Abstract
Background
The coronavirus disease-2019 (COVID-19) pandemic crisis has affected millions of people worldwide. The emergence of mutant strains one after the other, breakthrough infections post-vaccination and reinfection of the virus have made it difficult to fight the pandemic and bring an end to it. Naturally available compounds with an array of phytochemicals and potent antiviral properties can provide an alternate solution in improving innate immunity, early recovery and symptomatic cure from COVID-19.
Objective
The present study investigates the efficacy of a polyherbal formulation, NAOQ19, on the rate of recovery and clinical improvement among COVID-19-infected patients who were not on a ventilator or in intensive care unit.
Methods
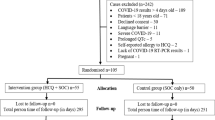
A randomized placebo-controlled study design was adopted for the study. The study enrolled 124 patients with 62 patients included in the NAOQ19 arm and other 62 patients enrolled in the placebo arm along with standard care of treatment. Key outcomes of the study included improvement from COVID-19 based on RT-PCR negative test tested on day 3, 5, 7 and 10, CRP inflammatory rate and drug safety. Data analysis included intention to treat approach. Significance was accepted with a two-sided p value < 0.05 for the outcome measures.
Results
The results of the present study demonstrated higher proportion of patients recovering in NAOQ19 arm compared to placebo arm on day 3 (33.8% vs. 8%; p < 0.001). The mean number of days required to turn RT-PCR (Real-time reverse transcriptase-polymerase chain reaction) negative was also lower in NAOQ19 arm by a day compared to placebo arm (5.4 vs. 6.2; p = 0.022). Inflammatory marker CRP (C-reactive protein) significantly reduced in the NAOQ19 arm at exit compared to placebo arm (6.25 mg/L vs. 10.26 mg/L; p = 0.048). Liver function test and kidney function test profiles were within normal limits during exit demonstrating the drug safety.
Conclusion
NAOQ19 along with standard care of treatment demonstrated higher percentage of population recovering from COVID-19 in comparison with those who were on standard care of treatment.
Trial registration: The trial was also registered in Clinical Trial Registry India with registration number CTRI/2021/10/037423.
Similar content being viewed by others
1 Introduction
Coronavirus disease-2019 (COVID-19) is an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The outbreak of COVID-19 and resulting public health crisis has garnered worldwide attention [1], affecting 200 nations across the world [2]. Many prevention and control measures have been used to limit the spread of COVID-19, such as shutting down travel and other activities; applying quarantine and screening measures, social distancing, and strict personal hygiene rules, such as frequent hand washing, disinfecting surfaces, and wearing face masks [3]. To prevent the variants like delta the continuity of the strict application of protective measures and making the necessary arrangements for the availability of oxygen are recommended. It is also necessary to perform an intensive vaccination process to optimize protection [4].
Health systems resilience is critical for the control of the COVID-19 pandemic [5]. Multiple antivirals, monoclonal antibodies, and immunomodulatory drugs have been suggested as treatments for SARS-CoV-2 infection, but most of these measures have not effectively reduced the risk of progression to severe disease or are too expensive or logistically difficult to treat widely [6]. In the previous year, delta variant of the virus created a massive loss of life among the Indian subcontinent, while the beginning of the year 2022 witnessed the highly infectious Omicron virus [7, 8]. Despite huge vaccination drives in India and worldwide with many being vaccinated against the virus, higher transmissibility, higher chance of reinfection [9], breakthrough infections [10] and viral mutations have been a concern. Regarding the efficacy of these vaccines, previous studies have confirmed that the vaccines are substantially associated with a decrease in hospitalization and death rates. However, multiple studies have shown that, as with other vaccines, the efficacy of the COVID-19 vaccines decreases a few months after the second primer dose [11]. Additionally, all the repurposed and targeted drugs against COVID-19 have brought along many side effects. However, natural antivirals for COVID-19 that pose no side effects are less explored for the cause and accepted in the medical settings.
