Abstract
Background
Hepatitis C virus (HCV) infection is the global epidemic of this century, affecting almost 100 million people, and it is now the leading cause of liver-related mortality and liver transplantation. Interferon (IFN)-α was introduced as the first treatment for chronic hepatitis C but had several limitations, including factors that cause unresponsiveness to therapy, such as viral and host factors. The availability of non-interferon antiviral agents, direct-acting antivirals (DAAs), has led to a major paradigm shift in the treatment of HCV infection. This therapy has been shown to achieve higher cure rates and minimal side effect profiles in clinical trials. This study is aimed to determine the correlation between host factors, such as age, gender, and body mass index (BMI) with virological response to DAA treatment in hepatitis C patients.
Result
Observational research with a retrospective cohort approach was conducted at Wahidin Sudirohusodo Hospital, Makassar, Indonesia, from April 2021 to October 2021. The virological response was assessed using HCV-RNA quantitative and sustained virological response (SVR) 12 weeks after therapy. The research was conducted on 86 subjects consisting of 57 men and 29 women with a mean age of 48.69±13.94 years and mean BMI of 23.17±3.71 kg/m2, with SVR12 up to 90.7%. Study analysis did not find a significant correlation between age, gender, and BMI, with virological response SVR12 of chronic hepatitis C patients with direct-acting antiviral (p>0.05).
Conclusion
Age, gender, and body mass index do not influence the success of DAA therapy.
Similar content being viewed by others
Introduction
Hepatitis C virus (HCV) infection was one of the global epidemics of this century that infected nearly 100 million people and now is the leading cause of liver and liver transplant-related deaths [1]. Hepatitis C virus is a ribonucleic acid (RNA) virus that is classified as a Flavivirus, generally entering the blood through transfusion or direct exposure to the blood circulation [2]. The main target of HCV is hepatocytes and B lymphocytes through receptors similar to CD81 found on liver cells and B lymphocytes or low-density lipoprotein (LDL) receptors [3].
Hepatitis C is an inflammatory liver disease that is still a health problem in the world, including in Indonesia. Hepatitis C is commonly found in injecting drug users (IDUs) and patients undergoing hemodialysis [4]. Transmission of HCV is mainly through exposure to blood and body fluids contaminated with the hepatitis C virus, including in the era before the use of disposable needles [5].
Since it was first discovered in 1989, hepatitis C therapy has developed quite rapidly. Interferon (IFN)-α was introduced as the first therapy for chronic hepatitis C infection, then enhanced by the pegylation process and the addition of ribavirin, resulting in improving virological response [6].
However, interferon therapy has several limitations, including factors that cause unresponsiveness to therapy, such as viral factors and host factors. The viral factors, such as genotype and viral load, are some factors that influence the virological response. While the host factors, such as elderly, gender, and obesity, are influencing the sensitivity of therapy [7,8,9].
Significant molecular and structural developments in the virology, life cycle, and pathogenesis of HCV led to the discovery of a new therapy, direct-acting antiviral (DAA), which was officially approved for chronic hepatitis C therapy in 2011 [10]. The availability of non-interferon antiviral agents or direct-acting antivirals has led to a major paradigm shift in the treatment of HCV infection. This therapy has been shown to achieve higher cure rates and minimal side effect profiles in clinical trials. However, due to different clinical characteristics and the presence of side effects and comorbidities, antiviral treatment in elderly, male, and obese patients with HCV infection remains a challenge in the present era [1, 7, 11, 12].
A large proportion of patients with chronic HCV infection in the United States are in the 50–70 years age range and have lived with HCV infection for 25–45 years. The extensive duration of HCV infection increases the incidence of liver disease and its associated sequelae. Several theories about old age include susceptibility to environmental factors such as oxidative stress with increasing age, decreased hepatic flow rate, decreased mitochondrial capacity, impaired immunity, and increased carcinogenic potential due to reduced ability to repair DNA [13]. The use of pegylated interferon/ribavirin in the elderly has several limitations. Various comorbidities, side effects, and poor tolerability increase with age in patients. Therefore, in elderly patients, it is often debated whether to start treatment with pegylated interferon/ribavirin [11].
Various studies using DAA therapy in the elderly have shown a better virological response. Studies by Sherigar et al. [14] in the USA and Kamel et al [15] in Egypt reported that the use of DAA therapy was not affected by patient age, which did not significantly affect the rate of virological response.
