Abstract
Background
Laparoscopic cholecystectomy has become a gold standard treatment for symptomatic cholelithiasis and other related diseases done in most centers worldwide. It is associated with an increase in frequency of iatrogenic biliary injury with an incidence of 0.3–0.7%, resulting in a significant impact on quality of life, overall survival, and frequently medico-legal obligations. Early recognition of bile duct injury (BDI) is of supreme importance towards early treatment and good outcome. With an experienced hepatobiliary surgeon, hepaticojejunostomy by left hepatic duct approach is often challenging and considered impossible due to scarring and fibrosis but has a noble outcome for proximal common hepatic duct injury.
Cases presentation
We described two cases from northern Tanzania who had iatrogenic proximal bile duct injury following laparoscopic cholecystectomy. Hepaticojejunostomy by left hepatic duct was the approach used after difficult dissection at porta hepatis and partly the liver tissue to attain a significant length of the left hepatic duct for anastomosis done at least 3 months post-bile duct injury. No postoperative complication was observed, which includes biliary fistula, restenosis, peritonitis, and cholangitis. To date, no evidence of biliary stenosis or other biliary complication happened during follow-up for 1 year.
Conclusion
Early recognition of BDI is of supreme importance towards early treatment and good outcome. With an experienced hepatobiliary surgeon, hepaticojejunostomy by left hepatic duct approach has an honorable outcome for proximal bile duct injury.
Similar content being viewed by others
Background
LC has become a gold standard treatment for symptomatic cholelithiasis in most centers. Bile duct injury (BDI) is the most iatrogenic complication frequently encountered with an incidence of 0.3–0.7%, resulting in a significant impact on quality of life, overall survival, and frequent medico-legal obligations [1]. Up to about 71–97% of all cases of BDI, difficulty in identifying the biliary anatomy has been reported to be the primary cause of biliary duct injury; hence, a clear definition of biliary anatomy could prevent these injuries at large.
In 1995, Strasberg introduced the CVS technique which is considered to be the gold standard to perform a safe cholecystectomy with the identification of biliary structures during dissection [2]. Three criteria are required to accomplish the CVS; first, the hepatocystic triangle must be cleared of adipose and fibrotic tissue; second, the lower third of the gallbladder must be separated from the liver bed to expose the cystic plate; and third, only two structures should be seen entering the gallbladder. CVS was conceived not as a way to do LC but as a way to avoid biliary injury.
The optimal treatment of BDI is influenced by the timing of recognition of the injury, the extent of BDI, the patient’s clinical condition, and the availability of experienced hepatobiliary surgeons. Early recognition of BDI is of supreme importance towards early treatment and good outcome.
Classification of bile duct injury
Bismuth and Strasberg classifications are mostly used ways of classifying biliary injury according to the level of biliary injury; it includes biliary injuries seen more commonly in the laparoscopic era, in particular biliary leaks [3]. These classifications have been summarized in Table 1.
Risk factors
Generally, any surgical procedure involving the gallbladder, common bile duct (CBD), or even surrounding organs can lead to a bile duct injury or stricture. There are various risk factors which can be attributed to a higher risk of BDI which can be divided into anatomical factors, patient-related factors, human factors, factors related to gallbladder disease, the surgical technique, and timing of surgery.
Anatomical factors include misinterpretation of biliary anatomy during LC and the anatomical variations of the biliary tract such as short cystic duct, the presence of hepatocystic duct, cystic duct running parallel to the CBD, accessory cystic duct, and the presence of aberrant bile ducts increase the risk of biliary injuries. The aberrant RHD anomaly is the common cause of biliary injury. The direction of traction of the gallbladder has been known to contribute to its misidentification and injury [4]. Among the patient-related factors are severe obesity, previous surgery on the biliary tract or pancreas, and underlying liver disease. Acute cholecystitis causes a series of modifications of the local anatomy (adhesions, thickening of the tissues, inflammation, bleeding) that are associated with an increased risk of iatrogenic lesion [5]. The human factors also play a vital role in the pathophysiology of the iatrogenic bile lesion: the excessive safety of the surgeon, the rush to finish the intervention, being a teaching hospital, the fatigue and personal concerns of the surgeon, the performance anxiety, the superficiality of the surgical act, and the lack of humility in converting to open surgery in doubtful cases may determine a relevant damage to the biliary tree [4]. Others include the type of procedure; open cholecystectomy is associated with less biliary injuries as compared with LC as seen in various studies and timing of surgery whereas emergency cholecystectomy has a three times more likelihood of causing biliary injury than elective surgery [6].
