Abstract
Background
Ultrasound guidance for renal access in percutaneous nephrolithotomy (PCNL) is a safe, effective, and low-cost procedure. The current study compared the safety and effectiveness of ultrasound-guided PCNL (US-PCNL) for renal stone therapy versus fluoroscopy-guided PCNL (FL-PCNL) in prone position.
Results
Successful puncture was attained in all cases in both groups. Unlike fluoroscopy, US guidance reduced the time needed for achieving renal puncture that was (22.45 ± 6.95 s) compared to fluoroscopy that was (68.28 ± 56.76 s) (P value < 0.001). The mean duration of access that was reported in our study was (3.92 ± 0.72 min) in the US-PCNL group and (4.03 ± 0.77 min) in the FL-PCNL group (P value 0.460). There was no significant difference in the total operative time between both groups in our study as the mean operative time in the US-PCNL group was (61.47 ± 6.07 min) and (65.86 ± 20.86 min) in the FL-PCNL group with a (P value of 0.349). Stone-free rate was nearly similar in both groups (P value 0.336). Three cases in our study in the FL-PCNL group had bleeding that required blood transfusion post-operative; mean Hb change was 0.23 g/dL and 0.55 g/dL in US-PCNL and FL-PCNL groups, respectively, which is clinically irrelevant despite statistical significance (P value 0.007). Mean fluoroscopy time was (6.38 ± 3.84) minutes in FL-PCNL group.
Conclusion
Ultrasound guidance is a reliable tool in the hands of experienced urologists in performing PCNL with less or even zero radiation.
Similar content being viewed by others
1 Background
Renal stones represent a major health issue globally and are a problem in both genders at any age [1]. It is estimated that 12% of the world's population are expected to have renal stones affecting all races, sexes, and ages, but males are more likely than women in the age between 20 and 49 years [2]. Stone treatment tools are extracorporeal shock wave lithotripsy (ESWL), flexible ureteroscopy (URS), and PCNL. Stone burden, composition, and renal collecting system complexity all influence these decisions. PCNL is one of the best modalities in large stone burden and is conducted using X-rays, ultrasonic waves, or both [3]. Since the conventional PCNL is done under fluoroscopy guiding renal puncture, guidewire insertion, ureteral dilatation, and stone extraction, radiation exposure increases [4]. Putting patients and medical personnel alike at risk of oncogenesis and genetic mutation by the high levels of ionizing radiation, they are subjected to during FL-PCNL [5, 6]. US-PCNL prioritizes “as low as reasonably achievable” (ALARA) risk levels [5]. The International Commission on Radiation Protection (ICRP) recommends 150 mSv for the lens of the eye, 500 mSv for the skin, and 500 mSv for the extremities as the yearly equivalent dose limit. Ultrasound instead of fluoroscopy during PCNL should be promoted to limit this increasing amount of radiation exposure [6].
X-ray side effects including genetic abnormalities and cancer are not dose dependent [7, 8]. Despite contemporary fluoroscopes and shielding, radiation exposure remains a concern. So, many authors emphasize that radiation-free US-PCNL replaces or be an adjunct to FL-PCNL [9]. Also, the use of contrast agents in FL-PCNL has the risk of exposing patients to allergic reactions or contrast nephropathy [10]. On the other hand, renal US no-radiation, fast, affordable, bedside technique does not involve any invasive procedures. It has the ability to detect hydronephrosis, ureteral dilatation, kidney size, thickness, stones, and parenchymal morphology (echogenicity, corticomedullary differentiation, cortical cysts) with great accuracy and instantly [11]. Hence diagnostic needs and plan of management can be determined promptly [12]. The current study compared the safety, effectiveness, and practicality of US-PCNL for renal stone therapy to FL-PCNL.