Several potent herbs and associated formulations available in the nature are recommended for the prophylactic and therapeutic management of COVID-19 [12]. Our study focuses on an polyherbal formulation, NAOQ19 containing well-researched herbs and shrubs from Asian sub-continent such as Withania somnifera, Glycyrrhiza glabra, Piper longum, and Tinospora cordifolia. Several of these drugs have been recognized for their antiviral potency [13,14,15,16,17,18]. Phytochemical analysis of many of these plants demonstrates antimicrobial properties, due to the presence of phenols, alkaloids and flavonoids [19]. A review of the literature on individual components and their phytoconstituents highlights the importance of blending selected herbs into a formulation [20]. In silico studies on Withania somnifera have demonstrated its antiviral properties against SARS-CoV-2 [21, 22]. Among its chief phytochemical components are Withanolides, which play an active role in inhibiting viral entry into the host cells. Potential targets of Withanolides include TMPRSS2 and Mpro receptor protein and viral proteins. These proteins play an important role in viral entry and viral replication inside the host cell [23]. Another molecular docking study of Withania somnifera, Tinospora cordifolia and Asparagus racemosus demonstrated that the combined effect of phytochemicals from the three herbs target against the spike protein, main protease and RNA-dependent RNA polymerase enzyme of the virus required for replication [24]. Glycyrrhiza glabra, another potent antiviral drug, has been studied in silico for its mechanism of action. In silico studies highlight glycyrrhizin as one of the best antiviral chemicals against SARS-CoV-2 [25]. An animal study also highlights that glycyrrhizin plays an important role in reducing the number of angiotensin-converting enzyme 2 (ACE2) receptors in the lung tissue, which is the main binding site of SARS- CoV-2 in humans [26]. Other components of NAOQ19 such as Tinospora cordifolia, Phyllanthus fraternus, Adhatoda vasica, Andrographis paniculata and Curcuma longa contain phytochemicals that target the Mpro protein of the virus. Amritoside and Apigenin-6- C-glucosyl 7-O-glucoside from Tinospora cordifolia, and Pectolinarin and Astragalin from Phyllanthus fraternus are among the few compounds that have demonstrated the highest docking ability with Mpro protein [27]. Few other components from NAOQ19 such as Cissampelos pareira, Ocimum sanctum and Alstonia scholaris are known for its antiviral and anti-inflammatory properties [28].
While several studies have targeted few of the above-mentioned herbs as an antiviral alternative for COVID-19, a combination of herbs targeting several manifestations of COVID-19 is rare. The objective of the present study is to evaluate the efficacy of a novel polyherbal formulation NAOQ19 among COVID-19 patients as noted by RT-PCR recovery rate among patients.
2 Methods
2.1 Trial design
The present study was a double blind, randomized controlled trial. The study protocol was in compliance with the Helsinki Declaration and Good Clinical Practice. The study enrolled patients during the second and third wave of pandemic in India. Adults presenting with mild-moderate COVID-19 infection, at the OPD or IPD in the second wave and mild OPD in the third were screened for eligibility and invited to participate in the study. Informed consent was obtained from patients willing to participate in the trial. The study was conducted from October 27th , 2021, to January 29th, 2022.
2.2 Participants
A total of 124 patients who presented to the OPD/IPD were recruited for the study. 62 patients received the NAOQ19 intervention, while other 62 were given Placebo. Both the arms received standard care of treatment on top of their respective intervention. All enrolled patients presented with symptoms of COVID-19 and were tested positive on RT-PCR. The eligible participants (based on the eligibility criteria listed below) were informed about the research study. Medical history of the patients was documented, and baseline parameters were assessed.
2.3 Inclusion criteria
-
1.
Symptomatic RT-PCR positive COVID-19 cases (with or without comorbidities) as per the GOI norms
-
2.
Reported to OPD within three days of onset of symptoms
-
3.
Patients between the ages of 18–75 years
-
4.
Both Genders (Male and Female)
-
5.
Willing to take Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homeopathy (AYUSH) treatment
2.4 Exclusion criteria
-
1.
Not willing to give consent/participate in the clinical trial
-
2.
Age less than 18 years or more than 75 years
-
3.
Patients with chronic comorbidities like diabetes, chronic heart conditions and HIV/AIDS
-
4.
