Abstract
Background
Reactivation of herpesviruses such as Epstein–Barr virus (EBV) and cytomegalovirus (CMV) in COVID-19 patients reported in many studies in different countries during the pandemic. We aimed to measure prevalence of this coinfection in Egyptian COVID-19 patients with elevated liver enzymes and its relation to the severity and the outcome of COVID-19 infection in those patients.
Methods
A cross-sectional study was carried out on 110 COVID-19 patients with elevated liver enzymes regardless the severity of COVID-19 disease. All patients were subjected to medical history, clinical examination, laboratory investigations, high-resolution computed tomography chest (HRCT chest). Epstein–Barr virus (EBV) and Human cytomegalovirus (HCMV) were determined by VCA IgM and CMV IgM respectively by enzyme-linked immunosorbent assay (ELISA).
Results
Of the included 110 patients with COVID-19 illness, 5 (4.5%) were Epstein–Barr virus seropositive and 5 (4.5%) were human cytomegalovirus seropositive. Regarding the symptoms, the incidence of fever in the EBV and CMV seropositive group was apparently higher than that in the EBV and CMV seronegative group. In lab tests, the platelets and albumin of EBV and CMV seropositive group decreased more significantly than EBV and HCMV seronegative group, and serum ferritin, D-dimer, and C-reactive protein show higher values in seropositive group than in seronegative group but not statistically significant. Seropositive group had received higher doses of steroids than seronegative group. The median of hospital stay in seropositive group was (15 days) nearly double that of seronegative group with statistically significant difference between both groups.
Conclusion
Coinfection of EBV and CMV in COVID-19 Egyptian has no effect on the disease severity or the clinical outcome of the disease. But those patients had higher hospital stay duration.
Similar content being viewed by others
Introduction
The novel coronavirus first detected in Wuhan, China, in December 2019, named severe acute respiratory syndrome-coronavirus-2 (SARS-COV-2), causes coronavirus disease 2019 (COVID-19) [1]. COVID-19 is primarily transmitted through contact with droplets which contain viral particles [2].
A strong immune response is triggered in the lungs by the rapid replication of SARS-CoV-2. Cytokine storm syndrome gives rise to acute respiratory distress syndrome and respiratory failure, that is considered the main cause of death in COVID-19 patients [3, 4]. In some COVID-19 cases, multiple organ failure has also been reported [5, 6]. Increasing levels of ALT, AST, and bilirubin in SARS-CoV-2 infection, indicating injury to the hepatic tissue [3,4,5,6,7]. Some of these liver serum enzymes indicating hepatic damage, albumin level was significantly decreased, indicating the severity of the infection [8].
It was reported that there is suppression in COVID-19 patients’ immunity in the early stage of the disease particularly T cell-mediated immunity [9, 10]. Furthermore, drugs used in COVID‐19 treatment may also act a major role in altering immune responses by means of regulating intracellular signaling pathways, hence prompting the reactivation process of EBV. High dose of corticosteroids, which is used in COVID-19 treatment, has been stated as a risk factor for herpes virus reactivation, particularly EBV and CMV [11, 12].
Methods
Study design and participants
This was a cross-sectional study to measure prevalence of Epstein–Barr virus and cytomegalovirus in elevated liver enzymes patients infected with COVID-19. And to evaluate the relation between the severity and COVID-19 infection outcome in patients coinfected with CMV and EBV. One hundred and ten COVID-19 patients with elevated liver enzymes presented to Ain Shams University Hospitals and Damietta Fever Hospital. All adult patients (the mean age of patients is 55), with variety of spectrum of COVID‐19 illness, ranges from mild up to critical case, confirmed by qualitative real-time RT-PCR assay of nasopharyngeal swabs or by (SARS-COV2 antigen-RDT) and radiological criteria for COVID-19 infection [13], were included in the study. The spectrum of COVID-19 disease severity is classified, based on the severity of symptoms into four levels: mild, moderate, severe, and critical. Mild cases only have mild symptoms without radiographic features. Moderate cases present with fever, respiratory symptoms, and radiographic features. Severe cases develop one of three criteria: (a) dyspnea, RR more than 30 times/min, (b) oxygen saturation less than 93% in ambient air, and (c) PaO2/FiO2 less than 300 mmHg. Critical cases develop one of three criteria: (a) respiratory failure, (b) septic shock, and (c) multiple organ failure.
Patients with pre-existing liver disease, such as:viral hepatitis (A, B, C), decompensated liver disease, and hepatocellular carcinoma, were excluded from the study.
