Abstract
Background
The current study expands on the use of design of experiment in developing cefuroxime axetil mucoadhesive minitablets for treating antibiotic-associated colitis. A comprehensive QbD-based product development strategy was implemented, with the target product profile defined based on the desired product quality of mucoadhesive minitablets. The identified critical quality attributes are based on the target product profile. The goal was to find the optimum levels by using the concentrations of chitosan (mg) (X1), HPMC K100M (X2) and sodium carboxymethyl cellulose (X3) as the influential variables. The response surface methodology determines the dependent variables using 33 Box–Behnken design to optimize the selected critical factors. The friability (%), drug content (%) and mucoadhesive strength (%) characteristics of cefuroxime axetil mucoadhesive minitablets were evaluated using ANOVA for the observed responses or dependent variables.
Results
The study demonstrated that run 8 with optimum composition chitosan, HPMC K100M and sodium carboxy methyl cellulose, which are the mucoadhesive polymers, showed a desirable and promising drug release profile up to 24 h, higher percentage of drug content, mucoadhesion and swelling index.
Conclusions
The optimized mucoadhesive minitablets of cefuroxime axetil demonstrated desired formulation characteristics, including improved bioavailability and high control over the drug’s release rate and increased flexibility in adjusting both the dose and the drug’s release rate. In a nutshell, the studies support the successful development of mucoadhesive minitablets of cefuroxime axetil, which could be used to treat antibiotic-associated colitis.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.1 Background
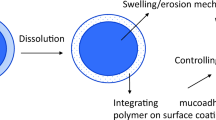
Antibiotic cefuroxime axetil (CA) is a second-generation cephalosporin antibiotic with low solubility and high permeability (BCS Class-II). There are 32% oral bioavailability and a short half-life for CA [1]. Cefuroxime is hydrolysed by nonspecific esterase enzymes when CA is attached to the intestinal mucosa, and the highly polar carboxyl group is ionized in this environment. This condition occurs when a large amount of antibiotic enters the colon [2]. Proximal to the GI tract, CA has a higher rate of absorption at pH 8. Cefuroxime axetil (CA) has an absorption window located in the proximal gastrointestinal tract that can be overcome by slowing the release of cefuroxime axetil from the formulation. As a result, better absorption of CA necessitates a gastro-retentive mucoadhesive drug delivery system. Minitablets with modified release mucoadhesion consist of multiple subunits, each containing a different dose of medication [3]. As a result, the dose is the sum of the quantities of the drug in each subunit, and the total functionality of the dose is directly correlated with each individual subunit's functionality. Also, a common problem with the oral sustained release dosage form is that it does not have a long-term ability to remain in the proximal part of the small intestine [4, 5]. When it comes to prolonging the gastric residence time of solid dosage forms, mucoadhesive drug delivery systems offer the most effective and rational protection against early and random gastric emptying. Modified release bioadhesive systems were developed as a result of the reliability and irreproducibility of single-unit solid dosage forms in prolonging gastric residence time due to the problem of all or nothing emptying [6, 7]. There is great promise in the development of minitablets, which will allow for greater control over drug release rates while allowing for greater dose due to less adverse effects, enhanced residence time of drug in oral cavity, with release rate customization [8,9,10]. Box–Behnken experimental design, a three-factor three-level (− 1, 0, 1) notable response surface methodology, was used to perform statistical optimization of the developed formulation to determine the specific interactions of the parameters. Additionally, the Box–Behnken design incorporates the idea of interpreting category and numerical factors through the use of (1–5) minimum centre points [5, 6, 8]. The conventional immediate release (IR) formulation available in the market shows inability to accomplish desired drug release profile owing to poor retentivity in the stomach for extended periods of time and the utility of diverse gastroretentive floating formulations of cefuroxime axetil, yet, these systems are not considered to be highly satisfactory for attaining the desired retentivity in the gastric absorption window owing to floatation characteristics only. Thus, attempts were made to develop the mucoadhesive minitablets employing dual approach of floatation and bioadhesion for maintaining drug absorption and plasma concentration of the drug for prolonged periods of time and improving the therapeutic efficacy of cefuroxime axetil. Chitosan is a cationic polysaccharide polymer and mostly used for the development various novel delivery system low toxicity properties. Chitosan has –OH and –NH2 functional groups and its chemically modified derivatives ability to form hydrogen and covalent bonds and stick to the mucus membrane in the targeting site of the drug delivery [9,10,11]. HPMC K100M is a common binder, film coating and controlled-release matrix polymer used mainly for preparation of solid dosages forms including hydrophilic matrix tablets formulations because as it forms quickly homogeneous, strong, viscous gel over the dosage form and protects the drug release in a controlled manner from the matrix. On the other hand, the amount of drug present in the matrix causes the swelling properties of the matrix to become more pronounced [11,12,13].