2 Patients and methods
2.1 Participants and study groups
Between August 2020 and July 2022, a prospective randomized study was conducted in the urology department at our university hospital, with an estimated minimum sample size of 84 participants for 95% power, error probability 0.05, and 10% dropout rate during follow-up. Patients were randomly assigned to one of two treatment groups using a computer-generated sequence: either an US-PCNL group of 51 patients or a FL-PCNL group of 50 patients. Adult patients between 18 and 70 years were included if they had a renal stone greater than 1 cm in diameter and an American Society of Anesthesia score (ASA) of 2 or below. Patients with renal abnormalities, kidney transplants, uncorrected coagulopathy, or active infection were excluded; Fig. 1 shows consort flowchart of the studied cases.
2.2 Methods
2.2.1 Data collection
Preoperatively, patients’ age, sex, and ASA health status were obtained. Ultrasound and non-contrast CT scan and Guy's stone score were done for all patients. The stone load was calculated using the total stone size.
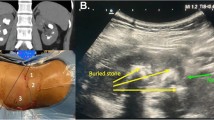
Surgical technique All patients underwent prone PCNL. In FL-PCNL, a movable multi-directional C-arm fluoroscopy equipment with an under-table X-ray generator was employed for imaging. It was used. Total screening time was measured by the fluoroscopy equipment. Estimated blood loss and total operating time were also documented. In the US-PCNL group, a [3.5–6 MHz] convex abdominal ultra-sound transducer (BK Medical, USA) was employed. The probe was held in a way to permit visualizing the whole kidney in the longitudinal plane, being parallel to the ribs to avoid acoustic shadow from obscuring the view. Identify posterior calyces and choose entrance calyx using an 18-gauge, 20-cm renal access needle. The needle enters the skin 1 cm from the caudal end of the probe for lower pole punctures and 1 cm from the cephalad end for upper pole punctures. The ultrasound monitor should show the needle as it penetrates the skin, traverses the subcutaneous, fascial, muscular, and perinephric layers, enters the kidney, and enters the targeted calyx in the longitudinal view. Maintaining the longitudinal view and fanning the ultrasonic probe back and forth helps re-direct the needle into the right plane relative to the targeted calyx. Once in the collecting system, removing the needle stylet allows seeing urine outflow or aspiration to check needle tip location. The needle stylet is removed to pass a J-tip coaxial guide wire through the access needle. Gently moving the guiding wire forward and backward locates the tip and collecting system. This jiggling action under ultrasound supervision shows its exact location.
The access needle is removed over the guide wire, and a skin incision is created. Using a balloon device (nephromax) or Amplatz dilator dilation, the functioning tract is created, and percutaneous access sheath is carefully advanced over the dilator. The sheath advanced until the back end of the balloon can be seen through the external sheath in balloon dilation or until the distance into the renal pelvi-calyceal system is measured in case of Amplatz dilators. The FL-PCNL group used monoplanar needle puncture under fluoroscopic supervision. The two methods followed the same processes after puncturing the target calyx. The FL-PCNL group exclusively employed fluoroscopy for future phases. An appropriate sheath is glided over the dilator into the chosen calyx under US or fluoroscopy, depending on the group. Ballistic (pneumatic) lithotripters fragmented stone. A Foley catheter was inserted after fixation of a JJ stent or a ureteric catheter depending on the demanding circumstances in each procedure. Later on-table check antegrade pyelography determined JJ stent and PCN placements.
Post-operative outcomes Hematocrit change, blood transfusion, SFR, complications, and hospital stay were noted.
2.2.2 Statistical analysis
SPSS version 25 for Windows 10 was used to code, input, and analyse the data. Data normality was tested using Kolmogorov–Smirnov. Description of qualitative findings is as a percentage distribution and quantitative results as minimum, maximum, mean, and standard deviation. Use cross-tabulation and Chi-square test (χ2) to compare category variables and percentage values. The Student t test compares the means of two unrelated groups with a normal distribution. Paired sample t test compares pre- and post-operative means of two related groups with normal distributions. Statistically significant P values were 0.05 or less.