Timing for recognition, clinical presentation, and evaluation of BDI
A delay in diagnosis is crucial for the postoperative outcome. Only about less than 30% of BDI are recognized intraoperative especially by a few surgeons who perform on-table cholangiography due to convenience or commonly due to lack of the service [7]. BDI are well managed by experienced hepatobiliary surgeons in high-volume centers; otherwise, it is recommended that once diagnosed intraoperatively, intra-abdominal drain should be placed and patient referred to high hepatobiliary center [8].
Diagnosis often occurs in the immediate postoperative period (within 6 weeks post-intervention) or in some cases, later (over 6 weeks). The presence of persistent or abdominal pain in the right hypochondrium, the leakage of bile from drainage (if placed during surgery), features of biliary peritonitis, and the appearance of fever and jaundice with increased liver function tests are all elements supporting a diagnosis of any iatrogenic BDI.
Various radiological investigation can be done to evaluate the scope of BDI so as to plan for the therapeutic intervention. Abdominal ultrasound as the first tool can be done to show any collection, biliary dilatation, associated vascular, and surrounding organ injury [9]. The abdominal CT scan has added advantage of high accuracy and objective way of defining the focal intra- or peri-hepatic fluid collections, ascites, biliary obstruction, secondary biliary cirrhosis, and associated vascular and nearby organ injury. Contrasted magnetic resonance cholangiopancreatography (MRCP) is the “gold standard” for the complete morphological evaluation of the biliary tree as it gives detailed information about the integrity of the biliary tract [10]. The use of contrast agent during MRCP permits detection of bile leakage by direct visualization of contrast material into fluid collections in addition to indicating the anatomical site of the leakage and the type of BDI.
Generally, if fluid collection is found in one of the imaging studies, an abdominal drain should be placed right away under radiological guidance in order to improve patient’s clinical condition (peritonitis, sepsis, tissue repairing) while optimizing the patient for definitive surgery about 2–3 months post-injury [8]. Due to increased morbidity and mortality associated with explorative laparotomy, laparoscopy can be done postoperatively period for diagnostic or additional intervention to identify other biliary injuries, drainage of any intra-abdominal collection, and exclusion of injury to other surrounding organs, which can lead to the decision between conservative management and early or late definitive surgical repair [11].
The ERCP examination has an important diagnostic and therapeutic role in cases where a conservative therapeutic approach is preferred based on the type and extent of the biliary lesion cystic duct leaks.
Therapeutic management
Management of BDI based on Bismuth-Strasberg classification which is a helpful tool to decide the best intervention for each case according to etiological mechanism of the injury [12].
The timing of the operation is an extremely important factor in the repair of the lesion because of challenges during surgery which are contributed by the size and caliber of the bile duct and from local inflammatory and sclerotic; hence, early identification of the lesion plays a significant part. In case of partial or complete transection of the CBD, it is possible to perform a tension-free direct end-to-end suture if the distal choledochus and preferable to protect the suture by inserting a Kehr T-tube or internal Y-drainage [13]. When primary repair is not possible or in cases of severe biliary strictures, a biliodigestive anastomosis is recommended, a Roux-en-Y hepaticojejunostomy in most cases, as demonstrated. If a hepaticojejunostomy cannot be performed due to the presence of dense adhesions with infected and friable tissues, a combination of endoscopic biliary stenting and pedicle omental patch repair of the bile duct to control bile leak and sepsis as a bridging procedure to definitive hepaticojejunostomy [14].