2 Materials and methods
2.1 Materials
Cefuroxime axetil was obtained as a gift sample from Dr Reddy’s Laboratory, Hyderabad, India. HPMC K100M was a gift sample from Colorons, Goa. The sodium carboxymethyl cellulose and chitosan were procured from Himedia Laboratories Ltd., Mumbai. All other chemicals and reagents used were of analytical grade.
2.2 Methods
2.2.1 Target product profile (TPP)
The formulation's target product profile (TPP) containing cefuroxime axetil minitablets was determined to improve its bioavailability. Analysing quality target product profile (QTPP), factors such as mucoadhesive strength, friability and ex vivo or in vivo pharmacokinetic profiles were used to traverse the optimum multi-dimensional space based on method factors, i.e. method of operable design (MODR) by selecting optimum process parameters and quality attributes [14, 15].
2.2.2 Critical quality attributes (CQAs)
Among the entire TPPs, several crucial and promising quality attributes are designated as CQAs based on the criticality effect upon prepared minitablets by mapping the critical process parameters (CPPs) [16,17,18]. The intent CQAs such as % friability, mucoadhesive strength and % drug contents were chosen.
2.3 Pre-formulation study
2.3.1 Determination of solubility
The solubility was determined by adding an excess amount of CA in a screw-cap glass vial to which 20 ml of SGF or water was added. The samples were shaken at 25 ± 0.5 °C for 24 h on a Mini-Rotary shaker (RS-12R DX, Remi, India). After 48 h, the samples were filtered through a 0.45-μm membrane filter. The filtrate was diluted ten times and further analysed at maximum wavelength λmax at 281 nm using a UV–visible spectrophotometer (Shimadzu UV-1800, Switzerland).
2.3.2 Drug–excipient compatibility study
2.3.2.1 Fourier transform infrared spectroscopy (FT-IR)
FT-IR analysis was performed on pure drug CA and its physical mixture with mucoadhesive polymers (HPMC K100M, chitosan and sodium carboxy methylcellulose) to determine drug–polymer compatibility using KBr discs (IR Affinity, Shimadzu, Japan). The apparatus was operated with a dry air purge, and scans were taken at a scanning speed of 2 mm/sec with a resolution of 4 cm−1 over the range 4000–400 cm−1.
2.3.2.2 Differential scanning calorimetry (DSC)
The thermal analyses were performed using a differential scanning calorimeter (DSC-TA-60, Shimadzu, Japan). Approximately 2 mg of CA and its physical mixture with mucoadhesive polymers (HPMC K100M, chitosan and sodium carboxy methyl cellulose) were placed in a sealed aluminium pan and heated at a scanning rate of 10 °C/min from 30 to 300 °C. An empty aluminium pan was used as a reference.
2.3.3 Preparation of mucoadhesive minitablets
The drug (CA), mucoadhesive polymers (HPMC K100M, chitosan and sodium carboxy methyl cellulose) and other excipients were passed through sieve 40. Then, required quantities of each ingredient were weighed as per Table 1 and were mixed for 10 min. The final powder mixes were compressed into minitablets of 3 mm diameter using multi-tip flat punches (Karnavati, Ahmedabad, India). The batch size of each formulation was 50 minitablets.
2.4 Statistical analysis and optimization of variables using experimental design
2.4.1 Statistical analysis
Design-Expert® (version 12), Stat-Ease Inc., Minneapolis, MN, advanced statistical software of USA, was employed for formulation optimization and the estimation of its critical method parameters (CMAs) [9]. Microsoft performed the data evaluations excels 2007 (Microsoft, USA).
2.4.2 Optimization of variables using experimental design
The experiments were carried out using the Box–Behnken experimental design, with 15 runs using three categories and three numerical factors with single-centre points using response surface methodology [8, 14]. Design-Expert 12 statistical software was used to optimize the formulation. Further away from these focal points, consecutive cumulative replicates of CQAs were created for evaluation [14]. The concentrations of chitosan (X1), HPMC K100 M (X2) and sodium CMC (X3) are chosen as influential factors while keeping the other factors constant at a low level. Based on preliminary data from the analysis, three levels (− 1, 0 and 1) were chosen for each factor. Table 2 shows the 15 runs (centre points 1) using a three-factor at three levels of 33 BBD [15, 16, 18]. Characterization studies on each formulation were carried out to investigate the effect of various factors.