Study tools
Serum samples (2 ml) studied for EBV (viral capsid antigen) VCA IgM and CMV IgM determined by enzyme-linked immunosorbent assay (ELISA). All patients were tested for CBC, CRP, ALT, AST, D-dimer, and serum ferritin.
Statistical analysis
-
Data were tabulated and statistically analyzed using SPSS, version 20 (SPSS Inc., Chicago, IL).
-
Quantitative data were described as mean and standard deviation (minimum–maximum) and median and interquartile range.
-
Mann-Whitney U test was used for comparing quantitative variables between groups.
-
Qualitative data were expressed as frequencies (n) and percentage (%).
-
Fisher exact test was used to test the association between qualitative variables.
-
P value ≤ 0.05 was considered statistically significant.
Results
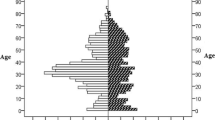
Baseline demographic data of patients included in this study, are listed in the Table 1. The mean age of patients was 55 ± 14.4 (range, 23–87 years) and 60.0% were less than or equal 60 years, with 50.9% were males. 94.5% of patients have no special habits, 75.5% were from Damietta, 57.6% (n = 49) were retired or not working.
CT chest findings among COVID-19 participants in the current study are listed in the Table 1. Shows that the most common finding was bilateral ground glass opacity (GGOs) (89.1%) while the other finding was unilateral subpleural GGOs patches as well as free CT chest.
There were 10 (9.1%) patients with either CMV or EBV seropositive tests group among the studied group of COVID-19 patients. Among those 10 patients, 5 were CMV and the other were EBV seropositive.
As regards comparison of sociodemographic data between COVID-19 patients with and without CMV or EBV coinfection, Table 2 shows that there were (60.0%) of seropositive group for EBV-VCA IgM and CMV IgM less than or equal 60 years old and it was not statistically significant difference. As regards gender, males (60%) were more than females with no statistically significant difference. As regards special habits of medical importance, 90.0% of patients have no special habits, and there was no statistically significant difference between smokers and non-smokers.
As regards comparison of presence of comorbidities between EBV and CMV seropositive and seronegative, Table 2 shows that patients in seropositive group for EBV and CMV who had no comorbidities (70%) were more than those who had comorbidities (30%) with no statistically significant difference, as regards those had comorbidities in seropositive group, the most common comorbidities were diabetes mellitus (50%) and hypertension (50%); also, these comorbidities were with higher percent in seropositive group more than in seronegative group, but without statistically significant difference. The only comorbidities that had statistically significant difference between seropositive group and seronegative group was kidney disease. Number of patients in seropositive group who had no kidney disease (80%) was more than those who had kidney disease (20%).
As regards comparison of symptoms between both groups, Table 3 shows that clinical symptoms such as fever, which its incidence in seropositive group is higher than in seronegative group with no statistically significant difference between both groups for any clinical symptom.
As regards laboratory parameters in the comparison between both groups, Table 4 shows that blood picture parameters lower values in seropositive group than in seronegative group without statistically significant difference except for platelets (P value = 0.021). Also, there were higher values for CRP, serum ferritin, D-dimer, ESR, ALT, AST, and PT in seropositive group than in seronegative group, but with no statistically significant difference between both groups. But there were lower serum albumin values in seropositive group than in seronegative group with statistically significant difference (P value = 0.039).
The median of hospital stay in seropositive group was (15 days) nearly double that of seronegative group with statistically significant difference between both groups.
As regards drugs intake in the comparison between both groups, Table 5 shows that steroids were taken in seropositive group in higher percentage than in seronegative group with no statistically significant difference. On the other hand, vitamins and antibiotics were taken in seronegative group than in seropositive group with statistically significant difference.
In EBV-VCA IgM and CMV IgM seropositive group, 4 (40.0%) are moderate COVID-19 cases, 4 (40.0%) severe cases, 2 (20.0%) critical cases on admission. Seven (70.0%) of them improved and discharged, 3 (30.0%) need ICU admission and died, as illustrated in Tables 6 and 7 respectively.
Discussion
EBV is latent in 90% of people approximately, and this is the highest rate among herpes viruses [14]. In individuals with severe COVID-19 illness, reactivation of viruses, such as herpes simplex, EBV, and CMV, occurs. The cause which has been suggested for this reactivation is the functional exhaustion of cytotoxic lymphocytes [15, 16]. COVID-19 can produce cellular immune dysfunction [16]; therefore, it can stimulate reactivation of latent viruses. Several studies have demonstrated a high incidence of EBV reactivation in COVID-19 patients [17,18,19].
