-Shahat M, Allayeh AK, Emam HE (2023) Maillard reaction for nucleation of polymer quantum dots from chitosan-glucose conjugate: antagonistic for cancer and viral diseases. Int J Biol Macromol 224:858–870. https://doi.org/10.1016/j.ijbiomac.2022.10.172
Daoud A, Malika D, Bakari S, Hfaiedh N, Mnafgui K, Kadri A, Gharsallah N (2019) Assessment of polyphenol composition, antioxidant and antimicrobial properties of various extracts of Date Palm Pollen (DPP) from two Tunisian cultivars. Arab J Chem 12:3075–3086. https://doi.org/10.1016/j.arabjc.2015.07.014
Ben HA, Trigui M, Ben MR, Jarraya RM, Damak M, Jaoua S (2011) Chemical composition, cytotoxicity effect and antimicrobial activity of Ceratonia siliqua essential oil with preservative effects against Listeria inoculated in minced beef meat. Int J Food Microbiol 148:66–72. https://doi.org/10.1016/j.ijfoodmicro.2011.04.028
NCCLS/CLSI (2007) National Committee for Clinical Laboratory Standards/ Clinical and Laboratory Standards Institute: Performance standards for antimicrobial susceptibility testing; Seventeenth informational supplement, M2-A9 and M7-A7. Wayne, PA, USA
Humphries RM, Ambler J, Mitchell SL, Castanheira M, Dingle T, Hindler JA, Koeth L, Sei K (2023) Erratum for Humphries et al., “CLSI Methods Development and Standardization Working Group Best Practices for Evaluation of Antimicrobial Susceptibility Tests.” J Clin Microbiol 61:e0073923. https://doi.org/10.1128/jcm.00739-23
de Lemos J, A, Costa CR, Araújo CR de, Souza LKH, Silva M do RR, (2009) Susceptibility testing of Candida albicans isolated from oropharyngeal mucosa of HIV+ patients to fluconazole, amphotericin B and Caspofungin: killing kinetics of caspofungin and amphotericin B against fluconazole resistant and susceptible isolates. Braz J Microbiol 40:163–169. https://doi.org/10.1590/S1517-83822009000100028
Wallace TC (2019) Health Effects of coconut oil—a narrative review of current evidence. J Am Coll Nutr 38:97–107. https://doi.org/10.1080/07315724.2018.1497562
Govea-Salas M, Rivas-Estilla AM, Rodríguez-Herrera R, Lozano-Sepúlveda SA, Aguilar-Gonzalez CN, Zugasti-Cruz A, Salas-Villalobos TB, Morlett-Chávez JA (2016) Gallic acid decreases hepatitis C virus expression through its antioxidant capacity. Exp Ther Med 11:619–624. https://doi.org/10.3892/etm.2015.2923
Welch JL, Xiang J, Okeoma CM, Schlievert PM, Stapleton JT (2020) Glycerol monolaurate, an analogue to a factor secreted by lactobacillus, is virucidal against enveloped viruses, including hiv-1. MBio 11:10–1128. https://doi.org/10.1128/mBio.00686-20
Dasgupta S, Bhattacharyya DK (2009) Dietary effect of capric acid containing soyphospholipids. J Oleo Sci 58:395–401. https://doi.org/10.5650/jos.58.395
Nitbani FO, Tjitda PJP, Nitti F, Jumina J, Detha AIR (2022) Antimicrobial properties of lauric acid and monolaurin in virgin coconut oil: a review. ChemBioEng Rev 9:442–461. https://doi.org/10.1002/cben.202100050
Schroder K, Hertzog PJ, Ravasi T, Hume DA (2004) Interferon-γ: an overview of signals, mechanisms and functions. J Leukoc Biol 75:163–189. https://doi.org/10.1189/jlb.0603252
Donalisio M, Nana HM, Ngono Ngane RA, Gatsing D, Tiabou Tchinda A, Rovito R, Cagno V, Cagliero C, Boyom FF, Rubiolo P, Bicchi C, Lembo D (2013) In vitro anti-herpes simplex virus activity of crude extract of the roots of nauclea latifolia smith (rubiaceae). BMC Complement Altern Med 13:1–8. https://doi.org/10.1186/1472-6882-13-266
Almuhayawi MS, Gattan HS, Alruhaili MH, Alharbi MT, Nagshabandi MK, Tarabulsi MK, Almuhayawi SM, Al Jaouni SK, Selim S, Alanazi A, Alruwaili Y, Faried OA, Amin I, Elnosary ME (2023) Molecular profile and the effectiveness of antimicrobials drugs against staphylococcus aureus and pseudomonas aeruginosa in the diagnostic approaches of otitis infection. Infect Drug Resist 16:4397–4408. https://doi.org/10.2147/IDR.S418685
Esghaei M, Monavari SHR, Tavassoti-Kheiri M, Shamsi-Shahrabadi M, Heydarchi B, Farahmand B, Saleh M, Fotouhi F (2012) Expression of the influenza M2 protein in three different eukaryotic cell lines. J Virol Methods 179:161–165. https://doi.org/10.1016/j.jviromet.2011.10.016