In case of strictures involving the bifurcation or left or RHD, unilateral or bilateral hepaticojejunostomies may be necessary [15]. Endoscopic dilatation followed by placement of stents is an accepted alternative, with both techniques resulting in similar clinical success: surgery vs endoscopy. They have a similar stricture recurrence rate of 17% [16] and excellent or good long-term outcomes; 77.3% (17 of 22) of patients were treated surgically and 80% (16 of 20) patients treated endoscopically [17].
ERCP is the first-line management option for most patients with biliary stricture as it is safe, effective, repeatable, and less invasive than other treatment options, such as percutaneous or surgical modalities [18] but associated with adverse events in 3.4–6.5% of procedures, including pancreatitis (2.2%), perforation (0.8%), and major bleeding (0.4%) [19].
Liver resection is very rarely indicated in cases of extensive hepatic necrosis. In a small subset of patients with iatrogenic BDIs, failure of surgical or non-surgical management might lead to acute or chronic liver failure necessitating liver transplantation [20].
Preventive measures for iatrogenic BDI
SAGES has created a six-step Safe Cholecystectomy [21]. The principles include the following:
-
Achieving the critical view of safety
-
Recognizing aberrant anatomy
-
Performing an intra-operative time-out before clipping or cutting ductal structures
-
Liberal use of intraoperative cholangiogram
-
Devising bail-out options
-
Asking for help in difficult cases
Case presentation
Case A
A 40-year female from northern Tanzania was presented to our facility with 2-month history of abdominal pain and had a percutaneous abdominal drain catheter for 1 month following relaparotomy.
She had a history of LC for symptomatic cholelithiasis 1 month prior. On the second day post-LC, she developed features of peritonitis that required exploration in OR. At laparotomy, she was found to have serosanguinous fluid of about 1500 cc, and no obvious bile leak was noted. Abdominal lavage was done and drain tube was put in place. Four days post laparotomy, the abdominal drain had bilious effluent, and she underwent second laparotomy which was found to have 3 areas of bile leak first at RHD just proximal to the confluence, second further proximal to the first, and third at the proximal CHD just near the confluence. Primary repair was attempted unsuccessfully as it was technically difficult to access the almost intrahepatic bile ducts. 24Fr Foley catheter was placed at the point of leak, then exteriorized out for drainage. She fairly recovered with about 700 cc bile output per 24 h until the referral to our center.
At MNH, she was reviewed by IR team, abdominal MRCP was performed, it revealing diffuse intrahepatic bile duct dilatation, dilated CHD with a stricture at 1.39 cm distal to the confluence, corresponding to Bismuth 2 (Fig. 1). PTBD was performed. She had an uneventful recover, and the abdominal drain (Foley catheter) was removed at 14th day post-PTBD. She stayed with PTBD tube for about 2 months with bile output of 1000 cc per day (on average) before being referred to our department.
At 3 months post-BDI, the patient underwent explorative laparotomy and she was found to have extensive adhesions at the hilar plate, with clinically stenotic confluence (Bismuth type 3). Technically difficult dissection was performed to mobilize the LHD to about 2-cm length proximally from the confluence and end-to-side Roux-en-Y tension-free left hepaticojejunostomy was performed using 3–0 PDS sutures. PTBD tube was left in situ. Total operative time was about 6 h. Intraoperative blood loss was estimated to be 300 cc; there was no blood transfusion intraoperatively. She had an uneventful recovery, and on day 21 PTBD, tube was removed. It is now 1 year post-hepaticojejunostomy, she is attending our OPD clinic for follow-up, and there is no evidence of biliary stenosis or biliary complication happened.
Case B
A 46-year female from Northern Tanzania was referred to our facility with 2-month history of yellowish coloration of eyes, generalized body itching, and passage of pale stool which developed 7 weeks post-LC for cholelithiasis.