Patients on immunosuppressive therapy
-
5.
Pregnant women or lactating mothers
-
6.
SARS-CoV-2 infected patients with oxygen saturation less than 90% or those in ICU
2.5 Intervention
Patients enrolled in the study were provided respective intervention along with the standard of care treatment. The patients received a bottle containing 90 tablets each, as per their intervention. They were advised to take two tablets (500 mg each) TID (thrice a day), along with the standard of care treatment. Compliance was monitored by the study team daily for each patient individually, in person for the patients admitted in the hospital while telephonically for out patients (Fig. 1).
2.6 NAOQ19 preparation
NAOQ19 is a polyherbal formulation containing 19 ingredients made with 13 herbs. They are Withania somnifera powder and extract, Aegle marmelos, Glycyrrhiza glabra powder and extract, Pluchea lanceolata, Adhatoda vasica powder and extract, Piper longum, Curcuma longa, Cissampelos pareira, Phyllanthus fraternus powder and extract, Andrographis paniculata powder and extract, Alstonia scholaris, Ocimum sanctum and Tinospora cordifolia powder and extract.
NAOQ19 was licensed by the Ministry of AYUSH, Govt. of India: license number- AUS782. All the herbs & herbal extracts which constituted NAOQ19 were subjected to quality control. All the ingredients were blended with excipients followed by granulation, drying and compression. After passing the QC test, the tablets were packed in bottles following standard procedure.
2.7 Comparator group
The placebo control group was provided with the placebo tablets (made of only starch), which were packed in bottles identical to the NAOQ19 bottle. The placebo tablets were also matched with NAOQ19 for their color.
2.8 Standard treatment of care
Standard of care treatment included allopathic medicines as prescribed by the Government of India [29] during the second and third wave, respectively.
2.9 Outcomes
After enrollment, the patients were monitored daily for the study period. All patients were followed up for RT-PCR test on Day 0, Day 3, Day 5, Day 7, Day 10 to monitor viral load changes. One nasal and one throat swab were obtained for RT-PCR analysis.
2.10 Primary outcome
The rate of recovery based on viral load reduction/ RT-PCR negativity rate on day 0, 3, 5,7, 10 (if required).
2.11 Secondary outcomes
The clinical improvement among the patients as evaluated by the CBC (Complete Blood Count), CRP on baseline, day 5/exit.
To evaluate the safety of the drug by assessing (Liver Function Test) LFT and (Kidney Function Test) KFT on baseline, day 5/exit.
2.12 Sample size calculation
The sample size was calculated based on the study of Devapura et al. [30] where the treatment group witnessed 100% recovery by day 7, while it was 60% in the placebo group. Taking these values as reference, the minimum required sample size with 99% power of study and 1% level of significance is 37 patients in each study group. To reduce margin of error, total sample size taken is 120 (60 patients per group).
2.13 Randomization and blinding
The study participants were allocated into different study arms with the help of a computer generated randomization. The allocation was sequentially distributed with an on-site computer system. The participants, investigator, outcome assessor, data collector, and data entry operator were blinded to the allocated study group. All the subjects were randomized in a 1:1 ratio between the intervention and placebo arm. The appropriate intervention was administered by the duty doctor who was not involved in the study.
2.14 Statistical analysis
Data entry was done in Microsoft Excel and analyzed using IBM Statistical Package for the Social Sciences (SPSS) Statistics, Version 23.0. Demographic variables were tabulated and represented using proportions (%). The analysis was performed using intention to treat approach where all patients randomized are included in the analysis. The study sample was put through the Kolmogorov–Smirnov test to check the data normality. Chi-square or Fisher's exact tests were used for comparisons between groups for categorical data. Quantitative data were presented with mean (SD) and analyzed using Student’s T (paired and unpaired) test wherever applicable. Wilcoxon signed rank test and Mann–Whitney U test were applied wherever the data did not follow normality. Result from Kaplan–Meier analysis provided the mean time for RTPCR conversion from positive to negative and log rank test was used for comparison. Significance was accepted with a two-sided p value < 0.05 for the outcome measures.