ZeinEldin RA, Ahmed MM, Hassanein WS, Elshafey N, Sofy AR, Hamedo HA, Elnosary ME (2023) Diversity and distribution characteristics of viruses from soda lakes. Genes (Basel) 14:323. https://doi.org/10.3390/genes14020323
Elshazly EH, Nasr A, Elnosary ME, Gouda GA, Mohamed H, Song Y (2023) Identifying the anti-MERS-CoV and anti-HcoV-229E potential drugs from the ginkgo biloba leaves extract and its eco-friendly synthesis of silver nanoparticles. Molecules 28:1375. https://doi.org/10.3390/molecules28031375
Hosny KM, Alhakamy NA, Sindi AM, Khallaf RA (2020) Coconut oil nanoemulsion loaded with a statin hypolipidemic drug for management of burns: formulation and in vivo evaluation. Pharmaceutics 12:1–16. https://doi.org/10.3390/pharmaceutics12111061
Tubtimsri S, Limmatvapirat C, Limsirichaikul S, Akkaramongkolporn P, Inoue Y, Limmatvapirat S (2018) Fabrication and characterization of spearmint oil loaded nanoemulsions as cytotoxic agents against oral cancer cell. Asian J Pharm Sci 13:425–437. https://doi.org/10.1016/j.ajps.2018.02.003
Makau JN, Watanabe K, Mohammed MMD, Nishida N (2018) Antiviral activity of peanut (Arachis hypogaea L.) skin extract against human influenza viruses. J Med Food 21:777–784. https://doi.org/10.1089/jmf.2017.4121
Hussein HAM, Thabet AAA, Mohamed TIA, Elnosary ME, Sobhy A, El-Adly AM, Wardany AA, Bakhiet EK, Afifi MM, Abdulraouf UM, Fathy SM, Sayed NG, Zahran AM (2023) Phenotypical changes of hematopoietic stem and progenitor cells in COVID-19 patients: Correlation with disease status. Cent Eur J Urol 48:97–110. https://doi.org/10.5114/ceji.2023.129981
Selim S, Albqmi M, Alanazi A, Alruwaili Y, Al-Sanea MM, Alnusaire TS, Almuhayawi MS, Al Jaouni SK, Hussein S, Warrad M, AbdElgawad H, Elshafey N, Elnosary ME (2023) Antiviral activities of olive oil apigenin and taxifolin against SARS-CoV-2 RNA-dependent RNA polymerase (RdRP): in silico, pharmacokinetic, ADMET, and in-vitro approaches. Cogent Food Agric 9:2236828. https://doi.org/10.1080/23311932.2023.2236828
Gonçalves BC, Lopes Barbosa MG, Silva Olak AP, Belebecha Terezo N, Nishi L, Watanabe MA, Marinello P, Zendrini Rechenchoski D, Dejato Rocha SP, Faccin-Galhardi LC (2021) Antiviral therapies: advances and perspectives. Fundam Clin Pharmacol 35:305–320. https://doi.org/10.1111/fcp.12609
Camero M, Lanave G, Catella C, Capozza P, Gentile A, Fracchiolla G, Britti D, Martella V, Buonavoglia C, Tempesta M (2019) Virucidal activity of ginger essential oil against caprine alphaherpesvirus-1. Vet Microbiol 230:150–155. https://doi.org/10.1016/j.vetmic.2019.02.001
Hammami S, Jmii H, Mokni R, Khmiri A, Faidi K, Dhaouadi H, Aouni M, Aouni M, Joshi R (2015) Essential oil composition, antioxidant, cytotoxic and antiviral activities of Teucrium pseudochamaepitys growing spontaneously in Tunisia. Molecules 20:20426–20433. https://doi.org/10.3390/molecules201119707
Mun H, Townley HE (2021) Nanoencapsulation of plant volatile organic compounds to improve their biological activities. Planta Med 87:236–251. https://doi.org/10.1055/a-1289-4505
Tariq S, Wani S, Rasool W, Shafi K, Bhat MA, Prabhakar A, Shalla AH, Rather MA (2019) A comprehensive review of the antibacterial, antifungal and antiviral potential of essential oils and their chemical constituents against drug-resistant microbial pathogens. Microb Pathog 134:103580. https://doi.org/10.1016/j.micpath.2019.103580
Ahmadi R, Salari S, Sharifi MD, Reihani H, Rostamiani MB, Behmadi M, Taherzadeh Z, Eslami S, Rezayat SM, Jaafari MR, Elyasi S (2021) Oral nano-curcumin formulation efficacy in the management of mild to moderate outpatient COVID-19: A randomized triple-blind placebo-controlled clinical trial. Food Sci Nutr 9:4068–4075. https://doi.org/10.1002/fsn3.2226
Wang SH, Chen J, Smith D, Cao Z, Acosta H, Fan Y, Ciotti S, Fattom A, Baker J (2020) A novel combination of intramuscular vaccine adjuvants, nanoemulsion and CpG produces an effective immune response against influenza A virus. Vaccine 38:3537–3544. https://doi.org/10.1016/j.vaccine.2020.03.026