3 Results
Both groups were comparable regarding demographic and stone data with an average age of 38.61 ± 13.38 years, male to female ratio (P values < 0.357 and 0.180), respectively, pre-operative stone side, previous renal stone surgery, hydronephrosis grade, stone site, Guy’s score, stone size and stone density, without statistically significant differences (P values > 0.05), Table 1. Most cases required a single-puncture attempt in both groups apart from 29 patients in the FL-PCNL group who required additional attempts. All patients required a single lower calyceal puncture apart from 5 patients in the FL-PCNL group required additional middle calyceal puncture and two patients required additional upper calyceal puncture, Table 2. The puncture time, haemoglobin change, and radiation exposure time were lower in US-PCNL group showing high statistical significance (P values < 0.001) without significant differences between both groups in the access time, stone-free rate, and operative time, Table 3 and Fig. 2. The incidence of complication according to the modified Clavien–Dindo classification in the FL-PCNL group was bleeding that required blood transfusion in three patients (grade II) with (P value 0.118) which denotes statistically non-significant value but clinically significant and 3 patients that experienced extravasation and were managed by JJ stent placement (grade II) in contrast to one patient experienced post-operative fever in US-PCNL group (grade 1) that was controlled with parenteral antibiotics and antipyretics (P value 0.114), Figure 3.
4 Discussion
Urologists, surgical assistants, nurses, and patients are exposed to cumulative radiation during FL-PCNL. To avoid hazards of ionized radiation the best solution is to use US-PCNL [8, 13]. This study evaluated both procedures’ safety and efficacy. As regards fluoroscopy time, few designed studies have compared zero radiation PCNL vs conventional PCNL as most trials used ultrasonography for the puncture and used additional fluoroscopy for the tract formation as in Elhashash and associate, where the mean time of radiation exposure was 11.06 min in FL-PCNL, whereas ultrasound procedures expose them for 5.32 min (P = 0.002). Also, Jagtap and associate reported less radiation exposure when ultrasound was used with fluoroscopy time (239.9 ± 77.5 s) in the C-PCNL compared with (204.3 ± 84 s) in the US-PCNL group, respectively (P value 0.04) [14, 15]. In our study the US-PCNL was zero exposure to fluoroscopy, while in the FL-PCNL the mean time of radiation exposure was 6.38 min (range from 2 to 16.34 min). In Kumari and associate the mean time of radiation was 6.04 min (range 1.8–12.16 min) and 10.42 min in reports of Lipkin and associate (compared to 0 min in the US-PCNL group) [5, 6].
One of these parameters was the number of puncture trials needed which were 1.7 trials in FL-PCNL in contrast to US-PCNL patients were punctured on the first trial in 100% of patients (P value < 0.001). A study of Agarwall and associate fluoroscopic puncture required 3.3 trials, whereas US puncture only 1.5 trials (P value 0.01) [16] and in Jagtap and associate a mean of 1.7 ± 0.9 trials US-PCNL versus 1.6 ± 0.8 trials in FL-PCNL (P value 0.33) [15].
Basiri and associate reported a 94% success rate with US-PCNL and a 90% success rate with FL-PCNL (P value 0.5) [17]. The US-guided group had a considerably lower puncture time (mean = 22.45 ± 6.95 s) compared to the FL-PCNL group in our study (68.28 ± 56.76 s) (P value 0.001). Agarwall and associate found that puncture took 1.8 min in the US-PCNL group and 3.2 min in FL-PCNL (P value = 0.01) [16]. This significant difference in puncture time did not affect the overall operative time which was statistically non-significant (P value of 0.349) because the mean duration of access time was not significant between both groups (P value 0.460). In contrast El hashash and associate found that US-PCNL patients had longer operative times than FL-PCNL patients mean operative time of 90 min (range 65–130 min) in Group I (C-PCNL), whereas it was 97 min (range 75–145 min) in group II (US-PCNL), which proved to be statistically significant (P value = 0.001) [14], while Sun and associate as well as foo and associate did not find any significant difference in operative time between patients from the US-PCNL and C-PCNl groups [18, 19].
