Abstract
Background
Gastrointestinal bleeding from cholecystoduodenal fistula is rare. It is usually managed surgically, although a conservative approach is reported in isolated cases.
Case presentation
A 71-year-old male patient was admitted to the emergency department (ED) presenting melena associated with severe anemia, requiring a blood transfusion. An urgent upper endoscopy showed the intestinal orifice of a cholecystoduodenal fistula. This finding was confirmed by radiological examination and laparoscopy. Cholecystectomy and simultaneous excision of the fistula were successfully performed. As a result, a diagnosis of Mirizzi syndrome type Va was also made.
Conclusion
A cholecystoduodenal fistula orifice leading to gastrointestinal bleeding is difficult to diagnose without an endoscopic examination of the upper digestive tract. Following this first diagnostic step, a comprehensive patient examination should be conducted, specifically if a history of gallbladder lithiasis has been reported.
Similar content being viewed by others
Background
A rare complication is upper gastrointestinal tract bleeding due to a cholecystoduodenal fistula [1]. It may be developed from a long-lasting chronic cholecystolithiasis, eventually leading to a Mirizzi syndrome, which results from forming adhesions between the gallbladder and its adjacent structures [2, 3]. Due to the scarce and unspecific symptoms, most cases are discovered only during surgery. As reported in literature, only 7.9% of patients receive a correct preoperative diagnosis [2]. Cholecystoduodenal fistula represents a subtype of bilioenteral fistulas. Its initial etiopathogenetic mechanism is triggered by an inflammatory process due to the impact of a stone in the Hartmann’s pouch of the gallbladder, leading, over time, to erosion, necrosis, formation of fistula, and adhesions [4]. Hereby, this case report presents a rare case of gastrointestinal bleeding due to a cholecystoduodenal fistula whose intestinal orifice was discovered during an urgent upper endoscopy and confirmed by radiological evaluation and an operation.
Case presentation
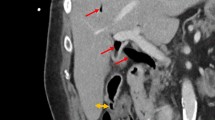
A 71-year-old male, on antiplatelet medication (clopidogrel 75 mg/day), presented to the emergency department (ED) for melena. On admission, his vital sign assessment recorded blood pressure of 105/70 mmHg, pulse rate of 87/min, and respiratory rate of 16/min. Physical examination of the abdomen highlighted only a weak positive Murphy sign with no peritoneal reaction to palpation. Laboratory tests revealed anemia (hemoglobin level was 7.2 g/dL) with normal platelet values (350 × 109/L), so the patient underwent a blood transfusion and urgent gastroscopy. This last revealed fresh and coagulated blood along the bulb and the second portion of the duodenum. After repeated washings, a polypoid-like lesion was observed of about 3 cm localized on the anterosuperior wall of the bulb. No apparent features of a heteroplastic lesion on narrow-band imaging (NBI) were noted (Fig. 1a). After having detached the apex of the formation with a biopsy forceps, a probable fistula orifice was found (Fig. 1b). The histological report of this lesion showed only an eroded mucosa without dysplasia or adenoma components. A focused assessment with sonography (FAST) demonstrated a stone of size 3 cm wedged in the infundibulum of the gallbladder. An abdominal computed tomography (CT) with intravenous (IV) contrast agent confirmed the ultrasound finding and revealed a close adherence between the gallbladder and the duodenum (Fig. 2a, yellow arrow). A subsequent abdominal magnetic resonance imaging (MRI) with intravenous (IV) contrast endorsed the results of the CT and pointed out the fistulous tract, which connected the gallbladder with the duodenum (Fig. 2b, yellow arrow). Furthermore, both these two radiological techniques, i.e., CT and MRI, excluded the concomitant presence of a biliary ileus. After obtaining the informed consent, the patient was referred for surgery. A laparoscopic cholecystectomy was performed with dissection of the adhesions, simultaneous excision of the fistula, and repair of the duodenal wall. Recovery was successful without any post-operative complications, and the patient was discharged six days later.
Discussion
Mirizzi syndrome is a rare condition found in only 0.1% of patients with gallbladder lithiasis and may be related to obstruction from a single large stone in Hartman’s pouch, as in the case of our patient [5]. Currently, this condition is classified into five types, of which type V is articulated into two subtypes (Va and Vb) based on the occurrence of gallstone ileus [6]. The latter degree of classification (type V) can also manifest as multiple fistulas, as reported in a 77-year-old man, in whom during an endoscopic retrograde cholangiopancreatography three fistulas were found, two cholecystogastric and one cholecystoduodenal [7]. Generally, it is recognized that both the formation of fistulous tracts and the appearance of a possible concomitant biliary ileus represent late complications of long-lasting gallbladder lithiasis. Beltran et al. [7] described 338 patients suffering from a Mirizzi condition and noted a cholecystoenteric fistula associated with gallstone ileus in only 12 cases. In patients with gallbladder stones, bilioenteric fistula incidence is 0.15–8% and presents in 0.15–5% of all biliary tract surgeries [1]. In type V of this syndrome, the most frequent fistulous tracts concerning location are cholecystoduodenal (77–90%), cholecystocolonic (8–26.5%), choledochoduodenal (5%), and cholecystogastric (2%) [6, 8]. A recent analysis of patients who experienced bleeding from a cholecystoduodenal fistula was performed [9]. A total of 15 patients (9 males and 6 females, with a mean age of 68.1 years) with this complication were analyzed [9]. Of these, 12 (80%) presented a gallbladder lithiasis, and only in 10 of them (83.3%) a gastroscopy was performed, highlighting the orifice of a fistula only in 3 cases (30%, 3/10). In this subgroup of 12 patients, surgery was successfully performed in 11 cases (91.6%), while only a 97-year-old patient died who was treated conservatively and was also the oldest [9]. Mirizzi syndrome and its complications are preferably treated surgically and, nowadays, in a less invasive way by the laparoscopic approach, as in our case [5, 10]. To underline the effectiveness of this procedure, in a retrospective study just released, 16 patients presenting with the Va subtype underwent successful laparoscopic surgical treatment [11].