2.4.2.1 Interpretation of Box–Behnken design using ANOVA
Calculating quadratic polynomial equations, counter plot analysis, and using response surface to exemplify interactions intensified the mathematical model, which was then used to interpret the results through graphical optimization using overlay plots and 2D and 3D plots [15, 16] as shown in Fig. 1a–f. The Box–Behnken design was carried out by demonstrating a strong link between the independent and dependent variables [16,17,18]. The model F-value of 18.24 for the response R1 (% Friability) indicates that the model is significant. There is only a 0.26 per cent chance that the F-value will be abnormally high, which could be due to noise. P-values less than 0.0500 indicate that the model is valid. The predicted R2 value is 0.6897, while the adjusted R2 value is 0.9173, meaning that the predicted and actual values are nearly equal and pass through the central axis (Fig. 2). In the same way, R2 is a response (% drug content). The model F-value of 14.98 indicates that the model is statistically significant. There is only a 0.41 per cent chance that the F-value will differ due to noise. Model terms with P-values less than 0.0500 are considered essential. Similarly, the adjusted R2 was found to be 0.8999, and the predicted R2 was 0.4278. As an S/N ratio, the appropriate precision value was used to navigate. For model significance, a ratio greater than four is preferred. The calculated ratio of 9.942 indicates a sufficient signal, implying that the current model was adequate for navigating the design space. After interpretation of BBD, the quadratic polynomial Eqs. (1–3) were calculated, which are represented as follows:
Here, the responses [R1], [R2] and [R3] represent the evaluation of % friability, % drug content and % mucoadhesive strength, respectively.
2.4.3 Response surface analysis of 2D and 3D counter plots
2.4.3.1 Interaction of factor X1 (concentration of chitosan) on the responses (% friability), (% mucoadhesive strength) and (% drug content)
By gradually increasing the concentration of chitosan, there is a deliberate change in the variables, i.e. % friability to its low density, poor flowability and compression characteristics. Similarly, tolerable variations are observed in the available responses such as % drug content and mucoadhesive strength [8, 14].
2.4.3.2 Interaction of factor X2 (concentration of HPMC K100M) on the responses (% friability), (% mucoadhesive strength) and (% drug content)
The 2D counter and 3D response surface plots (Fig. 1) depict that HPMC K100M and chitosan polymer were found to be the most influential factors, which indicates that the desirable sustain release profile of the drug in 24 h signifies in 2D and 3D plots. A gradual increase in the HPMC K100M proportions may gradually increase the viscosity of the minitablet matrix gel layer with a longer diffusional path. The formulation F8 (with experimental run 7) was selected as an optimized formulation through graphical and numerical optimizations through point predication and confirmation data demonstrated, which reflects the values of 0.16 (% friability) R1, 98.9% drug content, R2 and 6.184 as (% mucoadhesive strength) R3. Here, R1, R2 and R3 depict the individual responses. Table 2 represents the design matrix of Box–Behnken design with coded levels, and Table 3 signifies the predicted and experimental responses, which are almost closer to the central axis. The plots are depicted in Fig. 2. From the critical factors' results, HPMC K100M is chosen as the rate-controlling polymer with the propensity for oral extended-release drug delivery, elucidating the most robust formulations and simplified production among other selected polymers [17]. Similarly, the interaction effect of the influential variable (HPMCK 100 M) and its observed responses are explained in perturbation plots, shown in Fig. 3. Ultimately, the quadratic model exposed a good correlation with the tentative experimental data employed to navigate the design space.
2.4.3.3 Interaction of factor X3 (concentration of sodium CMC) on the responses (% friability), (% mucoadhesive strength) and (% drug content)
The sodium CMC considerably impacted the per cent friability and per cent mucoadhesive strength responses and favoured the per cent drug content. However, due to the ionic features of the applied sodium CMC concentration, a progressive increase in mucoadhesive strength was seen; similarly, purposeful change was found in the variables of per cent friability and per cent drug content due to its viscosity modification propensity [14, 18].
2.4.4 Characterization of mucoadhesive minitablets
2.4.4.1 Quality control tests for minitablets
The drug content was determined by crushing ten minitablets with a pestle in a mortar. Weighing an amount equal to 10 mg of CA and transferring it to a 10-mL volumetric flask, 10 mL SGF was added to the formulation powder without enzyme, sonicated for 5 min, filtered and analysed at 281 nm in a UV–visible spectrophotometer (Shimadzu, Japan). Using a portable digital hardness tester (Electrolab, India), the hardness of six minitablets was determined, and the average of six minitablets was calculated. The friability of minitablets was tested using a Roche friability tester with 20 minitablets. The total weight of ten minitablets was determined before and after the friability test, and the per cent weight loss was calculated. The per cent deviation was calculated using the collective and individual weights of 20 minitablets as a weight variation test.