At MNH in the IR unit, MRCP was done and revealed a massive dilated bilateral intrahepatic bile duct with a stricture at the confluence corresponding to Bismuth type 3 (Fig. 2). PTBD was performed, and the patient had significant improvement for 2 months, bile duct drain internalization was attempted twice, but it was unsuccessful. Patients had recurrent cholangitis and peristomal bile leak.
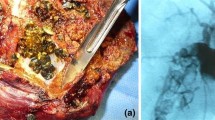
At 6 months post-LC, the patient was optimized for explorative laparotomy. Intraoperatively, she was found to have extensive adhesions, fibrotic CHD, dilated confluence, and proximal bile ducts (Bismuth 3). Dissection at the hilar plate, mobilization of the confluence, and more the LHD to about 1.5-cm length proximally from the confluence with dissection partly of liver tissue (Fig. 3).
Side to side Roux-en-Y left hepaticojejunostomy tension-free anastomosis was performed using interrupted 3–0 PDS sutures. Total operative time was about 5 h. Blood loss during the operation was about 350 cc and one unit of whole blood was transfused intraoperatively. No postoperative complication was observed and she was discharged on the 13th postoperative day. No evidence of biliary stenosis or other biliary complications happened during 1 year of follow-up.
Preoperative preparation
Prior to the procedure, complete blood count, liver function tests, renal function test, and electrolytes and cardiopulmonary functional assessment were done, and all were found to be normal. Patients were reviewed by anesthesiologist and were cleared for general anesthesia with ASA II, ECOG 1. Informed consent was obtained and the patients were ready for the operation. Patients had overnight fasting and antibiotics were administered within 40 min prior to the incision.
Discussion
In the past 10 years, LC has been introduced in various centers in Tanzania, including MNH as a customary treatment for symptomatic cholelithiasis and other related gall bladder disease. There is no published data which shows complications related to this procedure, but observation shows there is a rise in the pattern and frequency of biliary injury related to the procedure as compared to the previous open cholecystectomy reflecting various centers worldwide [1]. At this level where most surgeons are at early levels of learning curve, violation of SAGES principles for prevention of iatrogenic BDI particularly failure in identification and interpretation of structure at surgery, i.e., attaining CVS, has been a mutual occurrence among surgeons [22].
In previous studies, intraoperative cholangiography has been recommended in the course of LC especially in the setting of inexperienced surgeons. It is valued in detecting bile duct stones and delineating the anatomy of the biliary ducts, facilitating dissection, avoiding injuries to the biliary tract, and identifying other abnormalities, such as fistulas, cysts, and tumors of the biliary system [23]. This test is not in place in almost all centers in Tanzania; otherwise, it is the surgeon preference to do it or not. In case A, at first laparotomy biliary injury was missed which is a common phenomenon, same as at LC [7]. On-table cholangiography could help early detection of biliary injury. We feel that cholangiography should be endeavored on all patients undergoing LC especially at the hand of inexperienced surgeon [24].
In case B who had PTBD, bile duct drain internalization was attempted twice but it failed due to stenotic stricture at the confluence. At the time, surgery was the main option for the bile draining considering her age, performance status and associated complication rates, discomfort due to longstanding indwelling catheters, and high-stricture recurrence rates [25]. Only it has been recommended this surgery should be managed by experienced hepatobiliary surgeon in high volume centers; otherwise, once diagnosed, intra-abdominal drain or percutaneous drain should be placed as a temporary measure and patient referred to a high center with hepatobiliary surgeon [8].
Early postoperative biliary injury recognition (typically within 24 to 48 h) in a stable patient without signs of sepsis may be repaired immediately. Primary biliary repair attempt was done in case A, at day two unsuccessful. In general, intraoperative recognition should typically prompt immediate surgical repair as this confers the best outcomes; however, less than 40% of bile duct injuries are recognized at the index operation. Stewart and Law reviewed bile duct repairs done by specialists and general surgeons and found that only 17% of patients repaired by the general surgeon had a favorable outcome [26]. Bile duct injuries should not be underestimated, if the surgeon is inexperienced, an intraabdominal drain should be placed, and the patient should be immediately transferred to a hepatobiliary specialist as observed after the second attempt, case A.
