Abstract
Introduction
Given that ERCP has major procedure-related complications in non-cirrhotic patients, the complications and the cost of therapeutic ERCP were not studied in cirrhotic patients.
Aim
We aimed to study the complications and cost of ERCP compared to patients without cirrhosis.
Patients and methods
Outcome and complications of therapeutic ERCP were prospectively studied in patients with cirrhosis and compared to patients without cirrhosis undergoing ERCP. Patients with cirrhosis were evaluated using the Child-Pugh classification, MELD, MELD Na, and APRI scores. Safety was assessed up to 30 days following the procedure.
Results
Pancreatitis, perforation, bleeding, and cardiopulmonary complications were not different in both groups (8% vs. 9.3, 0% vs. 2%, 3.3% vs. 4%, and 4% vs. 2% respectively), while cholangitis occurred more frequently in cirrhosis (13.3% vs. 1.3% respectively). Hospital stay was longer, and mortality and costs were significantly higher among patients with cirrhosis. Patients with Child C cirrhosis developed more complications and had higher mortality. A MELD score cut-off of ≥ 11.5 separated all mortalities. Similarly, MELD-Na and APRI separated patients with cirrhosis who had more frequent complications and mortalities.
Conclusions
Patients with cirrhosis experienced more complications and costs, and cirrhotic patients who developed moderate to severe complications were more likely to die.
Similar content being viewed by others
Introduction
Since its introduction in the sixties of the last century, ERCP has come to be the preferred therapeutic modality for many biliary and pancreatic diseases [1]. However, due to its major and sometimes catastrophic complications, and with the advances in imaging technology and endoscopic ultrasound, non-invasive imaging techniques are preferred as diagnostic tools, except in cases where intra-ductal biopsy, intra-ductal ultrasound, and or cholangioscopy are indicated. Liver cirrhosis is associated with a disturbed coagulation profile and thrombocytopenia, which can contribute to bleeding with invasive procedures. The impaired immune function of patients with cirrhosis and the CBD manipulation during ERCP increase the risk factors for bacterial cholangitis, peritonitis, hepato-renal syndrome, and hepatic encephalopathy [2, 3].
Because of disease-related complications of cirrhosis, varieties of scores have been derived to estimate the prognosis of patients with cirrhosis to identify patients who are at risk of morbidity and mortality. The practical advantages of these scores include their noninvasiveness, widespread availability, and reproducibility.
Child score was introduced as an index of liver disease severity and prognosis. Elements of the Child score include bilirubin, albumin, ascites, and encephalopathy; although it is simple in the evaluations of the liver condition, it has been affected by its fallibility to subjective assessment (ascites and encephalopathy), and the ceiling effects are affected by extraneous factors (e.g., diuretics) [4].
Many years ago, the model of end-stage liver disease (MELD) score was proposed as an objective predictor of short-term mortality among patients with cirrhosis undergoing transjugular intrahepatic portosystemic shunt placement [5]. Its simplicity and availability make it widely accepted for the assessment of liver disease including medical urgency and organ allocation.
Several prognostic scores are used to predict prognosis prior to operative intervention in patients with cirrhosis, such as the Child-Turcotte-Pugh classification and the MELD and MELD Na scores. Different scores were used in a few studies with few numbers of patients to predict complications in patients with cirrhosis undergoing ERCP, and large prospective controlled studies are lacking. The cost analysis of ERCP was not studied previously in patients with cirrhosis.
Aim of the study
We aimed to assess the safety, costs, and feasibility of the ERCP procedure in patients with cirrhosis versus patients without cirrhosis additionally, to evaluate different function and fibrosis scores to predict post-procedure-related complications in patients with cirrhosis.
Patients and methods
Study design
Patients
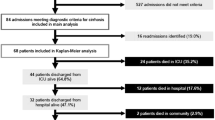
Patients with liver cirrhosis undergoing ERCP for obstructive jaundice were prospectively included. Matched case-control patients without cirrhosis undergoing ERCP for the same indication were included in the same period. From December 2019 to June 2021, 150 patients with cirrhosis underwent ERCP, and a similar number without cirrhosis were included.
Methods
Baseline data obtained included history, clinical examination, liver tests, renal tests, blood count, INR, and abdominal ultrasonography. MRCP or abdominal CT was ordered when indicated.