2.4.4.2 In vitro dissolution study and kinetics
The USP type 2 apparatus was used to conduct an in vitro dissolution investigation on mucoadhesive minitablets of CA in SGF without enzyme. Time stamps of 0, 0, 0, 0, 1, 1, 2, 3, 4, 6, 8, 10, 12, 18 and 24 h were used to collect the 5-mL aliquots from the dissolution jar. The dissolution jar was refilled with 5 mL of fresh dissolution medium to maintain a sinking state. Various kinetics equations, such as zero-order, first-order, Higuchi and Korsmeyer–Peppa's equations, were used to examine the order and mechanisms of drug release for all formulations.
2.4.4.3 Ex vivo mucoadhesion study
The strength of the mini-mucoadhesive tablet was measured using the modified physical balance. The device is a modified double pan physical balancing with additional weight added to the right pan to bring the weight on the right side to the same level as the weight on the left side. A tiny beaker was placed beneath the balance's right-side pan in a beaker filled with SGF without enzyme. The moistening fluid was SGF without enzyme, while the model membrane was goat stomach mucosa. A goat's stomach mucosa was acquired from a nearby slaughterhouse and delivered in a Kerb's solution. The underlying mucous membrane was removed with a surgical blade and extensively cleaned with an SGF medium. It was then tied over the smaller beaker with thread, cello tape and elastic bands. During the trials, the smaller beaker was filled with SGF such that the enzyme did not come into contact with the viable upper surface of the goat stomach mucosa. The balance's right arm/pan was linked to one side of the mini-tablet, and the beaker was slowly elevated until contact was formed between the goat mucosa and the mucoadhesive mini-tablet. One gramme preload was placed on the slide for 5 min to induce adhesion bonding between the mucoadhesive mini-tablet and the goat stomach mucosa (preload time). The preload and preload time were kept constant across all formulations. Burette removed the preload from the right side and continued to pour water into the glass beaker in the left arm at a consistent rate of 100 drops per minute. After the mucoadhesive mini-tablet was removed from the goat stomach mucosa, the water was turned off. The amount of water required to remove a mucoadhesive mini-tablet from the stomach mucosa was characterized as mucoadhesion strength (g). The following parameters were calculated from the mucoadhesion strength using Eqs. 4 and 5.
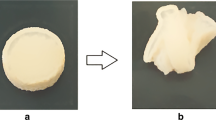
2.4.5 Swelling index and percentage of hydration
Each mini-tablet was weighed (W0) and placed in a beaker with 200 mL of SGF without enzyme for the duration of the experiment (0.5, 1, 2, 4, 8 and 24 h). After immersion, the mini-tablet was taken from the beaker, and excess surface water was collected from the minitablets using filter paper. The swelling index and percentage of hydration were computed using Eqs. 6 and 7.
where \(W_{t }\) and \(W_{o}\) are the weights of the minitablet at particular time t and 0, respectively.
2.5 Stability study
Selected minitablet formulation was subjected to accelerated stability as per ICH guidelines, i.e. at 40 ± 2 °C with relative humidity 75 ± 5%. The study was performed for 6 months, and the samples were analysed at 0, 3 and 6 months for drug content and mucoadhesive strength [14].
2.6 Pharmacokinetic study
The Institutional Animal Ethical Committee approved this study of Jeeva Life Sciences, Hyderabad (CPCSEA Reg. no.: 1757/PO/ReBiBt/S/14/CPCSEA). For the bio-analytical estimation of CA in rabbit serum samples, the reported UFLC method was used [14, 15]. At 1 mL/min, PDA was used to monitor the flow of 80:20 (v/v) water/methanol as a mobile phase on a C18 column with an i.d. of 25 cm by 4.6 mm and 5 m particle size. CA had a retention time of 3.182 min when it was eluted. CA in the mobile phase and serum calibration curve was constructed. CA was extracted from serum samples using ethyl acetate as a solvent. Among the animals in the animal house, 12 male rabbits weighing 2.5 kilogrammes or less were selected. The tests (using a mucoadhesive minitablet of CA) and the standard were divided into two groups of six animals each (aqueous suspension of pure drug CA). Every day, they were fed and hydrated with sterile water and food. Before the study, all animals were given a 15 days washout period. The rabbit dosage was determined as follows: For a rabbit weighing 2.5 kg, the total dose (in human) is (250 0.07 2.5)/1.5 = 29.16 mg ≈ for the rabbit of 2.5 kg body weight. With a Ryle’s tube with a diameter of 4 mm, rabbits were given three mucoadhesive minitablets, each containing 10 mg of CA and an aqueous suspension of CA (30 mg). Blood samples of 1 mL were taken from the marginal ear vein at 1, 4, 8, 12, 18 and 24 h after the sample was administered, and the serum samples were used for bio-analytical estimate [14, 17]. The serum concentration versus time plot was used to calculate pharmacokinetic parameters. The peak plasma concentration (Cmax), the area under the curve (AUC) and the time to reach the peak concentration (Tmax) were all determined.