Our study found that 10 (9%) COVID-19 patients were EBV-VCA IgM and CMV IgM seropositive, 5 (4.5%) COVID-19 patients were EBV-VCA IgM seropositive, and 5 (4.5%) COVID-19 patients were CMV IgM seropositive.
While the results in the study of Xie et al. (2021) which found that 17 (13.3%) were diagnosed with EBV infection in 128 critically ill COVID-19 patients [20]. Probably, the difference in the results because they established their study on critically ill COVID-19 patients only while in this study, the sample include all spectrum of illness from mild to critical COVID-19 cases.
Also, Im et al. (2022) reported that EBV viremia was found in 16.7% of 269 COVID-19 patients [19]. The difference in the results may be because their sample was larger than our sample, and their results depend on detection of EBV viremia, using the Real-Q EBV Quantification Kit (BioSewoom, Inc., Seoul, Republic of Korea) with 72 copies/mL cut-off value for EBV viremia while we use EBV-VCA IgM in the detection of EBV infection.
In addition, Gold et al. (2021) found that EBV reactivation was in 66.7% (20/30) of long-term long COVID patients versus 10% (2/20) of long-term control patients, based on positive titers for EBV VCA IgM or EBV EA-D IgG [21]. The difference in results may be because they used EBV VCA IgM or EBV EA-D IgG to detect EBV infection reactivation, and they found 18 of the long-term long COVID-19 patients were positive for EBV EA-D IgG, 1 of which was also EBV VCA IgM-positive. Two additional long-term long COVID-19 patients were positive for EBV VCA IgM but not EBV EA-D IgG, and the two patients positive for EBV reactivation in the long-term control group were positive for EBV EA-D IgG only, they caught more cases of EBV reactivation by EBV EA-D IgG, while we only used EBV VCA IgM in the detection of EBV infection.
On the other hand, Chen et al.’s (2021) study disagreed with our results as they found negative CMV IgM antibody in COVID-19 patients in their study [22], probably because their study included relatively small number (67 COVID-19 patients) than our sample (110 COVID-19 patients).
Also, Paolucci et al.’s (2021) study is in disagreement with our results about CMV IgM as they reported that CMV reactivation was never observed, they do CMV PCR [18] but in this study, it was not done. This difference in these results could be attributed to the variability in COVID-19 infection nature and the sociodemographic difference of patients.
In the current study, regarding the symptoms, the incidence of fever in the EBV and HCMV seropositive group was apparently higher than that in the EBV and HCMV seronegative group. Also, no statistically significant difference for other symptoms between both groups. This was in agreement with Naendrup et al.’s (2021) study which reported persisting fever in COVID-19 patients with EBV and CMV reactivation [11]. Also, these findings agreed with the findings in Chen et al. (2021), beside that they found statistically significant difference for fever between both groups [22].
As regards laboratory parameters in the current study, the platelets, albumin, serum ferritin, D-dimer, and C-reactive protein show higher values in seropositive group than in seronegative group but not statistically significant. Thrombocytopenia conditions and immune thrombocytopenia reported with EBV and CMV infection in many studies such as Wu et al. (2013) and Zhang et al. (2021) which agree with our findings in the current study [23, 24].
This is in disagreement with Chen et al.’s (2021) study which reported that blood routine examination and blood biochemistry results reveals no significant differences between EBV/SARS-CoV-2 coinfection and SARS-CoV-2 infection alone patients [22]. Also, this was in disagreement with Naendrup et al.’s (2021) study which reported that there were no correlations between EBV and CMV reactivations and neutrophil-to-lymphocyte ratio [11].
This finding is in agreement with Xie et al.’s (2021) study which reported that patients with EBV reactivation had lower albumin and higher incidence of hypoproteinaemia in EBV group than in non-EBV group [20].
These findings were not agreed with those in Chen et al.’s (2021) study which reported that no significant difference in liver function tests between EBV/SARS-CoV-2 coinfection patients and SARS-CoV-2 infection alone patients except for aspartate aminotransferase (AST) which had significantly higher results in EBV/SARS-CoV-2 coinfection patients than that in SARS-CoV-2 infection alone patients [22].
On the other hand, Naendrup et al.’s (2021) study reported that there was no correlation between EBV and CMV reactivations and the transaminases as well as bilirubin were detected [11].