Conclusion
This case demonstrates the necessity of endoscopy in the event of an upper gastrointestinal hemorrhage, since when a cholecystoduodenal fistula is discovered throughout the exam, as in our situation, it allows proceeding with further diagnostic investigations, leading to an eventual diagnosis of Mirizzi syndrome, which can be successfully treated with surgery. Emergency physicians should consider this rare complication while leading to a differential diagnosis of intestinal bleeding, especially in patients with a known history of gallbladder lithiasis, to set up a timely and appropriate treatment.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- CT:
-
Computed tomography
- ED:
-
Emergency department
- FAST:
-
Focused Assessment with Sonography for Trauma
- IV:
-
Intravenous
- MRI:
-
Magnetic resonance imaging
- NBI:
-
Narrow band imaging
References
Changku J, Shaohua S, Zhicheng Z, Shusen Z (2005) Upper gastric tract bleeding due to cholecystoduodenal fistula: a case report. Hepatogastroenterology 52(65):1372–1374. PMID: 16201077
Aguilar-Espinosa F, Maza-Sánchez R, Vargas-Solís F, Guerrero-Martínez GA, Medina-Reyes JL, Flores-Quiroz PI (2017) Cholecystoduodenal fistula, an infrequent complication of cholelithiasis: our experience in its surgical management. Rev Gastroenterol Mex. 82(4):287–295. https://doi.org/10.1016/j.rgmx.2016.10.010. Epub 2017 Apr 5. PMID: 28389051
Chen H, Siwo EA, Khu M, Tian Y (2018) Current trends in the management of Mirizzi syndrome: a review of literature. Medicine (Baltimore) 97(4):e9691. https://doi.org/10.1097/MD.0000000000009691. PMID:29369192;PMCID:PMC5794376
Chowbey PK, Bandyopadhyay SK, Sharma A et al (2006) Laparoscopic management of cholecystoenteric fistulas. J Laparoendos Adv Surg Tech A 16:467–472
Jones MW, Ferguson T (2023) Mirizzi Syndrome. StatPearls. StatPearls Publishing, Treasure Island
Beltran MA, Csendes A, Cruces KS (2008) The relationship of Mirizzi syndrome and cholecystoenteric fistula: validation of a modified classification. World J Surg 32(10):2237–2243. PMID: 18587614
Lalountas M, Smyrlis N, Mouratidis SV, Makedos P (2023) Mirizzi syndrome type V complicated with triple fistula: a case report. Surg Case Rep 9(1):110. https://doi.org/10.1186/s40792-023-01696-7. PMID:37335440;PMCID:PMC10279597
Faridi MS, Pandey A (2014) Mirizzi syndrome type II with cholecystoduodenal fistula: an infrequent combination. Malays J Med Sci 21(1):69–71
Park JM, Kang CD, Kim JH, Lee SH, Nam SJ, Park SC et al (2021) Cholecystoduodenal fistula presenting with upper gastrointestinal bleeding: a case report. World J Clin Cases 9(2):410–415
Severi C, Zippi M, Baccini F, Gentile G, Bezzi M, Fiocca F et al (2004) Amebic liver abscess, Mirizzi syndrome, and acute hepatic failure. Dig Dis Sci 49(2):304–307
Gómez D, Pedraza M, Cabrera LF, Mendoza Zuchini A, Arrieta GM, Aparicio BS, Pulido J (2022) Minimally invasive management of Mirizzi syndrome Va: case series and narrative review of the literature. Cir Esp (Engl Ed) 100(7):404–409. https://doi.org/10.1016/j.cireng.2022.04.024. Epub 2022 May 4 PMID: 35525486
Acknowledgements
The authors thank Dr. de Vito Saveria, Italian Medicines Agency, Rome, Italy, for the English revision of the manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MZ and AG—clinical care and diagnosis of the case. AT—collection of clinical information. WH and SF—contribution to the manuscript and manuscript correction. All authors have read and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The patient has given his written informed consent for publication, including publication of images, in which no identity is disclosed.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zippi, M., Toma, A., Hong, W. et al. A rare gastrointestinal bleeding due to a cholecystoduodenal fistula: a case report. Egypt Liver Journal 13, 55 (2023). https://doi.org/10.1186/s43066-023-00292-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-023-00292-6