All patients with cirrhosis were additionally evaluated by using the Child-Turcotte-Pugh classification, model of end-stage liver disease (MELD), and MELD Na scores and aspartate aminotransferase to platelet ratio index (APRI) [4,5,6,7]. Cirrhosis was diagnosed if any of the following showed confirmed its presence at any time before the procedure: liver biopsy result showing > F3 fibrosis on the Metavir score, radiological or endoscopic evidence of portal hypertension, or non-invasive liver fibrosis test (transient elastography > 12.5 kPa or FIB-4 > 3.25) [8].
Endoscopic procedures
Pre-procedure medications
All patients were well hydrated and received prophylactic broad-spectrum intravenous antibiotics (cefoperazone 1 g every 12 h) before the procedure. Antibiotic administration started 1 day before the procedure and continued for 72 h after the procedure.
Four units of fresh frozen plasma were given if the INR was more than 1.8.
Platelet transfusion was done if the platelet count was less than 30,000 per microliter (mcL).
ERCP
ERCP was done under propofol anesthesia for all patients. Olympus side-viewing duodenoscope (TJF190VR, Olympus, Tokyo, Japan) was used for all procedures. Zebra J-tip or straight tip guide wire (0.35/400 cm) was advanced through triple lumen papillotome (both Boston Scientific Corp, Massachusetts, USA), and the guide wire was advanced through malignant stenosis if present.
After attaining selective bile duct cannulation using guide wires, a cholangiogram was done under fluoroscopic guidance. Therapeutic interventions were done according to the findings during the procedure. These included sphincterotomy, precut sphincterotomy, sphincteroplasty, stone extraction (with balloons or baskets), stricture dilatation, insertion of pancreatic and/or biliary plastic stents, biliary metal stents, and insertion of nasobiliary tubes.
Outcome measures
We evaluated the following outcome measures: successful cannulation, successful drainage, stone extraction, stent placement, and ERCP-related complications.
Intervention was considered effective with drop of serum bilirubin to less than 3 g/dl within 30 days’ stent occlusion, or primary non-functioning was defined as the persistence of jaundice or bilirubin level of more than 5 mg/dL, alkaline phosphatase, GGT, and transaminases 3 times the normal values and/or dilated bile ducts by ultrasound and/or CT follow-up indicating re-endoscopy [9,10,11].
Procedure-related morbidity and mortality were defined as complications or deaths directly related to the ERCP procedure within 1 month. Cholangitis, a month post-ERCP, was considered procedure-related.
Follow-up
Patients were evaluated clinically and by laboratory investigations at day 1, day 3, day, 7, and day 30 after the procedure.
Determination of costs
-
A.
Direct cost was estimated by determination of direct hospitalization costs for every patient (fees of specialist and consultant, imaging cost, laboratory investigations (liver profile, renal profile, and INR), procedure cost, and repeated procedure to treat complications, and cost for hospital admissions)
-
B.
Indirect cost was estimated by determination of time lost away from productivity and activity and the times spent for procedures, hospitalization, visits for consolations, and investigations multiplied by 100 Egyptian pounds for every day
Statistical analysis of the data
Data were fed to the computer and analyzed using the IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Qualitative data were described using numbers and percentages. Quantitative data were described using range (minimum and maximum), mean, standard deviation, and, median. The significance of the obtained results was judged at the 5% level.
The used tests were as follows:
-
1.
Chi-square test: for categorical variables, between different groups
-
2.
Fisher’s exact: correction for chi-square when more than 20% of the cells have an expected count of less than 5
-
3.
Student t-test: for normally distributed quantitative variables, to compare two studied groups
-
4.
Mann-Whitney test: for abnormally distributed quantitative variables, to compare two studied groups
-
5.
Receiver operating characteristic curve (ROC): it is generated by plotting sensitivity (TP) on the Y-axis versus 1-specificity (FP) on the X-axis at different cut-off values. The area under the ROC curve denotes the diagnostic performance of the test. An area of more than 50% gives acceptable performance, and an area of about 100% is the best performance for the test. The ROC curve allows also a comparison of performance between two tests
Results
The study included 150 patients with cirrhosis and obstructive jaundice (60% males, mean age 60 ± 12.4 years); 35 patients were Child A, 67 patients were Child B, and 48 patients were Child C, and 150 matched patients were with obstructive jaundice without cirrhosis (56% males, mean age 52.4 ± 20.3 years). Tables 1 and 2 show the patients’ baseline characteristics and laboratory data. Patients with cirrhosis were older and had less hypertension and ischemic heart disease than patients without cirrhosis. They also had lower hemoglobin and platelets and higher bilirubin and INR.