Hepatitis C virus infection generally affects men more than women, because women are more likely to have spontaneous viral recovery after acute HCV infection [16]. Risk factors such as alcohol consumption in men led to a twofold increase in the progression of fibrosis from HCV infection compared to women [17]. Several theories such as Toll-like receptor 7 (TLR7) play a role in the immune response in HCV infection, where the gene of TLR7 is located on the X chromosome so this might explain the sex difference in HCV infection [18].
Various studies have shown that young women have a better response to interferon therapy than men [19,20,21]. This is thought because of estrogen's role in the inhibition of the liver fibrosis process through an antifibrotic effect that depends on liver tissue receptors and enhances the response to antiviral therapy [20, 21].
Meanwhile, with DAA therapy, a study by Kanwal et al. [22] in the USA and Yunihastuti et al. [23] in Jakarta, Indonesia, found that there was no significant difference in virological response by gender, either male or female who received DAA therapy.
Patients with chronic HCV infection with a high body mass index (BMI) are closely associated with the incidence of steatosis, increased progression of fibrosis, and reduced responsiveness to antiviral therapy. The exact mechanism by which obesity reduces the efficacy of this antiviral therapy remains unclear. One hypothesis is that a high BMI induces the occurrence of metabolic syndrome resulting in insulin resistance, hepatitis steatosis, and a high initial viral load. In addition, obesity also causes interference with cytokine signaling which is manifested in increased levels of leptin, adiponectin, and resistin [24].
With interferon therapy, Alsio et al. [24] in the USA found chronic hepatitis C patients with a BMI of 30 kg/m2 with a virological response of only 62%. Meanwhile, with DAA therapy, studies by Tran et al. [8] in the USA and Hsu et al. [25] in Taiwan found that body mass index did not negatively affect virological response.
Identification of viral and host factors that influence disease progression can help understand the underlying mechanisms of chronic HCV infection [18]. Differences in age, gender, and body mass index sometimes give different results from innovative medical technologies. Meanwhile, in chronic HCV infection, previous studies have shown differences with previous interferon-based therapy based on age, sex, and body mass inde x[7,8,9, 22].
Methods
Aim
The current study aimed to determine the correlation between host factors, such as age, gender, and body mass index with virological response to DAA treatment in hepatitis C patients.
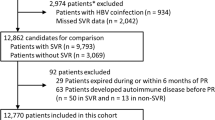
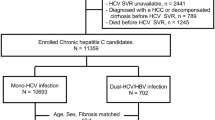
Study design and population
From April 2021 to October 2021, an observational, retrospective, cohort, and single-center study was conducted in Makassar, Indonesia at Wahidin Sudirohusodo Hospital. Eligible subjects were all adult patients with HCV chronic infection patient who started HCV naive therapy with DAA. Patients with hepatitis B coinfection, diabetes mellitus, and/or HCV treatment-experienced before were excluded. The primary endpoint was to determine the correlation between age, gender, and body mass index with virological response to DAA treatment in hepatitis C patients. The secondary endpoint was to determine the virological response to DAA treatment in hepatitis C patients.
Ethical considerations
This study has been approved by the Ethics Committee for Clinical Research of the Faculty of Medicine Hasanuddin University and Dr. Wahidin Sudirohusodo Hospital Makassar (No: 218/UN4.6.4.5.31/PP36/2021). Throughout the investigation process, ethical and data protection protocols related to anonymity and data confidentiality were complied with.
Data collection
Data of age, gender, body mass index, HCV-RNA, and treatment regimen were systematically obtained by reviewing patients’ medical records. All patients were followed up with HCV-RNA at the beginning and 12 weeks after treatment.
Statistical analysis
Data analysis was performed using SPSS software package version 25 (SPSS, Chicago IL). The method of analysis consisted of descriptive methods and statistical tests. The descriptive method aims to obtain general information about the research sample. The statistical method used descriptive statistical calculation and frequency distribution. The statistical test used is the chi-square test. Statistical test results are considered significant if the p-value is <0.05. The results obtained will be displayed in the form of a narrative equipped with tables and pictures.