3 Results
3.1 Determination of solubility
Solubility of CA was determined in two solvents, namely distilled water and SGF without enzyme, by saturation solubility. It showed saturation solubility of 0.056 ± 0.002 and 0.121 ± 0.024 mg/mL in distilled water and SGF without enzyme, respectively. It reveals that CA is a poorly soluble drug.
3.2 Fourier transform infrared spectroscopy (FT-IR)
Two carbonyl absorption bands at 1681 cm−1 were observed in CA pure medication, which was attributed to amide carbonyl stretching. In the physical mixing of CA with mucoadhesive polymers chitosan, HPMC K100M and sodium CMC, there were two absorption peaks at 3483 cm−1 and 1778 cm−1, which were attributable to secondary N–H stretching vibration and C=O stretching of vinyl ester, respectively. Figure 4 clearly illustrates that the FT-IR spectra of pure drug and its formulations showed no difference in peak characteristics (observed between group frequency region 1500 and 4000 cm−1), showing that there were no interactions between the drug and the excipients in current study.
3.3 Differential scanning calorimetry (DSC)
With an exothermic peak at 237.71 °C, the DSC thermogram of CA showed an onset or endset temperature of 221.45 °C and 244.03 °C. Latent heat of fusion (H) was discovered to be 49.92 mJ. As a result, CA is shown to be amorphous. Temperatures of 200.03 °C and 228.22 °C were recorded as the onset and endset of the exothermic peak in the DSC thermogram of PM, CA and chitosan-containing CA; the latent heat of fusion was found to be 56.53 mJ. Onset and endset temperatures were 220.40 °C and 248.14 °C, respectively, in the DSC thermogram of PM from CA and HPMC K100M; a value of 56.53 mJ was found to be the latent heat of fusion. For PM of CA and sodium CMC, the DSC thermogram showed an exothermic peak at 216.47 °C; the start and end temperatures, on the other hand, were each at 197.87 °C and 225.91 °C. The latent heat of fusion was found to be 56.53 mJ. All three PM with mucoadhesive polymers chitosan, HPMC K100M and sodium CMC showed no significant change in the exothermic peak of CA. The drug and excipients used in this study are compatible so that the results can be extrapolated. No observable variations in melting point have been noted. DSC spectra are shown in Fig. 5, and they emphasize the fact that there was no difference in exothermic peak characteristics between the pure drug and the formulation, indicating no interactions between the drug and the excipients.
3.4 Preparation of mucoadhesive minitablets
The drug and excipient mixtures were compressed by direct compression using multi-title punches of 3 mm diameter. The batch size of each formulation was 50 minitablets. The prepared minitablets were subjected to various quality control tests.
3.5 Experimental design, optimization and analysis
A three-factor, three-level (33) experimental design was applied for the optimization of process variables and analysis of critical quality attributes (CQAs) [16, 18]. The optimization was performed using the RSM methodology in which PRESS (predicted residual error sum of squares), predicted and experimental values are analysed using statistical analysis using ANOVA. Ultimately, the predicted R2 and adjusted R2 were found out which could afford the statistical data, enduring the model goes significant or not [13,14,15].
3.5.1 Response surface analysis of 2D and 3D plots
3.5.1.1 Effect of the factor on CQA (% of Friability)
Figure 1a, d counter plots (2D and 3D) responses elucidate the impact of observed Responses % friability content upon the polymer concentration. There is a gradual decrease in the chitosan concentration (low level coded value − 1, 0 was embedded in the model), and there is a significant variation in % friability due to its low density, poor flowability and compression characteristics. However, when the level changes from low to high (0, to + 1), i.e. results in a significant increase in polymer concentrations (HPMC K100M and sodium CMC), there is a prevalence of dark green colour region replicating the considerable influence upon % friability of mucoadhesive minitablets.
3.5.1.2 Effect of the factor on CQA (% of drug content)
Figure 1b, d counter plots (2D and 3D) depict that improvement in the polymer concentration upsurges the level of size aggregation, which retards the release behaviour. This, in turn, enhances an optimum % drug content (95–99.5%) specified in the prevalence of the red region. For example, in the case of mucoadhesive minitablets of CA, organized with HPMC K100M polymer, it was perceived that an abundant, desirable sustain release profile of 24 h was achieved with a much lesser proportion of HPMC K100M in comparison with chitosan and sodium CMC.