These higher values of C-reactive protein also shown in EBV/SARS-CoV-2 coinfection patients in Chen et al.’s (2021) study and were higher than that of SARS-CoV-2 infection alone patients [22]. Higher D-dimer and CRP in EBV seropositive COVID-19 patients than in EBV seronegative patients also reported in Xie et al. (2021) [20].
On the other hand, this was in disagreement with Naendrup et al.’s (2021) study which reported that there was no correlation between EBV and CMV reactivations and C-reactive protein, and ferritin levels [11].
In the current study, seropositive group had received higher doses of steroids than seronegative group. This was in agreement with Naendrup et al.’s (2021) study which stated that the use of high‐dose corticosteroids as a risk factor for herpes virus reactivation [11].
Also, these findings agreed with Chen et al.’s (2021) study which reported that the EBV/SARS-CoV-2 coinfection individuals were more likely to be received corticosteroid therapy by doctors than the SARS-CoV-2 infection alone patients [22].
In addition, Im et al.’s (2022) study reported that steroid administration is often prolonged in patients with severe COVID-19. In addition, host immunity may be compromised because of critical illness. EBV viremia can persist at high levels in these cases [19].
Moreover, in the current study, as regards period of admission in the comparison between EBV and CMV seropositive and seronegative groups, the median of hospital stay for the seropositive group was (15.0) double that for the seronegative group (7.0) with statistically significant difference (P value = 0.019). These data were in agreement with Chen et al. (2021) but without statistically significant difference. Also, agree with Simonnet et al.’s (2021) study which that EBV reactivation in critically ill COVID-19 patients was associated with a longer duration of intensive care unit stay [25].
The current study did not show increased disease severity in individuals with coinfection of EBV, CMV, and SARS‐CoV‐2 and the results demonstrated no differences in disease outcome, may be due to the small sample. These results are in agreement with Blumenthal et al. (2021), who found that individuals with coinfection of EBV and SARS‐CoV‐2 did not show increasing in disease severity and the results showed no differences in terms of viral load and disease outcome [26]. Larger scale of studies including COVID-19 patients with either normal or elevated liver enzymes values could give more data about the effect of CMV and EBV coinfection on the incidence of elevation of liver enzymes in such patients.
Conclusion
Coinfection of EBV and CMV has been found in Egyptian COVID-19 patients. COVID-19 disease severity and clinical outcome were not affected by EBV and CMV coinfection, but those patients had higher hospital stay duration.
Study limitations
The limited number of studied patients and the dependence on serological tests in CMV and EBV diagnosis rather confirmation by Rt-PCR.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- EBV:
-
Epstein–barr virus
- CMV:
-
Cytomegalovirus
- HRCT:
-
High-resolution computed tomography
- HCMV:
-
Human cytomegalovirus
- VCA:
-
Viral capsid antigen
- ELISA:
-
Enzyme-linked immunosorbent assay
- COVID-19:
-
Coronavirus disease 2019
- SARS‐CoV‐2:
-
Severe acute respiratory syndrome -coronavirus-2
- DM:
-
Diabetes mellitus
- HTN:
-
Hypertension
- IHD:
-
Ischemic heart disease
- BA:
-
Bronchial asthma
- COPD:
-
Chronic obstructive pulmonary disease
- HF:
-
Heart failure
- CBC:
-
Complete blood count
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- ALP:
-
Alkaline phosphatase
- GGT:
-
Gamma glutamyl transferase
- PT:
-
Prothrombin time
- INR:
-
The international normalized ratio
- RT-PCR:
-
Real-time reverse transcription polymerase chain reaction
- EBV EA:
-
Epstein–Barr virus early antigen
References
Lu H, Stratton CW, Tang YW (2020) Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol 92(4):401
Dietz L, Horve PF, Coil DA, Fretz M et al (2020) 2019 novel coronavirus (COVID-19) pandemic: built environment considerations to reduce transmission. Msystems 5(2):e00245-e320
Huang C, Wang Y, Li X, Ren L et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan China. Lancet 395(10223):497–506
Mehta NS, Mytton OT, Mullins EW, Fowler TA et al (2020) SARS-CoV-2 (COVID-19): what do we know about children? A systematic review. Clin Infect Dis 71(9):2469–2479