2.15 Subgroup analysis
2.15.1 Mild and moderate
Based on the Government of India guidelines [31, 32], the patients were categorized into mild and moderate in both the arms. The categorization was based on the symptoms presented by the patients during the respective wave.
3 Results
The study compared the COVID-19 recovery, as measured by RT-PCR recovery rate, CRP marker and symptoms between the intervention NAOQ19 arm and placebo arm. Attrition rate in both the study groups was zero.
3.1 Demographic characteristics
Table 1 demonstrates the demographic characteristics of the patients enrolled in the study. No significant differences in age or gender distribution were observed between the study groups. The two groups were also similar in their vitals like blood pressure and pulse rate at the time of enrollment. Patients were also categorized based on the severity of illness into mild and moderate illness type. Immunization status of the patients was also captured to analyze any change in response of the intervention between the partially and fully vaccinated groups.
3.2 RT-PCR
Patients turning RT-PCR negative among overall, mild and moderate patients in both the arms were analyzed. Difference in percentage population turning RT-PCR negative in NAOQ19 and placebo arm was measured (Table 2 and Figs. 2 and 3).
Proportion of patients with RTPCR negative at day 3 was significantly higher in NAOQ19 arm as compared to Placebo arm. (Negative: − 33.8% vs. 8%, respectively, p value < 0.01). On day 5, the percentage of population turning negative was comparable between the arms (Negative: − 72.5% vs. 70.9%, respectively, p value 0.84). On day 7, the percentage population turned negative in the NAOQ19 arm was slightly higher than the placebo arm (Negative: − 82.2% vs. 72.5%, respectively, p value 0.19).
Among the mild patients, 16 (40%) patients turned RT-PCR negative in the NAOQ19 arm, while 3 (7.7%) patients turned negative in the placebo arm on day 3. Further on day 5, 37 (92.5%) patients turned RT-PCR negative in the NAOQ19 arm, while 34 (87.2%) patients turned negative in the placebo arm. On day 7, 40 (100%) patients turned RT-PCR negative in the NAOQ19 arm while 35 (89.7%) patients turned negative in the placebo arm (p value 0.05).
Among the moderate patients, 5 (22.7%) patients turned negative in the NAOQ19 arm on day 3 while 2 (8.7%) patients turned negative in the placebo arm. On day 5, 8 (36.36%) patients turned negative in the NAOQ19 arm, while 10 (43.4%) patients turned negative in the placebo arm. While on day 7, 11 (50%) patients turned negative in the NAOQ19 arm while 10 (43.5%) patients turned negative in the placebo arm. By Day 10, all the patients had turned RT-PCR negative.
3.3 Time to become RT-PCR negative
Time to event (defined as RT-PCR negative) analysis was done using Kaplan–Meier method (Fig. 4). The analysis showed lower mean time to turn RTPCR negative in NAOQ19 arm with 5.4 days as compared to 6.2 days in placebo arm. This difference was found to be significant, p = 0.022 by Log Rank (Mantel–Cox) test (Table 3).
3.4 Time to become RT-PCR Negative among immunized versus partially immunized patients
The analysis showed lower mean time to turn RTPCR negative in intervention arm when fully immunized with 4.3 days as compared to 6.0 days in placebo arm. This difference was significant, χ2 = 15.842, p = 0.000 by Log Rank (Mantel–Cox) test (Table 4).
3.5 Duration of stay for IPD patients
The patients admitted in the hospital were also characterized for mean number of days in the hospital (duration of stay). The patients in NAOQ19 arm were discharged significantly earlier (mean number of days-5.45) compared to the placebo arm (mean number of days-6.27) (p value = 0.01) (Table 5).
3.6 CRP Inflammatory marker
It was also noted that both the arms did not show difference in CRP values on day 0 while the values significantly differed by Day 5/exit between the 2 arms. The difference in CRP values on day 5 or exit was statistically significant between the two arms (p value = 0.048). It is depicted in Table 6 and Fig. 5 (Fig. 6).
