Abstract
Introduction and importance
Choledochal cysts are congenital conditions that affect the biliary tree, typically identified during childhood. These cysts present as dilations in the biliary system, occurring either in the extrahepatic or intrahepatic regions or in some cases, in both areas. Occasionally, it may have associated chronic pancreatitis posing a challenge to the management of both conditions.
In the case reported, a female child was diagnosed with a choledochal cyst along with chronic pancreatitis. She had an excision of cyst and lateral pancreaticojejunostomy simultaneously for both conditions resulting in favorable outcomes.
Case presentation
An 8-year-old child visited the clinic with a complaint of upper abdominal pain accompanied by intermittent vomiting. An ultrasound was performed which showed a dilated common bile duct. To confirm the diagnosis, an MRCP and baseline labs including liver function tests were ordered. The findings were suggestive of a type IA choledochal cyst with concomitant chronic pancreatitis. Subsequently, she had choledochal cyst excision with Roux-en-Y hepaticojejunostomy reconstruction plus lateral pancreaticojejunostomy using the classical Puestow’s technique. The patient’s recovery post-surgery was uneventful, resulting in discharge on the fifth post-operative day for routine outpatient follow-up.
Clinical discussion
Patients afflicted with choledochal cysts are prone to recurrent pancreatitis, though the precise underlying mechanism is unknown. Certain studies propose an association between abnormal pancreatico-biliary junction and recurrent pancreatitis, often defined as a common channel surpassing 15 mm in length. However, this aberration could not be definitively established in the current case. Diagnosis of choledochal cysts can be confirmed through either ERCP or MRCP, with the latter preferred due to its non-invasive nature. The optimal management strategy for choledochal cysts necessitates cyst resection and Roux-en-Y hepaticojejunostomy reconstruction Moreover, in cases associated with chronic pancreatitis, longitudinal pancreatojejunostomy may be undertaken.
Conclusion
Thus, it is concluded that although rare choledochal cysts may have associated chronic pancreatitis. Surgical excision of the cyst and lateral pancreaticojejunostomy can be performed simultaneously resulting in favorable post-operative outcomes.
Similar content being viewed by others
Introduction
Choledochal cysts constitute a congenital condition characterized by cystic dilations affecting both intrahepatic and extrahepatic biliary ducts. Although rare, this condition impacts approximately 1 in every 100,000 to 150,000 births [1]. Typically emerging during childhood, it manifests with symptoms such as abdominal pain. The risk of biliary tract carcinoma increases significantly, ranging from 2.5 to 17.5%, a stark contrast to the general population's risk of 0.01 to 0.05% [2]. Complications of choledochal cysts also encompass pancreatitis, cholangitis, and spontaneous cyst rupture.
The primary mode of treatment involves surgical removal of the cyst and subsequent biliary system reconstruction. Although the most frequently documented association in the genesis of choledochal cysts is an anomalous pancreato-biliary junction (APBJ) [3, 4], the presence of an associated pancreatic ductal dilation remains an infrequent occurrence. The inaugural documented case of a choledochal cyst concomitant with chronic pancreatitis dates back to 1991, and its management involved a pylorus-preserving pancreaticoduodenectomy [5]. The recurrent bouts of pancreatitis can lead to dilated pancreatic ducts and calculi, representing a recognized complication found in 11.9% of patients with choledochal cysts [3].
In cases where pain is the primary complaint, addressing pancreatic ductal drainage simultaneously through procedures like pancreatojejunostomy, may yield substantial advantages.
This case has been reported in line with Surgical CAse REport (SCARE) 2020 Guidelines [6].