Table 3 shows the indications for ERCP and the therapeutic interventions performed. Patients without cirrhosis more often had ERCP for stone obstruction of the CBD, and patients with cirrhosis had more malignant obstruction of the CBD or CHD. Biliary cannulation was successful in 98% and 98.3% of patients with and without cirrhosis, and consequently, patients with cirrhosis had more stents placed and patients without cirrhosis had more stones extracted.
Table 4 shows the adverse events and complications in the study groups. Clinical pancreatitis, perforation, bleeding, and cardiopulmonary complications were not different in patients with and without cirrhosis, while cholangitis occurred more frequently in patients with cirrhosis (13.3% vs. 1.3% respectively). Hospital stay was longer, and mortality was significantly higher among patients with cirrhosis. Patients with Child C cirrhosis developed more complications and had higher mortality. The causes of death are listed in Table 5.
Table 6 shows the correlation between rates of complications and severity of liver cirrhosis. CTP class A patients experienced fewer overall complications and mortality than class B and C patients (3.3% morbidity and 0.0% mortality vs. 15.7% and 28% for class B and 26.7% and 72% for CTP C).
At the MELD score cut-off of ≤ 11.5, 4% of patients developed complications, and no mortalities occurred, while at a score of > 11.5, 41% of patients developed complications, and all mortalities occurred. At MELD-Na scores of ≤ 21.13, the complications and mortalities were 12.7% and 20%, and at a cut-off of > 21.13, the rates were 32.7% and 80%. With the APRI at a level of ≤ 1.49 and > 1.49, the complication and mortalities were 19.3% and 32% and 26% and 68%, respectively. Applying the New Wilson Index, a score of ≤ 5 and > 5 showed 5.3% and 16% and 40% and 84% morbidity and mortality, respectively (Figs. 1, 2, and 3).
Discussion
In this study, we demonstrate that pancreatitis as a complication of therapeutic ERCP was not more frequent in patients with cirrhosis. Several previously published studies reported no association between the presence of cirrhosis and pancreatitis as a complication of ERCP, except when alcohol is the underlying cause of cirrhosis [12]. However, Inamdaret al. found a significant association of post-ERCP pancreatitis with decompensated cirrhosis, which they attributed to the accumulation of administered intravenous fluids in the third space due to portal hypertension [13].
Although cirrhosis is not among the risk factors of ERCP-related pancreatitis, it is strongly linked to post-procedure bleeding. Thrombocytopenia, congestive duodenopathy, and coagulopathies are independent risk factors for bleeding. In this series, bleeding in patients with cirrhosis occurred less frequently than in patients without cirrhosis. However, procedure-related bleeding from the papilla after papillotomy occurred more in patients with cirrhosis. Variable rates of post-ERCP bleeding were previously reported [3, 12,13,14,15], with increased bleeding rates with increased severity of cirrhosis (from 2.1 to 25%) [3, 5, 6]. On the other hand, other studies reported no significant association found between post-sphincterotomy complications and severity of liver cirrhosis [15,16,17,18].
Although INR is the most commonly used test to assess the possibility of bleeding prior to operative procedure, we found no significant association between a higher INR and the development of bleeding post-ERCP, similar to several previous reports [2, 10, 18,19,20,21]. This might be explained by the precarious rebalanced hemostatic state caused by decreased synthetic power of the cirrhotic liver to produce both anticoagulant and pro-coagulant proteins [22,23,24]. However, Adler et al. avoid ERCP if the INR is > 1.7 [15]. The use of fresh frozen plasma has been shown not to reduce the risk of bleeding even with the use of standard rates of transfusions [18, 25]. The discrepancy in bleeding rates between different studies has been attributed to the differences in the characteristics of studied patients and the type of procedures.
Cardiopulmonary complications are among the major hazards post-ERCP. In our study, patients with cirrhosis developed more cardio-pulmonary complications than patients without cirrhosis, but this was not significant. With the progress of liver disease, concomitant progress of cardiac dysfunction occurs [26,27,28], with reduced ejection fraction [26,27,28] and the possibility of the associated hepato-pulmonary syndrome, portopulmonary hypertension, and hepatic hydrothorax as added risk factors [29].
In our study, cholangitis developed in 13.3% of patients with cirrhosis versus 1.3% of patients without cirrhosis. Other studies reported variable rates of cholangitis [2, 15]. Possible explanation of increased post-ERCP cholangitis is bacterial translocation caused by bile duct manipulation especially when the biliary drainage is incomplete [30, 31]. Poor immune function and portal bacteremia are possible added factors. The lower rates of cholangitis in other studies may be attributed to their retrospective nature, variability of diagnostic code, and that these studies captured only the data base of hospitalized patients.