4 Discussion
Natural herbs have been widely utilized for viral flu and other seasonal infections. COVID-19, like any other viral pandemic, has costed life of millions with extending the disease for more than 2 years now. With the promise to end the COVID-19 pandemic inching closer, some integrative solution strategies can provide an accelerated elimination. The present study explored efficacy of a polyherbal formulation in treating a COVID-19 patient when given on top of standard care of treatment. Key finding reported in the present study includes higher population of patients experiencing early recovery in the NAOQ19 arm with a statistical significance. However, the placebo arm demonstrates a slow and gradual improvement in the recovery. This result is supported by noticing significantly reduced number of days in time to become RT-PCR negative and duration of stay in the hospital for IPD patients. The findings from this study are supported by a similar AYUSH drug, Kabasura Kudineer, well studied for its efficacy in symptomatic recovery and therapeutic cure against COVID-19 demonstrated that that patients in the intervention group along with standard therapy took only 2.7 days to turn asymptomatic while those with only standard of care treatment took 4.2 days [27].
Among the researched herbs, Glycyrrhiza glabra has been extensively studied via in silico studies for the presence of phytochemicals possessing antiviral properties. Glycyrrhizin, a component of Glycyrrhiza glabra, has been identified as the chief component responsible for inhibiting the attachment of SARS-CoV-2 spike protein with the ACE-2 receptors [33]. Clinical trials on Withania somnifera have demonstrated its immunogenic, anti-inflammatory and adaptogenic properties [34]. Adhatoda vasica is a well-known anti-inflammatory, antiviral and antitussive herbal drug [35]. Known for its antithrombotic properties, Andrographis paniculata prevents blood clotting. Blood clotting is one of the severe clinical presentations of SARS-CoV-2 virus [36] and antithrombotic properties of Andrographis paniculata can reduce blood clotting. A common routinely used spice in India, Curcuma longa has an excellent antiviral properties [37]. Curcumin, the chief component of Curcuma longa, is a phenolic compound which has an inhibitory effect against Toll-like receptors, inflammatory cytokines and chemokines [38, 39]. This is crucial in COVID-19 since it can regulate the cytokine levels and inhibit the cytokine storm. The present anti-inflammatory property of NAOQ19 is also supported by significant reduction in CRP among the NAOQ19 group patients by Day 5/exit. These herbs together may be the probable cause for easy elimination, providing faster recovery and enhanced immunity against SARS-CoV-2.
Another important finding of the study was that fully immunized patients had a significant expedited recovery when treated with NAOQ19 while patients in the standard care of treatment arm followed a normal recovery curve. A similar study explores the efficacy of Withania somnifera on enhancing immunogenicity among COVID-19 patients [40]. Studies in the past have demonstrated the role of both cell-based and humoral-based immunity against SARS-CoV-2 [41]. Several studies have demonstrated the immune boosting properties of various phytochemicals such as curcumin and lactoferrin present in herbal medicine to increase cell-based immunity. A review on Ayurvedic Indian system of medicines demonstrated the role of Adhatoda vasica used as an adjuvant to enhance immunogenicity of the vaccines [42]. SARS-CoV-2 enters through nasal-oral route invoking mucosal immunity along with other antibody subtypes. However, most vaccine-based immunity only produces IgG response. Since the consumption of polyherbal formulation such as NAOQ19 is also through oral route, these herbal medicines can offer a potential adjuvant role in enhancing the vaccine-based immunity. [42]
In addition to objective marker analysis, the study also monitored side effects of the drug upon consumption. Patients in the NAOQ19 arm reported no adverse events. In vitro and in vivo studies [43, 44] on the effectiveness of the polyherbal formulation, NAOQ19 also showed significant viral load reduction. The in vivo animal study on infected Syrian golden hamsters demonstrated a 78.2% viral load reduction in hamster lungs compared to the infected untreated group. Along with that no mortality was observed in hamsters that were treated with NAOQ19, bodyweights of NAOQ19 treated hamsters improved and did not worsen over the course of treatment.
The presented few limitations during the clinical trial, such as absence of biomarkers such as ferritin, interleukins, D-Dimer and other inflammatory markers. Along with addressing the limitations of the present study, future scope of the study involves large group double blind clinical trials in other viral infections to test the antiviral properties of the novel polyherbal formulation.