One of the most important advantages of FL-PCNL and combined (FL-PCNL and US-PCNL) is easier and simpler in constructing multiple punctures in case of multiple and branching renal stones which is challenging in US-PCNL [20, 21]. In spite of single-access puncture performed in all patients of US-PCNL versus multiple access puncture in FL-PCNL, the SFR was 86.3% of US-PCNL patients and 80% of FL-PCNL patients without significant difference (P value = 0.336). Wei Sun and associate reported that the US-PCNL had a higher SFR (79.1%) than the control group (69.8%); however, the difference was not statistically significant [18]. The meta-analysis by KunWang and associate concluded higher SFR in the ultra-sonographic access group (odds ratio (OR) 1.26, 95% CI 1.02–1.55, P = 0.03), as well as a lower rate of operative complications (OR 0.72, 95% CI 0.56–0.93, P = 0.01), reduced intraoperative blood loss (mL) (WMD = − 14.55 mL, 95% CI − 27.65 to − 1.46, P = 0.03), and a lower rate of blood transfusion requirement (OR 0.39, 95% CI 0.24–0.63, P = 0.001) [22].
In terms of complications, three FL-PCNL patients needed blood transfusions after surgery. The mean Hb change was 0.23 g/dL and 0.55 g/dL in US-PCNL and FL-PCNL groups, respectively (P value = 0.118). Three FL-PCNL patients had extravasation and were treated with JJ stents, while one US-PCNL patient had post-operative fever (P value = 0.114).
In both groups, Agarwal and associate found no substantial bleeding needing transfusion during or after surgery. Sun and associate found no problems in either group, except fever (4.7% in the US-PCNL and 9.3% in the control group, P value = 0.410) and haemoglobin (7.0% and 11.6%, P value = 0.46) in both groups [16, 18].
While Basiri and associate reported five (10%) US-PCNL patients and three (6%) FL-PCNL patients had intraoperative bleeding (P value 0.5), two (4%) US-PCNL patients and one (2%) FL-PCNL patient needed transfusions to restore hemodynamics. One (2%) patient in both groups needed selective angiographic embolization. Seven ultrasonography and six fluoroscopy patients had supracostal surgery. One FL-PCNL patient (2%) had renal pelvis perforation during access and dilation. After 1 week of nephrostomy drainage, the patient recovered. No subject in the research had organ damage [17].
5 Conclusions
This study added to the existing data demonstrating the efficacy of using either fluoroscopy or ultrasonography guidance to carry out PCNL. However, ultrasound has the benefits of being radiation-free, providing a shorter puncture time, requiring fewer attempts of renal puncture in any type of hydronephrosis indicating higher accuracy, and providing a well orientation towards the adjacent organs, making their injury less liable. Furthermore, ultrasound has nearly the same outcome as conventional PCNL with respect to SFR, bleeding, and other complications and has less cost than fluoroscopy.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALARA:
-
AS low as reasonably achievable
- ASA:
-
American Society of Anesthesiology
- CCTs:
-
Clinically controlled trials
- FL-PCNL:
-
Fluoroscopy-guided percutaneous nephrolithotomy
- ESWL:
-
Extracorporeal shock wave lithotripsy
- mSv:
-
Millisievert
- OR:
-
Odds ratio
- PCNL:
-
Percutaneous nephrolithotomy
- SFR:
-
Stone-free rate
- URS:
-
Ureteroscopy
- US:
-
Ultrasound
- US-PCNL:
-
Ultrasound-guided percutaneous nephrolithotomy
References
Alelign T, Petros B (2018) Kidney stone disease: an update on current concepts. Adv Urol 2018:3068365
Jobs K, Rakowska M, Paturej A (2018) Urolithiasis in the pediatric population—current opinion on epidemiology, patophysiology, diagnostic evaluation and treatment. Dev Period Med 22(2):201–208
Shin TS et al (2011) Complications of percutaneous nephrolithotomy classified by the modified Clavien grading system: a single center’s experience over 16 years. Korean J Urol 52(11):769–775
de la Rosette J et al (2011) The clinical research office of the endourological society percutaneous nephrolithotomy global study: indications, complications, and outcomes in 5803 patients. J Endourol 25(1):11–17