In our cases, both A and B were operated on at least 3 months post BDI, with the successful results similar to other studies which recommend that late postoperative recognition should generally be managed by immediate control of the sepsis with delayed reconstruction in about 12 weeks [27]. Preoperatively further evaluation should be done to classify the extent of the injury and set planning. In our setting, we were able to do MRCP and CT scan which are available towards the evaluation of the biliary tree [28]. ERCP and PTC are procedures capable of both diagnosis and treatments for biliary injuries that are not put into practice.
The choice of anastomosis depends on the extent and location of biliary stricture. In the two cases, A and B, we did Roux-en-Y hepaticojejunostomy successfully. It is a useful form of biliary reconstruction for bypassing or reconstructing the biliary drainage after radical resection. This reconstruction is safe and effective at managing BDI to include early transections and delayed strictures. So far the method has been used successfully in most cases reported preferable end-to-side anastomosis [29]. In end-to-side Roux-en-Y hepaticojejunostomy, a Roux loop made of healthy, tension-free jejunum distal to the ligament of Treitz passed to the hilum of the liver and anastomosed in an end-to-side fashion to the proximal bile duct. The procedure is safe and durable, with a rate of success of 80–99% in the hands of experienced surgeons [30]. End-to-end anastomosis may be performed if the stricture is short and extrahepatic, and the ends can be opposed without tension. This approach is seldom used, given the inevitable loss of ductal length associated with fibrosis, as well as lack of expertise.
The purpose of bile duct reconstruction is the restoration of long-term functional biliary–enteric continuity. We achieved continuity through anastomosis to the LHD. Normally the RHD, about 1 cm, is in an extrahepatic position while the LHD has a much longer extrahepatic course than the right bile duct about 2 to 3 cm in length [31]. This is a key anatomic feature, which makes this length of the duct the prime site for high biliary–enteric anastomosis. It is much easier to expose a long length of LHD and hence tension-free anastomosis. It is often difficult and often considered impossible because it involves dissection into an area with scarring and fibrosis at porta hepatis, confluence and partly the liver tissue to attain a significant length of the duct for anastomosis. It is mainly achieved in the hand of experienced hepatobiliary surgeon in high center.
Conclusion
LC has become a gold standard treatment for symptomatic cholelithiasis and other related diseases done in most centers. BDI has become the most iatrogenic complication frequently encountered during LC, resulting in a significant impact on quality of life, overall survival, and frequently medico-legal obligations mainly due to violation of CVS technique. Early recognition of BDI is of supreme importance towards early treatment and good outcome. With an experienced hepatobiliary surgeon, hepaticojejunostomy by LHD approach has a noble outcome for proximal BDI.
Availability of data and materials
Not applicable.