5 Conclusion
Nature is abundant with resources that have curative and preventive properties against various harmful organisms. The present study explores the efficacy of novel polyherbal formulation NAOQ19 in COVID-19 management in a clinical trial. Our study demonstrated NAOQ19 to provide expedited COVID-19 recovery, viral load reduction and clearance and reduction in anti-inflammatory properties associated with NAOQ19. With the emergence of every new strain or sub-strain of the virus and breakthrough infections, the challenge to end the pandemic is pushed farther away. During such times, natural therapy without any side effects can aid in improving innate immunity in addition to acquired immunity through vaccine. Findings of the present study with superior benefits can integrate NAOQ19 as an adjuvant therapy to standard of care in clinical practice.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus disease-2019
- RT-PCR:
-
Real-time reverse transcriptase-polymerase chain reaction
- CRP:
-
C-reactive protein
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome Corona Virus 2
- ACE 2:
-
Angiotensin-converting enzyme 2
- AYUSH:
-
Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homeopathy
- SPSS:
-
Statistical Package for Social Sciences
- KFT:
-
Kidney function test
- LFT:
-
Liver function test
- CBC:
-
Complete blood count
- OPD:
-
Outpatient department
- IPD:
-
Inpatient department
References
Jin Y, Yang H, Ji W et al (2020) Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses 12(4):372
Pal R, Yadav U (2020) COVID-19 pandemic in India: present scenario and a steep climb ahead. J Prim Care Community Health 11:2150132720939402
Hamimes A, Aouissi HA, Ababsa M et al (2022) The effect of preventive measures and vaccination against SARS-CoV-2 on the infection risk, treatment, and hospitalization: a cross-sectional study of Algeria. Viruses 14(12):2771. https://doi.org/10.3390/v14122771
Aouissi HA (2021) Algeria’s preparedness for Omicron variant and for the fourth wave of COVID-19. Glob Health Med 3(6):413–414. https://doi.org/10.35772/ghm.2021.01117
Zhang H, Sun Y, Wang Y et al (2022) Recent developments in the immunopathology of COVID-19. Allergy. https://doi.org/10.1111/all.15593
Najjar-Debbiny R, Gronich N, Weber G et al (2023) Effectiveness of Paxlovid in reducing severe coronavirus disease 2019 and mortality in high-risk patients. Clin Infect Dis 76(3):e342–e349. https://doi.org/10.1093/cid/ciac443
Zhang H, Sun Y, Wang Y et al (2022) Recent developments in the immunopathology of COVID-19. Allergy. https://doi.org/10.1111/all.15593
World Health Organization (2021) Coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed on 10 Sept 2021
Gavriatopoulou M, Ntanasis-Stathopoulos I, Korompoki E et al (2021) Emerging treatment strategies for COVID-19 infection. Clin Exp Med 21(2):167–179
Weber S, Ramirez CM, Weiser B, Burger H, Doerfler W (2021) SARS-CoV-2 worldwide replication drives rapid rise and selection of mutations across the viral genome: a time-course study–potential challenge for vaccines and therapies. EMBO Mol Med 13(6):e14062
Kislaya I, Rodrigues EF, Borges V, Gomes JP, Sousa C, Almeida JP et al (2022) Comparative effectiveness of coronavirus vaccine in preventing breakthrough infections among vaccinated persons infected with Delta and Alpha variants. Emerg Infect Dis 28(2):331
Lounis M, Aouissi HA, Abdelhadi S et al (2022) Short-term adverse effects following booster dose of inactivated-virus vs. adenoviral-Vector COVID-19 vaccines in Algeria: a cross-sectional study of the general population. Vaccines 10(11):1781. https://doi.org/10.3390/vaccines10111781