Case report
Presentation and evaluation
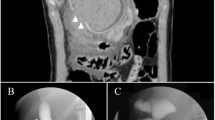
An 8-year-old female patient visited the outpatient clinic in January 2023, reporting persistent upper abdominal pain accompanied by intermittent vomiting spanning 4 years. Subsequent evaluation by ultrasonography raised the suspicion of a choledochal cyst. Magnetic resonance cholangiopancreatography (MRCP) was performed, revealing a type IA choledochal cyst measuring 5.5 cm in a fusiform configuration. This cyst exhibited mild dilatation in the intrahepatic ducts, cystic duct (0.8 cm), and pancreatic duct (0.7 cm), with multiple stones detected within the pancreatic duct, the largest measuring 0.5 cm (Fig. 1A, B). Laboratory investigations indicated amylase levels of 45 IU/L, total bilirubin at 0.5 mg/dL, direct bilirubin at 0.18 mg/dL, alkaline phosphatase at 158 IU/L, ALT at 47 IU/L, AST at 53 IU/L, and GGT at 167 IU/L.
To further assess the pancreatic duct and potentially decompress the system, an endoscopic retrograde cholangiopancreatography (ERCP) was performed. During this procedure, the pancreatic duct was stented using a 5-Fr 3-cm-long pigtail catheter. However, cannulation of the common bile duct (CBD) was impeded by an anomalous lengthy common channel.
Operative management
Subsequently, the patient was scheduled for choledochal cyst resection along with Roux-en-Y hepaticojejunostomy reconstruction. Additionally, longitudinal pancreatojejunostomy was performed using the classical Puestow’s technique. Intraoperatively, a choledochal cyst measuring approximately 8 cm in diameter, was identified. This cyst extended from the confluence of the right and left hepatic ducts to the anomalous pancreato-biliary junction (type IA), encased by extensive inflammation and adhesions. The procedure also revealed an anomalous right hepatic arterial system, with the superior mesenteric artery bifurcating into two extrahepatic branches, overlaying the cystic duct.
The Puestow procedure was carried out, incorporating a two-layer anastomosis utilizing 5/0 polydioxanone for the internal layer and 5/0 polypropylene for the external layer sutures. The hepaticojejunostomy was accomplished through a single layer of 5/0 polydioxanone suture (Fig. 2A, B).
Post-operative course
The patient’s recovery post-surgery was uneventful, resulting in discharge on the fifth post-operative day for routine outpatient follow-up. Over the ensuing 6 months, the patient reported a reduction in pain and regained the ability to participate in regular activities unrestrictedly.
Discussion
Patients afflicted with choledochal cysts are prone to recurrent pancreatitis, though the precise underlying mechanism is unknown. Certain studies propose an association between the abnormal pancreatico-biliary junction and recurrent pancreatitis, often defined as a common channel surpassing 15 mm in length [7, 8]. However, this aberration could not be definitively established in the current case.
As per the modified Todani classification system, the cyst in this instance aligns with type IA, representing the most prevalent subtype [9]. Diagnosis of choledochal cysts can be confirmed through either ERCP or MRCP, with the latter preferred due to its non-invasive nature. The clinical association found in earlier studies indicated a higher incidence of pancreatitis in children and females, as well as in those patients having larger cysts (> 5 cm) [10,11,12]. Other common clinical features of choledochal cysts include abdominal pain and/or jaundice, often accompanied by normal liver function tests, amylase levels, and the absence of distal biliary or intrahepatic strictures in most instances. In this case, raised amylase levels were likely due to associated chronic pancreatitis.
The optimal management strategy for choledochal cysts necessitates cyst resection and Roux-en-Y hepaticojejunostomy reconstruction to alleviate bile stasis and circumvent exposure to bile and pancreatic secretions. Moreover, in cases associated with chronic pancreatitis, longitudinal pancreatojejunostomy may be undertaken to drain a dilated pancreatic duct. This becomes especially relevant when linked to pain and the presence of ductal calculi or calcification, as it may ameliorate symptoms. The Puestow procedure, recognized for its low morbidity [13] and positive outcomes, may be favored in combination with hepaticojejunostomy for patients with choledochal cysts.