Abbreviations
- LC:
-
Laparoscopic cholecystectomy
- MNH:
-
Muhimbili National Hospital
- BDI:
-
Bile duct injury
- CVS:
-
Critical view of safety
- CBD:
-
Common bile duct
- CHD:
-
Common hepatic duct
- CT:
-
Computerized tomography
- RHD:
-
Right hepatic duct
- LHD:
-
Left hepatic duct
- SAGES:
-
Society of American Gastrointestinal and Endoscopic Surgeons
- MRCP:
-
Magnetic resonance cholangiopancreatography
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- PTBD:
-
Percutaneous transhepatic biliary drainage
- IR:
-
Intervention Radiology
- ASA:
-
American Society of Anesthesiologists
References
Pesce A, Palmucci S, La Greca G, Puleo S (2019) Iatrogenic bile duct injury: impact and management challenges. Clin Exp Gastroenterol. 12:121–128
Strasberg SM, Brunt LM (2010) Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg. 211(1):132–138. Bing [Internet]. [cited 2021 Dec 5]
Bismuth H, Majno PE (2001) Biliary strictures: classification based on the principles of surgical treatment. World J Surg 25(10):1241–1244
Hugh TB (2002) New strategies to prevent laparoscopic bile duct injury - surgeons can learn from pilots. Surgery 132(5):826–835
Georgiades CP, Mavromatis TN, Kourlaba GC, Kapiris SA, Bairamides EG, Spyrou AM et al (2008) Is inflammation a significant predictor of bile duct injury during laparoscopic cholecystectomy? Surg Endosc Other Interv Tech 22(9):1959–1964
Russell JC, Walsh SJ, Mattie AS, Lynch JT (1996) Bile duct injuries, 1989-1993. A statewide experience. Connecticut Laparoscopic Cholecystectomy Registry. Arch Surg 131(4):382–388. Bing [Internet]. [cited 2021 Dec 5]
Seeras K, Kalani AD. (2018) Bile duct repair. Treasure Island, FL: StatPearls Publishing LLC; Available at: https://www.ncbi.nlm.nih.gov/books/NBK525989/. - Bing [Internet]. [cited 2021 Dec 5]
Stewart L (2014) Iatrogenic biliary injuries: identification, classification, and management. Surg Clin North Am 94(2):297–310. Bing [Internet]. [cited 2021 Dec 5]
Latteri S, Malaguarnera G, Mannino M, Pesce A, Currò G, Tamburrini S et al (2017) Ultrasound as point of care in management of polytrauma and its complication. J Ultrasound 20(2):171–177
Palmucci S, Mauro LA, La Scola S et al (2010) Magnetic resonance cholangiopancreatography and contrast-enhanced magnetic resonance cholangiopancreatography versus endoscopic ultrasonography in the diagnosis of extrahepatic biliary pathology. Radiol Med. 115(5):732–746. Bing [Internet]. [cited 2021 Dec 5]
Gupta V, Jayaraman S (2017) Role for laparoscopy in the management of bile duct injuries. Can J Surg 60(5):300–304
Nasa Mukesh et al (2020) Bile Duct Injury—Classification and Prevention. J Digest Endosc. 11:182–186
Jabłonska B (2014) End-to-end ductal anastomosis in biliary reconstruction: Indications and limitations. Can J Surg 57(4):271–277
Ng JJ, Kow AWC (2017) Pedicled omental patch as a bridging procedure for iatrogenic bile duct injury. World J Gastroenterol 23(36):6741–6746. Bing [Internet]. [cited 2021 Dec 5]
Giulianotti PC, Quadri P, Durgam S, Bianco FM (2018) Reconstruction/repair of iatrogenic biliary injuries: is the robot offering a new option? short clinical report. Ann Surg 267(1):e7–e9. Bing [Internet]. [cited 2021 Dec 5]
Davids PH, Tanka AK, Rauws EA et al (1993) Benign biliary strictures surgery or endoscopy? Ann Surg. 217(3):237–243. Bing [Internet]. [cited 2021 Dec 10]
Tocchi A, Mazzoni G, Liotta G, Costa G, Lepre L, Miccini M et al (2000) Management of benign biliary strictures: Biliary enteric anastomosis vs endoscopic stenting. Arch Surg 135(2):153–157
Kuroda Y, Tsuyuguchi T, Sakai Y et al (2010) Long-term follow-up evaluation for more than 10 years after endoscopic treatment for postoperative bile duct strictures. Surg Endosc 24(4):834–840. Bing [Internet]. [cited 2021 Dec 10]
Skinner M, Popa D, Neumann H, Wilcox C, Mönkemüller K (2014) ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy. 46(7):560–572. Bing [Internet]. [cited 2021 Dec 10]