3.5.1.3 Effect of the factors on CQA (% of mucoadhesive strength)
Figure 1c, f counter plots (2D and 3D) depict those higher values of mucoadhesive strength were detected for chitosan-based mucoadhesive minitablets. In contrast, HPMC K100M indicates reasonable mucoadhesive strength compared with sodium CMC-based minitablets. This can be accredited to chemical bonding and high molecular weight. The % mucoadhesive strength can be altered due to a significant change of high viscoelastic and swellable polymeric properties of HPMCK 100 M rather than others indicated by the prevalence of green colour region.
3.6 Quality control tests for minitablets
The per cent drug content for all the minitablet formulations was in the range of 95 to 99.5%. This high drug content of all minitablets can be attributed to a uniform size and optimum mixing of drugs and excipients. The hardness of the minitablets was in the range of 4.8–5.2 kg/cm2. This ensures the mini-tablet's desirable physical strength to maintain its integrity during its storage and processing. The loss in weight of minitablets in the friability test of all the formulations was less than 0.35%, below the acceptable limit of 1%. The minitablet formulations (F1–F15) passed the weight variation test as the percentage deviation in weight was within the allowable limit of ± 10%. The results of quality control tests for mucoadhesive minitablets are demonstrated in Table 4.
3.7 In vitro dissolution study and release kinetics
The in vitro dissolving study was conducted for all of the prepared minitablet formulations for 24 h. The disintegration rate of mucoadhesive minitablets made with chitosan as a mucoadhesive polymer was shown to be retarded as the chitosan content was increased (F1–F5). The drug concentration in minitablets F1 and F2 could not be sustained for more than 6 h, whereas F3 and F4 could be sustained for up to 12 and 20 h, respectively. Formulation F5, on the other hand, had a favourable sustained release profile, with 100% drug release after 24 h. The viscoelasticity features, swelling index and high molecular weight of the chitosan are responsible for the protracted release (Fig. 6).
3.8 Ex vivo mucoadhesion study
The strong molecular weight (20.000 Daltons), strong viscoelastic capabilities and high swellable polymeric properties are also essential factors that contribute to improved mucoadhesion. The findings are summarized in Table 5 [1].
3.9 Swelling index and percentage of hydration
With increased chitosan concentration, the swelling index (SI) of minitablets increased (F1–F5). Within 0.5 h, F1 had a 59 per cent hydration rate, while F2 had a 98% hydration rate. Within 0.5 h, all other formulations had reached 100% hydration. Therefore, hydration is essential for a mucoadhesive polymer to expand and form a suitable macromolecular mesh and promote mobility in the polymer chains to improve the interpenetration process between the polymer and the mucin. By exposing the bioadhesive sites for hydrogen bonding and electrostatic contact between the polymer and the mucosal network, polymer swelling allows for mechanical entanglement [2]. The swelling index (SI) of all HPMC K100M-based mucoadhesive minitablets (F6 to F10) ranged from 1.363 to 6.739. With increasing concentrations of HPMC K100M, the swelling index (SI) of minitablets increased. Within 0.5 h, all HPMC K100M-based formulations had reached 100% hydration. The percentage of hydration of minitablets increased as the concentration of mucoadhesive polymer (HPMC K100M) was raised, reaching 674 per cent. In addition, the swelling index (SI) of sodium CMC-based mucoadhesive minitablets (F11–F15) ranged from 0.515 to 4.
3.10 Stability study
The stability study for the selected mucoadhesive minitablets showed no significant change in drug content and mucoadhesive strength. Hence, the prepared formulations are stable as per ICH guidelines. The results of stability studies are demonstrated in Table 6.
3.11 Pharmacokinetic study
RP-UFLC measured serum drug concentrations at various time intervals during the pharmacokinetic investigation using an aqueous suspension of CA and a selected mucoadhesive minitablet [14, 15]. Table 7 and Fig. 7 a, b depict the time–concentration relationship between minitablets and the pure medication CA administered to rabbits. The bioavailability (through AUC (ng.h)/mL) was obtained as 19690.11 ± 125.56 for aqueous suspension and 73857.32 ± 314.15 for mucoadhesive minitablets (Table 7). From the calculated results, it was confirmed that cefuroxime axetil minitablet formulation is better and effective than aqueous suspension and to that of pure drug.