In this report, there was a higher rate and severity of morbidity and higher mortality rate in patients with cirrhosis. Infection and cholangitis represented the major cause of mortality among patients with cirrhosis. The increased rates of morbidity and mortality in patients with cirrhosis reflected on the length of hospital stay.
We evaluated the risk stratification of procedure-related complications in patients with cirrhosis using Child-Turcotte-Pugh classification, the MELD and MELD-Na scores, APRI, and the New Wilson index.
CTP class A patients experienced less overall complications and mortality than class B and C patients. Similarly, a MELD score ≤ 11.5 categorized patients with 4% morbidity and no mortalities. Similar results were previously reported [12,13,14]. The MELD-Na score and APRI also segregated patients with low vs. high risk of morbidity and mortality.
The overall percentage of mortality in patients with cirrhosis was 16.7. Causes of mortality were pancreatitis, cardiopulmonary, bleeding, cholangitis, and hepato-renal syndrome, all occurring in the setting of moderate to severe complications. Lower rates of mortality in patients with cirrhosis were reported in other studies [21, 23]; however, these studies were retrospective analyses, and the cause of death was obtained by telephone. Our study was prospective, and patients were followed up for 1 month following the procedure.
The increased bilirubin in patients with cirrhosis with obstructive jaundice is not linearly related to the severity of liver cirrhosis and is partly caused by biliary obstruction. This is a limitation of our study and other studies that use the Child-Turcotte-Pugh classification and the MELD and MELD Na scores, where bilirubin is one of the measurable variables in these scores.
The strengths of our study include its prospective nature the inclusion of patients without cirrhosis as a comparator group, and the several scores we used for risk stratification plus the direct and indirect costs were calculated in both groups.
In conclusion, ERCP is safe in patients with cirrhosis; however, these patients experienced more complications and costs than patients without cirrhosis. Patients with more advanced liver disease were more likely to develop complications, and patients who developed moderate to severe complications were more likely to die. Hospital stay and costs were more in patients with cirrhosis.
Availability of data and materials
Please contact the author for data requests.
Abbreviations
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- DM:
-
Diabetes mellitus
- IHD:
-
Ischemic heart disease
- HTN:
-
Hypertension
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate transaminase
- ALK:
-
Alkaline phosphatase
- GGT:
-
Gamma-glutamyl transpeptidase
- HCV:
-
Hepatitis C virus
- HBV:
-
Hepatitis B virus
- INR:
-
International normalization ratio
References
McCune WS, Shorb PE, Moscovitz H (1968) Endoscopic cannulation of the ampulla of Vater: a preliminary report. Gastrointest Endosc 34(3):278–280
Park DH, Kim MH, Lee SK et al (2004) Endoscopic sphincterotomy vs. endoscopic papillary balloon dilation for Choledocholithiasis in patients with liver cirrhosis and coagulopathy. Gastrointest Endosc 60:180–185
Kröner PT, Bilal M, Samuel R et al (2020) Use of ERCP in the United States over the past decade. Endosc Int Open 08:E761–E769
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R (1973) Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 60:646–649
Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, ter Borg PC (2000) A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31:864–871
Kim WR, Biggins SW, Kremers WK, Wiesner RH, Edwards E, Therneau TM (2008) Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med 359(10):1018–1026. https://doi.org/10.1056/nejmoa0801209
Lin ZH, Xin YN, Dong QJ et al (2011) Performance of the aspartate aminotransferase-to-platelet ratio index for the staging of hepatitis C-related fibrosis: an updated meta-analysis. Hepatology 53(3):726–735
Hong H, Li J, Jin Y, Li Q, Li W, Wu J, Huang Z (2014) Performance of real-time elastography for the staging of hepatic fibrosis: a meta-analysis. PLoS One 9(12):e115702
Navaneethan U, Njei B, Zhu X et al (2017) Safety of ERCP in patients with liver cirrhosis: a national database study. Endosc Int Open 05:E303–E314
Yoon WJ, Lee JK, Lee KH et al (2006) A comparison of covered and uncovered wall stents for the management of distal malignant biliary obstruction. Gastrointest Endosc 63:996–1000