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323(13):1239–1242
Chen N, Zhou M, Dong X, Qu J et al (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223):507–513
Guan WJ, Ni ZY, Hu Y, Liang WH et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382(18):1708–1720
Chen L, Liu HG, Liu W, Liu J et al (2020) Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia. Zhonghua jie he he hu xi za zhiZhonghua jiehe he huxi zazhi Chin J Tuberc Respir Dis 43:E005–E005
Tian W, Zhang N, Jin R, Feng Y et al (2020) Immune suppression in the early stage of COVID-19 disease. Nat Commun 11(1):1–8
Bo XU, Fan CY, Wang AL, Zou YL et al (2020) Suppressed T cell-mediated immunity in patients with COVID-19: a clinical retrospective study in Wuhan China. J Infect 81(1):e51–e60
Naendrup JH, Garcia Borrega J, Eichenauer DA, Shimabukuro-Vornhagen A et al (2022) Reactivation of EBV and CMV in Severe COVID-19—Epiphenomena or Trigger of Hyperinflammation in Need of Treatment? A Large Case Series of Critically ill Patients. J Intensive Care Med 37(9):1152–58. https://doi.org/10.1177/08850666211053990
Shafiee A, Aghajanian S, Atharn MMT, Gargari OK (2022) Epstein–Barr virus and COVID-19. J Med Virol 94(9):4040–42. https://doi.org/10.1002/jmv.27823
Bao C, Liu X, Zhang H et al (2020) Coronavirus Disease 2019 (COVID-19) CT finding: a systemic review and meta-analysis. J Am Coll Radiol 17:701–709
Kang CI, Choi CM, Park JT, Park TS (2007) Seroprevalence of Epstein-Barr virus infection in young men of South Korea. Infect Chemother 39:93–94
Coşkun O, Yazici E, Şahiner F et al (2017) Cytomegalovirus and Epstein-Barr virus reactivation in the intensive care unit. Med Klin Intensivmed Notfmed 112:239–45
Textoris J, Mallet F (2017) Immunosuppression and herpes viral reactivation in intensive care unit patients: one size does not fit all. Crit Care 21:230
Lehner GF, Klein SJ, Zoller H, Peer A et al (2020) Correlation of interleukin-6 with Epstein-Barr virus levels in COVID-19. Crit Care 24:1–3
Paolucci S, Cassaniti I, Novazzi F et al (2021) EBV DNA increase in COVID-19 patients with impaired lymphocyte subpopulation count. Int J Infect Dis 104:315–319
Im JH, Nahm CH, Je YS, Lee JS et al (2022) The effect of Epstein-Barr virus viremia on the progression to severe COVID-19. Medicine 101(18):e29027
Xie Y, Cao S, Dong H, Lv H et al (2021) Clinical characteristics and outcomes of critically ill patients with acute COVID-19 with Epstein-Barr virus reactivation. BMC Infect Dis 21(1):1–8
Gold JE, Okyay RA, Licht WE, Hurley DJ (2021) Investigation of long COVID prevalence and its relationship to Epstein-Barr virus reactivation. Pathogens 10(6):763
Chen T, Song J, Liu H, Zheng H et al (2021) Positive Epstein-Barr virus detection in coronavirus disease 2019 (COVID-19) patients. Sci Rep 11(1):1–7
Wu Z, Zhou J, Wei X, Wang X et al (2013) The role of Epstein-Barr virus (EBV) and cytomegalovirus (CMV) in immune thrombocytopenia. Hematology 18(5):295–299
Zhang C, Kelly AM (2021) Severe thrombocytopenia in a case of Epstein-Barr virus-induced infectious mononucleosis. Cureus 13(9):17706
Simonnet A, Engelmann I, Moreau AS, Garcia B et al (2021) High incidence of Epstein-Barr virus, cytomegalovirus, and human-herpes virus-6 reactivations in critically ill patients with COVID-19. Infect Dis Now 51(3):296–299
Blumenthal MJ, Lambarey H, Chetram A, Riou C, et al (2021) Kaposi’s sarcoma-associated herpesvirus, but not Epstein-Barr virus, co-infection associates with coronavirus disease 2019, severity and outcome in South African Patients. Front Microbiol 2022;12:795555. https://doi.org/10.3389/fmicb.2021.795555. eCollection 2021
Acknowledgements
Not applicable.
Funding
The authors received no funding for this study.
Author information
Authors and Affiliations
Contributions
EMFB, AFH, and NGE were responsible for the modification and giving final approval of the manuscript. MMK was contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethical Committee of Ain Shams University Hospitals (31/8/2021), no. (FWA 000017585).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barakat, E.F., Sherief, A.F., Elsheikh, N.G. et al. Epstein–Barr virus and cytomegalovirus coinfection in Egyptian COVID-19 patients. Egypt Liver Journal 13, 27 (2023). https://doi.org/10.1186/s43066-023-00262-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-023-00262-y