4 Discussion
The Box–Behnken experimental design delivers an appropriate means of optimization and testing the robustness of a pharmaceutical method. BBD is a pertinent design with response surface analysis that essentially comprises cube, centre points and axial points. Such differences in points organized the experiments in block prearrangement. The DSC thermogram of CA showed an onset or endset temperatures of 221.45 °C and 244.03 °C, respectively, and an exothermic peak at 237.71 °C. The latent heat of fusion (H) was found to be 49.92 mJ. As a result, CA is shown to be amorphous. The temperature of 200.03 °C and 228.22 °C was recorded as the onset and endset of the exothermic peak in the DSC thermogram of PM, CA and chitosan-containing CA, and the latent heat of fusion was found to be 56.53 mJ. The onset and endset temperatures were found to be 220.40 °C and 248.14 °C, respectively, in the DSC thermogram of PM from CA and HPMC K100M; the latent heat of fusion was 56.53 mJ; for PM of CA and sodium CMC, the DSC thermogram showed an exothermic peak at 216.47 °C; the start and end temperatures, on the other hand, were each at 197.87 °C and 225.91 °C, respectively, and 56.53 mJ was found to be the latent heat of fusion. All three PMs with mucoadhesive polymers chitosan, HPMC K100M and sodium CMC showed no significant change in the exothermic peak of CA. The drug and excipients used in this study are compatible so that the results can be extrapolated. The mucoadhesive minitablets of CA produced with HPMC K100M polymer had a suitable 24-h sustained release profile. The in vitro dissolution data of all the 15 minitablet formulations were subjected to various kinetic equations vis-à-vis zero-order, first-order, Higuchi and Korsmeyer–Peppa’s equations. All the 15 minitablet formulations exhibited Higuchi-order kinetics, as the regression coefficient value (R2) is more in case of Higuchi-order kinetics than others and also the % drug release kinetics irrespective upon the type of mucoadhesive polymer and concentration. All the formulations showed a non-Fickian diffusion-controlled release mechanism for the release of CA from minitablets. The mucoadhesive strength, the force of adhesion and the bond strength of chitosan-based mucoadhesive minitablets were higher.
In contrast, HPMC K100M and sodium CMC-based minitablets had lower values. This could be due to chemical bonding or physical entanglement of the enlarged polymer with mucin, resulting in enhanced mucoadhesion. With the increasing concentrations of HPMC K100M, minitablets swelling index (SI) increased. Within 0.5 h, all HPMC K100M-based formulations had reached 100% hydration. The percentage of hydration of minitablets increased as the concentration of mucoadhesive polymer (HPMC K100M) was raised, reaching 67.4%. The swelling index (SI) of sodium CMC-based mucoadhesive minitablets (F11–F15) ranged from 0.515 to 4. When sodium CMC concentration was raised, minitablets swelling index (SI) also increased. Within 0.5 h, F11 had a 51% hydration rate, while F12 showed an 80% hydration rate. Within 0.5 h, all other formulations had reached 100% hydration. The percentage of hydration of minitablets increased as the concentration of mucoadhesive polymer (sodium CMC) was raised to 400%. Aqueous suspension of CA was shown to have a Tmax of 4 h, but the selected mucoadhesive minitablet had 3.0 times greater, indicating increased activity. The AUC for mucoadhesive minitablets was 3.75 times higher than for CA aqueous suspension. A possible explanation for this is mucoadhesion of minitablets in the proximal section of the gastrointestinal tract (GI). The higher MRT value for the mucoadhesive minitablet indicated that the medicine had a more extended period to be absorbed before it was removed from the body. The selected mucoadhesive minitablets' pharmacokinetic profile was superior to that of CA aqueous suspension, allowing both therapeutic and commercial applications. Finally, the mucoadhesive minitablets containing HPMC K100M and chitosan considerably enhanced the bioavailability of CA.
5 Conclusions
The current study concluded that mathematical data analysis was performed to fit the two-factor interaction model, and optimized mucoadhesive mini-tablet formulations were considered. The run 8 (− 1, 0, + 1 levels obtained in 33 experimental design) demonstrated a desirable and promising release profile for 24 h when compared with other formulations, specifying that it is the optimized run as the concentration of blends of chitosan, HPMC K100M and sodium CMC for the best mucoadhesive combination polymers as per response surface analysis (outlined in perturbation plots, predicted vs. actual value aided counter plot elucidations, as well as point prediction data’s obtained through solutions of graphical optimizations). The optimized run is applicable to formulate CAs minitablets as it reflects a higher percentage of drug content, mucoadhesion and swelling index. As a result, it can be concluded that the developed formulation is suitable for estimating CA in the formulated mucoadhesive minitablets.
Availability of data and materials
The data that support the findings of this study are included in the article.