Zhang J, Miao J, Han X, Lu Y, Deng B, Lv F, Zhao Y, Ding C, Hou J (2018) Development of a novel oil-in-water emulsion and evaluation of its potential adjuvant function in a swine influenza vaccine in mice. BMC Vet Res 14:1–11. https://doi.org/10.1186/s12917-018-1719-2
Ulanowska M, Olas B (2021) Biological properties and prospects for the application of eugenol—a review. Int J Mol Sci 22:3671. https://doi.org/10.3390/ijms22073671
Elshamy AI, El-Kashak WA, Taher RF, Elghonemy MM, Ahmed RF, Mohamed TA, Essa AF, Ragab TIM, Abdelhameed MF, El-Gendy AE-NG, Nassar MI, Abd-ELGawad AM, Farrag ARH, Abd-Alla HI, Hegazy M-EF (2023) Uses of nanoemulsions in pharmaceuticals industries. In: Current trends in green nano-emulsions: food, agriculture and biomedical sectors. Springer, pp 263–297
Zhong P, Agosto LM, Munro JB, Mothes W (2013) Cell-to-cell transmission of viruses. Curr Opin Virol 3:44–50. https://doi.org/10.1016/j.coviro.2012.11.004
Asaad GF, Abdelhameed MF, El Raey MA, Roshdy WH, Elgamal AM, Moemen YS (2022) Citrus clementine peels essential oil exhibited anti-SARS-CoV-2 and its modulatory effect against cytokine storm: evidence from in vitro and in silico studies. Egypt J Chem 65:419–427. https://doi.org/10.21608/EJCHEM.2022.116657.5271
Astani A, Schnitzler P (2014) Antiviral activity of monoterpenes beta-pinene and limonene against herpes simplex virus in vitro. Iran J Microbiol 6:149–155
Kabara JJ (1978) Fatty acids and derivatives as antimicrobial agents-a review. Pharmacol Eff lipids
Bhatia P, Sharma A, George AJ, Anvitha D, Kumar P, Dwivedi VP, Chandra NS (2021) Antibacterial activity of medicinal plants against ESKAPE: an update. Heliyon. https://doi.org/10.1016/j.heliyon.2021.e06310
Blair JMA, Richmond GE, Piddock LJV (2014) Multidrug efflux pumps in gram-negative bacteria and their role in antibiotic resistance. Future Microbiol 9:1165–1177. https://doi.org/10.2217/FMB.14.66
Bush K, Bradford PA (2016) β-lactams and β-lactamase inhibitors: an overview. Cold Spring Harb Perspect Med 6:a025247. https://doi.org/10.1101/cshperspect.a025247
Villagra NA, Fuentes JA, Jofré MR, Hidalgo AA, García P, Mora GC (2012) The carbon source influences the efflux pump-mediated antimicrobial resistance in clinically important Gram-negative bacteria. J Antimicrob Chemother 67:921–927. https://doi.org/10.1093/jac/dkr573
Mahon CR, Mt MS, Lehman DC (2022) Textbook of diagnostic microbiology-e-book. Elsevier Health Sciences
Camporotondi DE, Foglia ML, Alvarez GS, Mebert AM, Diaz LE, Coradin T, Desimone MF (2013) Antimicrobial properties of silica modified nanoparticles. Microb Pathog Strateg Combat them Sci Technol Educ 2:283–290
Dolgachev VA, Ciotti SM, Eisma R, Gracon S, Wilkinson JE, Baker JR, Hemmila MR (2016) Nanoemulsion therapy for burn wounds is effective as a topical antimicrobial against Gram-negative and Gram-positive bacteria. J Burn Care Res 37:e104–e114. https://doi.org/10.1097/BCR.0000000000000217
Acknowledgements
Not applicable.
Funding
The authors declare that they had no funding for the present research.
Author information
Authors and Affiliations
Contributions
M. E. Elnosary; H. A. Aboelmagd; A. R. Sofy; A. A. Hmed, E.E. Refaey; S. M. Ali; and M. Abdel Hady contributed to the study of conception and design. Material preparation, data collection and analysis were performed by M. E. Elnosary; H. A. Aboelmagd; and Mayssa Abdel Hady. The first draft of the manuscript was written by M. E. Elnosary; H. A. Aboelmagd; and Mayssa Abdel Hady and M. E. Elnosary; H. A. Aboelmagd; A. R. Sofy; A. A. Hmed, E. E. Refaey; S. M. Ali; and M. Abdel Hady commented on previous versions of the manuscript. M. E. Elnosary; H. A. Aboelmagd; A. R. Sofy; A. A. Hmed, E. E. Refaey; S. M. Ali; and M. Abdel Hady read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elnosary, M.E., Aboelmagd, H.A., Sofy, A.R. et al. Uncovering and evaluating coconut oil-loaded silica nanoemulsion as anti-viral, bacterial, and fungal: synthesis, fabrication, characterization, and biosafety profiles. Beni-Suef Univ J Basic Appl Sci 13, 56 (2024). https://doi.org/10.1186/s43088-024-00513-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43088-024-00513-w