Conclusion
The successful management of this 8-year-old female patient involved the simultaneous surgical excision of the cyst and lateral pancreaticojejunostomy. This integrated approach not only addressed the primary concern but also effectively managed the secondary complication of chronic pancreatitis.
The favorable post-operative outcomes, including the patient’s reported reduction in symptoms and the resumption of regular activities, highlight the importance of prompt diagnosis and comprehensive surgical treatment in cases of choledochal cysts with associated conditions.
Availability of data and materials
Not applicable.
Abbreviations
- MRCP:
-
Magnetic resonance cholangiopancreatography
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- CBD:
-
Common bile duct
- APBJ:
-
Anomalous pancreato-biliary junction
References
Bhavsar MS, Vora HB, Giriyappa VH (2012) Choledochal cysts: a review of literature. Saudi J Gastroenterol 18:230–236
Benhidjeb T, Munster B, Ridwelski K, Rudolph B, Mau H, Lippert H (1994) Cystic dilatation of the common bile duct: surgical treatment and long-term results. Br J Surg 81:433–436
Tashiro S, Imaizumi T, Ohkawa H et al (2003) Pancreaticobiliary maljunction: retrospective and nationwide survey in Japan. J Hepatobiliary Pancreat Surg 10:345–351. https://doi.org/10.1007/s00534-002-0741-7
Hamid R, Bhat NA, Ahmad M, Singh B. Choledochal Cyst (CDC) (2018) Gastrointestinal Surgery - New Technical Proposals. https://doi.org/10.5772/intechopen.72938
Yamataka A, Segawa O, Kobayashi H, Kato Y, Miyano T (2000) Intraoperative pancreatoscopy for pancreatic duct stone debris distal to the common channel in choledochal cyst. J Pediatr Surg 35(1):1–4
Agha RA, Franchi T, Sohrabi C, et al. for the SCARE Group (2020) The SCARE2020 Guideline: updating consensus Surgical CAse REport (SCARE)guidelines. Int J Surg, 84:226–30
Babbitt DP, Starshak RJ, Clemett AR (1973) Choledochal cyst: a concept of etiology. Am J Roentgenol Radium Ther Nucl Med 119:57–62
Jalleh RP, Williamson RC (1991) Choledochal cyst and chronic pancreatitis-treated by proximal pancreatectomy. HPB Surg 4:245–250
Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K (1977) Congenital bile duct cysts: classification, operative procedures, and review thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 134:263–269
Swisher SG, Cates JA, Hunt KK, Robert ME, Bennion RS, Thompson JE et al (1994) Pancreatitis associated with adult choledochal cysts. Pancreas 9:633–637
Komuro H, Makino SI, Yasuda Y, Ishibashi T, Tahara K, Nagai H (2001) Pancreatic complications in choledochal cyst and their surgical outcomes. World J Surg 25:1519–1523
Suchy FJ (2010) Pediatric disorders of the bile ducts. In: Feldman M, Friedman LS, Brandt LJ (eds) Sleisenger and Fordtran’s Gastrointestinal & Liver Disease II, 9th edn. WB Saunders, Philadelphia, pp 1052–62
Napolitano M, Brody F, Lee KB, Rosenfeld E, Chen S, Murillo-Berlioz AE, Amdur R (2020) 30-day outcomes and predictors of complications after Puestow procedure. Am J Surg 220(2):372–375
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: HB, AA. Data curation: HB, AA Methodology: HB. Visualization: HB, AA. Writing—original draft: MAK. Writing—review and editing: HB, AA, MAK. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Written informed consent was obtained from the patient's parents for publication and any accompanying images.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bashir, H., Abbas, A. & Khan, M.A. Simultaneous choledochal cyst excision and pancreaticojejunostomy (Puestow’s technique) for type IA cyst with associated chronic pancreatitis: a case report. Egypt Liver Journal 14, 62 (2024). https://doi.org/10.1186/s43066-024-00369-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-024-00369-w