Abbreviations
- AUC:
-
Area under the curve
- BBD:
-
Box–Behnken design
- CA:
-
Cefuroxime axetil
- C max :
-
Maximum concentration
- H:
-
Hour
- QbD:
-
Quality by design
- T max :
-
Maximum time
- UFLC:
-
Ultra-fast liquid chromatography
- UV:
-
Ultra-violet spectroscopy
References
Palem CR, Dudhipala NR, Battu SK, Repka MA, Rao Yamsani M (2016) Development, optimization and in vivo characterization of domperidone-controlled release hot-melt-extruded films for buccal delivery. Drug Dev Ind Pharm 42(3):473–484. https://doi.org/10.3109/03639045.2015.1104346
Gu JM, Robinson JR, Leung SH (1988) Binding of acrylic polymers to mucin/epithelial surfaces: structure-property relationships. Crit Rev Ther Drug Carrier Syst 5(1):21–67
Kumar V, Pavan N, Gupta V (2015) A review on quality by design approach (QBD) for pharmaceuticals. Int J Drug Dev Res 7:52–60
Bhise J, Bhusnure GJO, Shrikrishna TM, Mujewar IN, Gholve SB, Jadhav PU (2019) A review on quality by design approach (QBD) for pharmaceuticals. J Drug Deliv Ther 9(3-s):1137–1146
Yu LX (2008) Pharmaceutical quality by design: product and process development, understanding, and control. Pharm 25(4):781–791
Swain S, Parhi R, Jena BR, Babu SM (2019) Quality by design: concept to applications. Curr Drug Discov Technol 16(3):240–250
Jena BR, Panda SP, Umasankar K, Swain S, Rao Koteswara GSN, Damayanthi D, Ghose D, Pradhan DP (2021) Applications of QbD-based software’s in analytical research and development. Curr Pharm Anal 17(4):461–473
Jena BR, Panda SP, Umasankar K, Alavala RR, Rao GSNK, Swain S, Ghose D, Pattnaik G, Pradhan DP (2021) Analytical QbD based systematic development of a novel RP-UHPLC method for quantification of albuterol sulphate in its metered dose inhaler formulations. J Res Pharm 25(5):689–701
Khutoryanskiy VV (2011) Advances in mucoadhesion and mucoadhesive polymers. Macromol Biosci 11:748–764. https://doi.org/10.1002/mabi.201000388
Ferreira LMB, dos Santos AM, Boni FI, dos Santos KC, Robusti LMG, de Souza MPC, Ferreira NN, Carvalho SG, Cardoso VM, Chorilli M et al (2020) Design of chitosan-based particle systems: a review of the physicochemical foundations for tailored properties. Carbohydr Polym 250:116968
Sogias IA, Williams AC, Khutoryanskiy VV (2008) Why is chitosan Mucoadhesive? Biomacromol 9:1837–1842
https://www.sciencedirect.com/topics/neuroscience/hydroxypropylmethylcellulose.
Kowalczuk J, Tritt-Goc J, Piślewski N (2004) The swelling properties of hydroxypropyl methyl cellulose loaded with tetracycline hydrochloride: magnetic resonance imaging study. Solid State Nucl Magn Reson 25(1–3):35–41. https://doi.org/10.1016/j.ssnmr.2003.03.016
Ghose D, Patra CN, Ravi Kumar BVV, Swain S, Jena BR, Choudhury P, Shree D (2021) QbD-based formulation optimization and characterization of polymeric nanoparticles of cinacalcet hydrochloride with improved biopharmaceutical attributes. Turk J Pharm Sci 18(4):452–464. https://doi.org/10.4274/tjps.galenos.2020.08522
Roy S (2012) Quality by design-holistic concept of concept of building quality in pharmaceuticals. Int J Pham Biomed Res 3:100–108
Swain S, Jena BR, Madugula D, Beg S (2019) Application of quality by design paradigms for development of solid dosage forms. In: Beg S, Hasnain S (eds) Pharmaceutical quality by design; principles and applications. Elsevier Academic Press, Cambridge, pp 109–130
Conti S, Maggi L, Segale L, Machiste EO, Conte U, Grenier P, Vergnault G (2007) Matrices containing Na CMC and HPMC: swelling and release mechanism study. Int J Pharm 333:143–151. https://doi.org/10.1016/j.ijpharm.2006.11.067
Bezerra MA, Santelli RE, Oliveira EP, Villar ELSLA (2008) Response surface methodology (RSM) as a tool for optimization in analytical chemistry. Talanta 76:965–977. https://doi.org/10.1016/j.talanta.2008.05.019
Acknowledgements
The authors are acknowledged to the central instrumentation facility of Roland Institute of Pharmaceutical Sciences, Berhampur, Odisha, India, for the technical support.
Funding
None.
Author information
Authors and Affiliations
Contributions
SS designed the study and critically revised the manuscript for additional valuable content. JP performed the experiments, analysed and interpreted the data and drafted the manuscript. MBR, CNP and BRJ revised and designed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Panda, J., Rao, M.E.B., Swain, S. et al. Formulation development, optimization and characterization of mucoadhesive minitablets of cefuroxime axetil: in vitro, ex vivo and in vivo pharmacokinetic evaluation. Beni-Suef Univ J Basic Appl Sci 11, 123 (2022). https://doi.org/10.1186/s43088-022-00303-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43088-022-00303-2