Results
Baseline characteristics
This study consist of 86 subjects with 57 men (66.3%) and 29 women (33.7%), divided to the age category mostly <60 years with 67 subjects (77.9%). While the youngest was 22 years old and the oldest was 83 years old with a mean age of 48.69±13.94 years. From the BMI category, mostly normal BMI with 44 subjects (51.2%), while overweight and obese 36 subjects (41.9%), the lowest BMI 18.2 kg/m2 and the highest BMI 36.89 kg/m2 with a mean BMI of 23.17±3.71 kg/m2 (Table 1).
Based on descriptive statistics, the initial Log10 HCV-RNA level was 1.0 IU/mL and max 7.61 IU/mL with a mean of 5.63±1.24 IU/mL (Table 2), and the final HCV-RNA level after 12 weeks of therapy, 78 subjects (90.7%) were not detected, and 8 subjects (9.3%) were still detected.
Age with virological response
Analysis of the correlation between age and virological response was carried out using the chi-square test by comparing each category with the achievement of virological response after 12 weeks of DAA therapy or SVR12. No significant relationship was found between age and virological response (p > 0.05) (Table 3).
Gender with virological response
No significant correlation was found between gender and virological response, but the table shows that of the 8 subjects whose virus was detected, 5 subjects (62.5%) were female (p > 0.05) (Table 4).
Body mass index with virological response
There was no significant relationship between BMI and virological response, but the table shows that from 8 subjects whose virus was detected, 6 subjects (75%) were obese and overweight (p > 0.05) (Table 5).
Discussion
In this study with 86 subjects with chronic hepatitis C infection with DAA therapy, 78 subjects (90.7%) had undetectable HCV-RNA 12 weeks after DAA therapy. These results show that the SVR12 of chronic hepatitis C in patients with DAA therapy can reach >90%. Various studies have shown a high SVR12 with pan-genotype regimen DAA therapy, which in this study uses Sofosbuvir and Daclatasvir. Pott et al. [26] (2019) in Brazil on phase 4 randomized experimental study with 65 subjects receiving Sofosbuvir and Daclatasvir therapy, the SVR12 reached 100%. In a retrospective cohort study by Charatcharoenwitthaya et al. [27] (2020) in Thailand, there was a 98% SVR12 with Sofosbuvir and Daclatasvir. The same thing was also found in a meta-analysis conducted by Zoratti et al. [28] of 238 publications, where the SVR12 achievement ranged from 89–97% of genotypes 1–4 in Chronic Hepatitis C patients treated with Sofosbuvir and Daclatasvir.
Meanwhile, with interferon and ribavirin therapy, SVR12 can only be achieved in the range of 41–63% [29,30,31]. Thus, the use of DAA therapy in patients with chronic hepatitis C infection can achieve a higher SVR12 compared to interferon therapy.
Age correlation analysis in our study was carried out with the distribution of categories <60 years and ≥60 years according to WHO criteria, were compared with virological response after 12 weeks of DAA therapy or SVR12, with the results that no significant correlation was found between these two age groups (p > 0.05) (Table 3). The results of this analysis indicate that DAA therapy is well-tolerated, has high efficacy, and can be given to all ages, both adults and the elderly.
Studies by Elbaz et al., Pariente et al., and Nelson et al. supported this finding. In a prospective cohort study by Elbaz et al. [32] (2019) in Egypt in 285 subjects aged 60 years who received sofosbuvir and daclatasvir therapy, it was found that age did not affect the virological response with an SVR12 of 91.9% (p=0.44), with 8.1% failed to achieve SVR12 due to discontinuation of the drug due to adverse events and virological failure due to liver cirrhosis.
In another prospective cohort study by Pariente et al. [33] (2019) in France with 1123 subjects, in the fourth quartile with age 64 years, SVR12 up to 93.2% was achieved in the sofosbuvir and daclatasvir groups, and age did not decrease the virological response (p=044), where age increases exposure and efficacy of sofosbuvir because of a physiological decrease in glomerular filtration rate with age. While in a retrospective observational cohort study by Xia et al. [34] (21) in the USA, with 1106 HCV subjects with various DAA treatment regimens, the overall SVR12 was 97.8% with no significant difference between age and virological response.
Interferon-based regimens in elderly patients are associated with lower virologic response rates, due to side effects and reduced stimulatory effects of interferon on the aging immune system. Meanwhile, with DAA therapy in our study, we could achieve SVR >90% and it was not affected by age.