Patwardhan B, Chavan-Gautam P, Gautam M, Tillu G, Chopra A, Gairola S et al (2020) Ayurveda rasayana in prophylaxis of COVID-19. Curr Sci 118(8):1158–1160
Santhanu K, Senthil K (2021) Therapeutic potential of Withania somnifera (Linn) Dunal (Ashwagandha) in historical perspective and pharmacological evidence. Ann Ayurvedic Med 10(2):135–147
Anagha K, Manasi D, Priya L, Meera M (2014) Scope of Glycyrrhiza glabra (Yashtimadhu) as an antiviral agent: a review. Int J Curr Microbiol App Sci 3(12):657–665
Kumar A, Prasad G, Srivastav S, Gautam VK, Sharma N (2020) Efficacy and safety of Guduchi Ghan vati in the management of asymptomatic COVID-19 infection: an open label feasibility study. MedRxiv 65:179204
Jikadara J, Roy SP (2021) Review on potential herbal remedies to combat Covid-19. J Ayurvedic Herb Med 7(2):124–133
Lal J (2012) Turmeric, curcumin and our life: a review. Bull Environ Pharmacol Life Sci 1(7):11–17
Joshi RK, Setzer WN, Da Silva JK (2017) Phytoconstituents, traditional medicinal uses and bioactivities of Tulsi (Ocimum sanctum Linn.): a review. Am J Essent Oil Nat Prod 5(1):18–21
Ben-Shabat S, Yarmolinsky L, Porat D, Dahan A (2020) Antiviral effect of phytochemicals from medicinal plants: applications and drug delivery strategies. Drug Deliv Transl Res 10(2):354–367
Bone K (2003) A clinical guide to blending liquid herbs E-Book: herbal formulations for the individual patient. Elsevier Health Sciences
Shree P, Mishra P, Selvaraj C, Singh SK, Chaube R, Garg N, Tripathi YB (2020) Targeting COVID-19 (SARS-CoV-2) main protease through active phytochemicals of ayurvedic medicinal plants–Withania somnifera (Ashwagandha), Tinospora cordifolia (Giloy) and Ocimum sanctum (Tulsi)–a molecular docking study. J Biomol Struct Dyn 40:190–203
Tripathi MK, Singh P, Sharma S, Singh TP, Ethayathulla AS, Kaur P (2020) Identification of bioactive molecule from Withania somnifera (Ashwagandha) as SARS-CoV-2 main protease inhibitor. J Biomol Struct Dyn 39:5668–5681
Borse S, Joshi M, Saggam A, Bhat V, Walia S, Marathe A et al (2021) Ayurveda botanicals in COVID-19 management: An in silico multi-target approach. PLOS ONE 16(6):e0248479
Niraj S, Varsha S (2020) A review on scope of immuno-modulatory drugs in Ayurveda for prevention and treatment of Covid-19. Plant Sci Today 7(3):417–423
Damle M (2014) Glycyrrhiza glabra (Liquorice)-a potent medicinal herb. Int J Herb Med 2(2):132–136
Jezova D, Karailiev P, Karailievova L, Puhova A, Murck H (2021) Food enrichment with Glycyrrhiza glabra extract suppresses ACE2 mRNA and protein expression in rats—possible implications for COVID-19. Nutrients 13:2321
Murugesan S, Kottekad S, Crasta I, Sreevathsan S, Usharani D, Perumal MK et al (2021) Targeting COVID-19 (SARS-CoV-2) main protease through active phytocompounds of ayurvedic medicinal plants–Emblica officinalis (Amla), Phyllanthus niruri Linn. (Bhumi Amla) and Tinospora cordifolia (Giloy)—a molecular docking and simulation study. Comput Biol Med 136:104683
Revised Guidelines on Clinical Management of COVID-19. https://www.mohfw.gov.in/pdf/RevisedNationalClinicalManagementGuidelineforCOVID1931032020.pdf. Accessed on 30 Sept 2021
Pandey K, Shevkar C, Bairwa K, Kate AS (2020) Pharmaceutical perspective on bioactives from Alstonia scholaris: ethnomedicinal knowledge, phytochemistry, clinical status, patent space, and future directions. Phytochem Rev 19(1):191–233
Devpura G, Tomar BS, Nathiya D, Sharma A, Bhandari D, Haldar S, Balkrishna A, Varshney A (2021) Randomized placebo-controlled pilot clinical trial on the efficacy of ayurvedic treatment regime on COVID-19 positive patients. Phytomedicine 84:153494. https://doi.org/10.1016/j.phymed.2021.153494