Paik WH, Park YS, Hwang JH et al (2009) Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach. Gastrointest Endosc 69:55–62
Navaneethan U, Njei B, Zhu X, Kommaraju K, Parsi MA, Varadarajulu S (2017) Safety of ERCP in patients with liver cirrhosis: a national database study. Endosc Int Open 5(4):E303–E314
Inamdar S, Berzin TM, Berkowitz J et al (2016) Decompensated cirrhosis may be a risk factor for adverse events in endoscopic retrograde cholangiopancreatography. Liver Int 36(10):1457–1463
Li DM, Zhao J, Zhao Q et al (2014) Safety and efficacy of endoscopic retrograde cholangiopancreatography for common bile duct stones in liver cirrhotic patients. J Huazhong Univ Sci Technol Med Sci 34:612–615
Adler DG, Haseeb A, Francis G et al (2016) Efficacy and safety of therapeutic ERCP in patients with cirrhosis: a large multicenter study. Gastrointest Endosc 83:353–359
AdikeaA, Al-QaisiaM, Baffya J., , et al, International normalized ratio does not predict gastrointestinal bleeding after endoscopic retrograde cholangiopancreatography in patients with cirrhosis. Gastroenterol Res 2017; 10(3):177-181
Zhang J, Ye L, Zhang J et al (2015) MELD scores and Child-Pugh classifications predict the outcomes of ERCP in cirrhotic patients with choledocholithiasis: a retrospective cohort study. Medicine (Baltimore) 94(3):e433
Townsend JC, Heard R, Powers ER, Reuben A (2012) Usefulness of international normalized ratio to predict bleeding complications in patients with end-stage liver disease who undergo cardiac catheterization. Am J Cardiol 110(7):1062–1065
Mahmoud AM, Elgendy IY, Choi CY, Bavry AA (2015) Risk of bleeding in end-stage liver disease patients undergoing cardiac catheterization. Tex Heart Inst J 42(5):414–418
Pillarisetti J, Patel P, Duthuluru S et al (2011) Cardiac catheterization in patients with end-stage liver disease: safety and outcomes. Catheter CardiovascInterv 77(1):45–48
Segal JB, Dzik WH (2005) Transfusion Medicine/Hemostasis Clinical Trials N. Paucity of studies to support that abnormal coagulation test results predict bleeding in the setting of invasive procedures: an evidence-based review. Transfusion. 45(9):1413–1425
Cerini F, Gonzalez JM, Torres F et al (2015) Impact of anticoagulation on upper-gastrointestinal bleeding in cirrhosis. A retrospective multicenter study. Hepatology 62(2):575–583
Lisman T, Caldwell SH, Burroughs AK et al (2010) Hemostasis and thrombosis in patients with liver disease: the ups and downs. J Hepatol 53(2):362–371
Stravitz RT, Lisman T, Luketic VA, Sterling RK, Puri P, Fuchs M, Ibrahim A et al (2012) Minimal effects of acute liver injury/acute liver failure on hemostasis as assessed by hromboelastography. J Hepatol 56(1):129–136
Youssef WI, Salazar F, Dasarathy S, Beddow T, Mullen KD (2003) Role of fresh frozen plasma infusion in correction of coagulopathy of chronic liver disease: a dual phase study. Am J Gastroenterol 98(6):1391–1394
Wiese S, Hove JD, Bendtsen F, Moller S (2014) Cirrhotic cardiomyopathy: pathogenesis and clinical relevance. Nat Rev Gastroenterol Hepatol 11:177–186
Ma Z, Lee SS (1996) Cirrhotic cardiomyopathy: getting to the heart of the matter. Hepatology 24:451–459
Moller S, Henriksen JH (2002) Cirrhotic cardiomyopathy: a pathophysiological review of circulatory dysfunction in liver disease. Heart 87:9–15
SuraniSR MY, Anjum H, Varon J (2016) Pulmonary complications of hepatic diseases. World J Gastroenterol 22(26):6008–6015. https://doi.org/10.3748/wjg.v22.i26.6008
Kozarek RA (2017) The future of ERCP. Endosc Int Open 5:E272–E274
Thalheimer U, Triantos CK, Samonakis DN, Patch D, Burroughs AK (2005) Infection, coagulation, and variceal bleeding in cirrhosis. Gut 54(4):556–563
Acknowledgements
The author acknowledges professors Imam Waked, Gamal Badra, Esam Elshimi, and Mai Magdi and all staff of the Endoscopy Unit, National Liver Institute, Menoufia University.
Funding
None.
Author information
Authors and Affiliations
Contributions
This is a single-author study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the National Liver Institute (IRB number: IRB00003413). All patients undergoing ERCP gave written informed consent for the study and for the procedure.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Attia, A. Safety, risk stratification, and cost of ERCP in patients with cirrhosis: a prospective controlled study. Egypt Liver Journal 14, 7 (2024). https://doi.org/10.1186/s43066-024-00311-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-024-00311-0