Analysis of gender correlation in our study found no significant association between men and women (p > 0.05) (Table 4), which differs from gender-dependent interferon therapy [19,20,21], DAA therapy still has high efficacy in both men and women. The observed significance is consistent with the results of prior studies by Margusino et al, Ahmed et al, and Yang et al. In a prospective cohort study by Margusino et al. [35] (2019) in Spain with 111 subjects with chronic HCV who received sofosbuvir and daclatasvir could achieve an SVR12 of 94.6%, where there was no significant difference from SVR12 to gender, both male and female (p=0.19).
Similarly, in a prospective observational study by Ahmed et al. [36] (2018) in Egypt, 249 chronic HCV subjects with SVR12 after receiving sofosbuvir and daclatasvir therapy, reached 96%, with no gender difference between men and women (p>0.05 ). Another prospective observational study by Yang [37] et al. (2019) in China with 498 chronic HCV genotypes 1, 2, and 3 subjects who were treated with sofosbuvir and daclatasvir had an SVR12 of 96.6%, with no difference between gender (p=0.423).
In the interferon era, there were differences in virological responses between males and females, due to faster viral clearance in women than men and hormonal activity, especially estrogen levels. can minimize this difference [16, 20, 21, 38]. And then in the current DAA era, this difference is disappearing which is probably the result of excellent antivirus efficacy so that it can minimize this difference.
The absence of a significant correlation (p>0.05) between BMI and virological response indicates the efficacy of DAA therapy is better than interferon. However, 8 subjects who did not achieve SVR12 found 75% (6 subjects) with obese and overweight. This is thought to occur due to insulin resistance that occurs in obese and overweight patients.
This is consistent with studies conducted by Allam et al., Gupta et al., and Gayam et al. In a prospective cross-sectional study conducted by Allam et al. [39] (2019) in Egypt with 182 chronic HCV subjects treated with sofosbuvir and daclatasvir, the SVR12 achievement was up to 97% with no significant association between obesity and virological response (p>0.05). Likewise in a prospective cohort study by Gupta et al. [40] (2018) in India, with 149 chronic HCV subjects treated with sofosbuvir and daclatasvir, SVR12 was achieved by 97.3% without a significant association between BMI and SVR12 (p>0.05).
Another study using the Sofosbuvir regimen but in combination with other DAAs was conducted by Gayam et al. [41] (2018) in the USA in a retrospective cohort study with 112 chronic HCV subjects with a combination regimen of ledipasvir or velpatasvir, with an SVR12 up to 92%. In the analysis of multivariate logistic regression models, no significant association was found between higher BMI and virological response to SVR12 (p=0.085). In our study, 75% of subjects who did not achieve SVR12 with overweight and obesity BMI could not be analyzed further, because many independent variables were not known.
Conclusion
The virological response of SVR12 with DAA treatment, in this study sofosbuvir and daclatasvir, in chronic hepatitis C patients reached 90.7%, with age, gender, and body mass index do not influence the success of DAA treatment. With a success rate above 90%, DAA therapy can be given to patients with chronic hepatitis C infection with elderly, male or female gender, and obesity. Further research is needed to assess other variables, such as DAA regimen, liver function level, insulin resistance level, liver fibrosis degree, viral genotype, and cirrhotic state.
Availability of data and materials
Data are available on request.