Lipkin ME, Preminger GM (2012) Risk reduction strategy for radiation exposure during percutaneous nephrolithotomy. Curr Opin Urol 22(2):139–143
Kumari G et al (2006) Radiation exposure to the patient and operating room personnel during percutaneous nephrolithotomy. Int Urol Nephrol 38(2):207–210
Furlow B (2011) Radiation protection in pediatric imaging. Radiol Technol 82(5):421–439
Majidpour HS (2010) Risk of radiation exposure during PCNL. Urol J 7(2):87–89
Hosseini MM et al (2009) Ultrasonography-guided percutaneous nephrolithotomy. J Endourol 23(4):603–607
Blackwell RH et al (2017) Incidence of adverse contrast reaction following nonintravenous urinary tract imaging. Eur Urol Focus 3(1):89–93
Hansen KL, Nielsen MB, Ewertsen C (2015) Ultrasonography of the kidney: a pictorial review. Diagnostics (Basel, Switzerland) 6(1):2
O’Neill WC (2014) Renal relevant radiology: use of ultrasound in kidney disease and nephrology procedures. Clin J Am Soc Nephrol 9(2):373–381
Hellawell GO et al (2005) Radiation exposure and the urologist: What are the risks? J Urol 174(3):948–952 (discussion 952)
Elhashash M, Fathi B, Awad R (2021) Comparative study between ultrasound versus fluoroscopy-guided access during percutaneous nephrolithotomy. Sci J Al-Azhar Med Fac Girls 5(1):134–139
Jagtap J et al (2014) Which is the preferred modality of renal access for a trainee urologist: Ultrasonography or fluoroscopy? Results of a prospective randomized trial. J Endourol 28(12):1464–1469
Agarwal M et al (2011) Safety and efficacy of ultrasonography as an adjunct to fluoroscopy for renal access in percutaneous nephrolithotomy (PCNL). BJU Int 108(8):1346–1349
Basiri A et al (2008) Ultrasonographic versus fluoroscopic access for percutaneous nephrolithotomy: a randomized clinical trial. J Endourol 22(2):281–284
Sun W et al (2017) Ultrasound-guided percutaneous nephrolithotomy for the treatment in patients with kidney stones. Medicine (Baltimore) 96(51):e9232
Ng FC et al (2017) Ultrasound-guided percutaneous nephrolithotomy: advantages and limitations. Investig Clin Urol 58(5):346–352
Zhu W et al (2017) A prospective and randomised trial comparing fluoroscopic, total ultrasonographic, and combined guidance for renal access in mini-percutaneous nephrolithotomy. BJU Int 119(4):612–618
Zhu L et al (2020) Risk factors for the fever after percutaneous nephrolithotomy: a retrospective analysis. Transl Androl Urol 9(3):1262–1269
Wang K et al (2015) Ultrasonographic versus fluoroscopic access for percutaneous nephrolithotomy: a meta-analysis. Urol Int 95(1):15–25
Acknowledgements
Great appreciations to all authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript. All authors have contributed sufficiently to the manuscript and approved the final manuscript. This work has not been published previously, nor is any part of its content currently under consideration for publication elsewhere; it will not be published elsewhere in the same form in English or any other language.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AK, AMG, and RM contributed to laboratory work, data handling, writing, and revising the manuscript. AA and AM managed data, carried out statistical analyses, and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Beni-Suef University Faculty of Medicine ethics committee accepted the study, FMBSURGEC/07062020/Gaber.
Consent for publication
All participants gave informed written consent before joining the research after being told its goals. Maintaining data confidentiality was assured.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elmarakbi, A.A., Gaber Mohamed, A.M., Massoud, A.M. et al. Ultrasound-guided percutaneous nephrolithotomy versus conventional c-arm-guided percutaneous nephrolithotomy: a prospective randomized comparative study. Beni-Suef Univ J Basic Appl Sci 13, 10 (2024). https://doi.org/10.1186/s43088-024-00468-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43088-024-00468-y