Desai S, Gupta A (2020) IASO COVID-19 guidelines (updated on 9th April 2020). Indian J Surg Oncol 11(2):171–174
Kanchibhotla D, Harsora P, Subramanian S, Reddy MRK, Venkatesh HKR (2023) Rate of recovery and symptomatic efficacy of a polyherbal AYUSH formulation in the treatment of SARS-CoV-2 disease: a single-arm trial. Altern Ther Health Med 29(4):134–139
Hoever G, Baltina L, Michaelis M, Kondratenko R, Baltina L, Tolstikov GA et al (2005) Antiviral activity of glycyrrhizic acid derivatives against SARS−coronavirus. J Med Chem 48(4):1256–1259
Gupta GL, Rana AC (2007) Withania somnifera (Ashwagandha): a review. Pharmacognosy Rev 1(1)
Khanal H, Khanal U, Koirala J (2020) Medicinal plant vasaka could be a therapeutic option for the management of COVID-19 symptoms. J Med Plants 8(5):44–48
Mishra SK, Sangwan NS, Sangwan RS (2007) Phcog rev.: Plant review Andrographis paniculata (Kalmegh): a review. Pharmacogn Rev 1(2):283–298
Mathew D, Hsu WL (2018) Antiviral potential of curcumin. J Funct Foods 40:692–699
Zahedipour F, Hosseini SA, Sathyapalan T, Majeed M, Jamialahmadi T, Al-Rasadi K et al (2020) Potential effects of curcumin in the treatment of COVID-19 infection. Phytother Res 34(11):2911–2920
Soni VK, Mehta A, Ratre YK, Tiwari AK, Amit A, Singh RP et al (2020) Curcumin, a traditional spice component, can hold the promise against COVID-19? Eur J Pharmacol 886:173551
Saggam A, Limgaokar K, Borse S, Chavan-Gautam P, Dixit S, Tillu G, Patwardhan B (2021) Withania somnifera (L.) Dunal: opportunity for clinical repurposing in COVID-19 management. Front Pharmacol 12:835
Garcia-Beltran WF, Lam EC, Denis KS, Nitido AD, Garcia ZH, Hauser BM et al (2021) Multiple SARS-CoV-2 variants escape neutralization by vaccine-induced humoral immunity. Cell 184(9):2372–2383
Tiwari R, Latheef SK, Ahmed I, Iqbal H, Bule MH, Dhama K et al (2018) Herbal immunomodulators-a remedial panacea for designing and developing effective drugs and medicines: current scenario and future prospects. Curr Drug Metab 19(3):264–301
Kanchibhotla D, Subramanian S, Kumar RM, Hari KV, Pathania M (2022) An In-vitro evaluation of a polyherbal formulation, against SARS-CoV-2. J Ayurveda Integr Med 13(3):100581
Acknowledgements
We would like to acknowledge Dr Somya Ramrakhyani for language edits.
Funding
There was no funding provided for the study.
Author information
Authors and Affiliations
Contributions
DK made substantial contribution toward the concept and design of the study besides interpretation of the data and revision of the manuscript. AA made substantial contribution in the collection, analysis of the data as well as the revision of the manuscript. SS made substantial contribution in analysis of data as well as drafted the manuscript. All authors read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was approved by the Institutional ethics committee of Atharva multi-specialty hospital and research, with the registration number IEC/04/17/21/01. Informed consent was obtained from patients willing to participate in the trial. The trial was also registered in Clinical Trial Registry India with registration number CTRI/2021/10/037423.
Consent for publication
Publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out. Informed consent was taken from the participants before the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arun, A., Subramanian, S. & Kanchibhotla, D. Efficacy of polyherbal formulation along with standard care of treatment in early recovery of COVID-19 patients: a randomized placebo-controlled trial. Beni-Suef Univ J Basic Appl Sci 12, 103 (2023). https://doi.org/10.1186/s43088-023-00420-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43088-023-00420-6