Abbreviations
- HCV:
-
Hepatitis C virus
- IFN:
-
Interferon
- DAA:
-
Direct-acting antiviral
- BMI:
-
Body mass index
- SVR:
-
Sustained virological response
- RNA:
-
Ribonucleic acid
- LDL:
-
Low-density lipoprotein
- TLR7:
-
Toll-like receptor 7
References
Beig J, Orr D, Harrison B, Gane E (2018) Hepatitis C virus eradication with new interferon-free treatment improves metabolic profile in hepatitis C virus-related liver transplant recipients. Liver Transplant 24:1031–1039
Manns MP, Buti M, Gane E et al (2017) Hepatitis C virus infection. Nat Rev Dis Prim 3:1–19
Gani RA (2014) Hepatitis C. In: Setiati S, Alwi I, Syam AF (eds) Buku Ajar Ilmu Penyakit Dalam, VI. Interna Publishing, Jakarta, pp 1972–1977
Waworuntu W, Dwisangka S, Hasan I, Muljono DH (2017) Virologi Dan Perjalanan Penyakit Hepatitis C. In: Panduan Singkat Tatalaksana Hepatitis C, 1st edn. Direktorat Jenderal Pencegahan dan Pengendalian Penyakit Kementerian Kesehatan RI, Jakarta, pp 3–17
Wu GHM, Yang WW, Liu CL et al (2021) The epidemiological profile of chronic hepatitis C with advanced hepatic fibrosis regarding virus genotype in Taiwan: a nationwide study. J Formos Med Assoc 120:1444–1451
Basyte-Bacevice V, Kupcinskas J (2020) Evolution and revolution of hepatitis C management: from non-A, non-B hepatitis toward global elimination. Dig Dis 38:137–142
Soliman EMK, Morsy HAA, Othman AMM, Mady AM (2020) Predictor factors of sustained virological response in patients with chronic hepatitis C treated with current direct-acting antiviral drugs. Trop J Pharm Res 19:2015–2020
Tran K, Kuwajima VK, Tahan V (2018) Impact of Obesity on Treatment of Chronic Hepatitis C in Interferon-Free Direct-Acting Antiviral Era. In: AASLD The Liver Meeting 2018, San Francisco, p 681
Aziz H, Aziz M, Gill ML (2018) Analysis of Host and Viral-Related Factors Associated to Direct Acting Antiviral Response in Hepatitis C Virus Patients. Viral Immunol 31:256–263
Li DK, Chung RT (2019) Overview of Direct-Acting Antiviral Drugs and Drug Resistance of Hepatitis C Virus. In: Methods in Molecular Biology. Humana Press, New York, pp 3–32
Rheem J, Sundaram V, Saab S (2015) Antiviral Therapy in Elderly Patients With Hepatitis C Virus Infection. Gastroenterol Hepatol (N Y) 11:294–346
Hasan I, Gani RA, Sanityoso A, Lesmana CRA (2017) Konsensus Nasional Penatalaksanaan Hepatitis C di Indonesia, 1st edn. Perhimpunan Peneliti Hati Indonesia, Jakarta
Reid M, Price JC, Tien PC (2017) Hepatitis C Virus Infection in the Older Patient. Infect Dis Clin North Am 31:827–838
Sherigar JM, Gayam V, Khan A et al (2017) Clinical efficacy and tolerability of direct-acting antivirals in elderly patients with chronic hepatitis C. Eur J Gastroenterol Hepatol 29:767–776
Kamel S, Elessawy H, Ashraf O et al (2021) Effectiveness of Direct-Acting Antivirals in Treatment of Elderly Egyptian Chronic Hepatitis C Patients. Gastroenterol Insights 12:336–346
Baden R, Rockstroh JK, Buti M (2014) Natural History and Management of Hepatitis C: Does Sex Play a Role? J Infect Dis 209:S81–S85
Bakr I, Rekacewicz C, El HM et al (2006) Higher clearance of hepatitis C virus infection in females compared with males. Gut 55:1183–1187
Yan Z, Wang Y (2017) Viral and host factors associated with outcomes of hepatitis C virus infection (Review). Mol Med Rep 15:2909–2924
Cavalcante LN, Lyra ACAC (2015) Predictive factors associated with hepatitis C antiviral therapy response. World J Hepatol 7:1617–1631
Yu J-W, Sun L-J, Zhao Y-H et al (2011) Impact of sex on virologic response rates in genotype 1 chronic hepatitis C patients with peginterferon alpha-2a and ribavirin treatment. Int J Infect Dis 15:e740–e746
Floreani A, Cazzagon N, Boemo DG et al (2011) Female patients in fertile age with chronic hepatitis C, easy genotype, and persistently normal transaminases have a 100% chance to reach a sustained virological response. Eur J Gastroenterol Hepatol 23:997–1003
Kanwal F, Kramer JR, El-Serag HB et al (2016) Race and Gender Differences in the Use of Direct Acting Antiviral Agents for Hepatitis C Virus. Clin Infect Dis 63:291–299
Yunihastuti E, Hariyanto R, Sulaiman AS, Harimurti K (2021) Hepatitis C continuum of care: Experience of integrative hepatitis C treatment within a human immunodeficiency virus clinic in Indonesia. PLoS One 16:1–10