Parrilla P, Robles R, Varo E, Jiménez C, Sánchez-Cabús S, Pareja E (2014) Liver transplantation for bile duct injury after open and laparoscopic cholecystectomy. Br J Surg 101(2):63–68
Rogers AT, Dirks R, Burt HA, Haggerty S, Kohn GP, Slater BJ, Walsh D, Stefanidis D, Pryor A (2021) Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines development: standard operating procedure. Surg Endosc. 35(6):2417–2427. https://doi.org/10.1007/s00464-021-08469-z. (Epub 2021 Apr 19)
Fletcher DR, Hobbs MST, Tan P, Valinsky LJ, Hockey RL, Pikora TJ et al (1999) Complications of cholecystectomy: risks of the laparoscopic approach and protective effects of operative cholangiography: a population-based study. Ann Surg 229(4):449–457
Kuster GG, Gilroy S, Graefen M (1993) Intraoperative cholangiography for laparoscopic cholecystectomy. Surg Gynecol Obstet 176(5):411–417. [PubMed] [Google Scholar] - Search [Internet]. [cited 2022 Mar 30]
Phillips EH, Berci G, Carroll B, Daykhovsky L, Sackier J, PazPartlow M (1990) The importance of intraoperative cholangiography during laparoscopic cholecystectomy. Am Surg. 56(12):792–795. [PubMed] [Google Scholar] - Search [Internet]. [cited 2022 Mar 30]
Williams HJ Jr, Bender CE, May GR (1987) Benign postoperative biliary strictures: dilation with fluoroscopic guidance. Radiology 163:629–634. Bing [Internet]. [cited 2021 Dec 9]
Stewart L, Way LW (1995) Bile duct injuries during laparoscopic cholecystectomy. Factors that influence the results of treatment. Arch Surg. 130(10):1123–8. discussion 1129. [PubMed] - Search [Internet]. [cited 2022 Mar 30]
Mishra PK, Saluja SS, Nayeem M, Sharma BC, Patil N (2015) Bile duct injury-from injury to repair: an analysis of management and outcome. Indian J Surg 77(Suppl 2):536–42. [PMC free article] [PubMed] - Search [Internet]. [cited 2022 Mar 30]
Snyder E, Kashyap S, Lopez PP. (2023) Hepatobiliary Iminodiacetic Acid Scan. [Updated 2022 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539781/
Blumgart LH, Kelley CJ (1985) Hepaticojejunostomy in benign and malignant high bile duct stricture. Approaches to the left hepatic ducts. Schweizerische Rundschau fur Medizin/Praxis 74(45):1238–44
Ma MX, Jayasekeran V, Chong AK (2019) Benign biliary strictures: prevalence, impact, and management strategies. Clin Exp Gastroenterol. 18(12):83–92. https://doi.org/10.2147/CEG.S165016
Strasberg, Steven M.; Hawkins, William (2006). "Reconstruction of the Bile Duct: Anatomic Principles and Surgical Techniques". In Fischer, Josef E.; Bland, Kirby I.; Caller, Mark P. (eds.). Mastery of Surgery. Lippincott Williams & Wilkins. pp. 1129–42. ISBN 978-0-7817-7165-8
Acknowledgements
We acknowledge all surgical residents from Muhimbili University of Health and Allied Sciences at MNH who actively participated in the perioperative care of these two patients during the course of admission.
Funding
None.
Author information
Authors and Affiliations
Contributions
AYS: gathered the clinical information, did the literature review, conceptualized, and drafted the initial manuscript; AHM: a supervisor, did the literature review, conceptualized, drafted the initial manuscript, and critically reviewed the manuscript; KK: did the literature review and critically reviewed the manuscript; GM: did the literature review and critically reviewed the manuscript; LA: did the literature review and critically reviewed the final manuscript; AA: did the literature review and interpretation of the imaging studies. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was requested from the Institutional Review Board of Muhimbili University of Health and Allied Sciences.
Consent for publication
Written informed consent was obtained from the patients for the publication of this case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Swallow, A.Y., Mwanga, A.H., Kitembo, K. et al. Hepaticojejunostomy in proximal bile duct injury by left hepatic duct approach for patients attended at Muhimbili National Hospital. Egypt Liver Journal 13, 18 (2023). https://doi.org/10.1186/s43066-023-00252-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-023-00252-0