Alsiö Å, Rembeck K, Askarieh G et al (2012) Impact of Obesity on the Bioavailability of Peginterferon-α2a and Ribavirin and Treatment Outcome for Chronic Hepatitis C Genotype 2 or 3. PLoS One 7:e37521
Hsu SJ, Chiu MC, Fang YJ et al (2019) Real-world effectiveness and safety of glecaprevir/pibrentasvir in Asian patients with chronic hepatitis C. J Formos Med Assoc 118:1187–1192
Pott-Junior H, Bricks G, Grandi G et al (2019) Sofosbuvir in combination with daclatasvir or simeprevir for 12 weeks in noncirrhotic subjects chronically infected with hepatitis C virus genotype 1: a randomized clinical trial. Clin Microbiol Infect 25:365–371
Charatcharoenwitthaya P, Wongpaitoon V, Komolmit P et al (2020) Real-world effectiveness and safety of sofosbuvir and nonstructural protein 5A inhibitors for chronic hepatitis C genotype 1, 2, 3, 4, or 6: a multicentre cohort study. BMC Gastroenterol 20:1–15
Zoratti MJ, Siddiqua A, Morassut RE et al (2020) Pangenotypic direct acting antivirals for the treatment of chronic hepatitis C virus infection: A systematic literature review and meta-analysis. EClinicalMedicine 18:100237
Bressler B, Wang K, Grippo JF, Heathcote EJ (2009) Pharmacokinetics and response of obese patients with chronic hepatitis C treated with different doses of PEG-IFN α-2a (40KD) (PEGASYS®). Br J Clin Pharmacol 67:280
Charlton MR, Pockros PJ, Harrison SA (2006) Impact of obesity on treatment of chronic hepatitis C. Hepatology 43:1177–1186
Luz Narciso-Schiavon J, de Lucca SL, José Carvalho-Filho R et al (2010) Gender influence on treatment of chronic hepatitis C genotype 1. Rev Soc Bras Med Trop 43:217–223
Elbaz T, Abdo M, Omar H et al (2019) Efficacy and safety of sofosbuvir and daclatasvir with or without ribavirin in elderly patients with chronic hepatitis C virus infection. J Med Virol 91:272–277
Pariente A, Arpurt JP, Rémy AJ et al (2019) Effects of age on treatment of chronic hepatitis C with direct acting antivirals. Ann Hepatol 18:193–202
Xia H, Zhang Y, Zaongo SD et al (2021) Direct-acting antiviral treatments display excellent outcomes even in older HCV-infected patients at increased risk of fibrosis. Ann Transl Med 9:1–14
Margusino-Framiñán L, Cid-Silva P, Mena-Decea Á et al (2019) Effectiveness and safety of daclatasvir/sofosbuvir with or without ribavirin in genotype 3 hepatitis c virus infected patients. Results in real clinical practice. Rev Esp Quimioter 32:137–144
Ahmed OA, Safwat E, Khalifa MO et al (2018) Sofosbuvir plus daclatasvir in treatment of chronic hepatitis C genotype 4 infection in a cohort of Egyptian patients: An experiment the size of egyptian village. Int J Hepatol 2018
Yang Y, Wu F-P, Wang W-J et al (2019) Real life efficacy and safety of direct-acting antiviral therapy for treatment of patients infected with hepatitis C virus genotypes 1, 2 and 3 in northwest China. World J Gastroenterol 25:6551–6560
Belci P, Collo A, Martorana M et al (2016) Can gender predict virological response to standard antiviral therapy for chronic hepatitis C? A retrospective study. Hepatoma Res 2:122
Allam AS, Anwar AG, Nasser HM et al (2019) Impact Of Obesity On Sustained Virologic Response To Sofosbuvir Based Regimens In The Egyptian Chronic Hepatitis C Patients. J Egypt Soc Parasitol 49:699–706
Gupta S, Rout G, Patel AH et al (2018) Efficacy of Generic Oral Directly Acting Agents in Patients with Hepatitis C Virus Infection. J Viral Hepat 25:771–778
Gayam V, Mandal AK, Khalid M et al (2018) Sofosbuvir Based Regimens in the Treatment of Chronic Hepatitis C with Compensated Liver Cirrhosis in Community Care Setting. Int J Hepatol 2018:1–9
Acknowledgements
The authors would like to thank all internal medicine residents of Hasanuddin University, Medical Workers of Wahidin Sudirohusodo Hospital, and patients for their participation in this research.
Funding
No funds and other support were received.
Author information
Authors and Affiliations
Contributions
All authors have contributed to and agreed on the content of the manuscript, with the respective roles of each author: RDR, NAD, MLP, and AST drafted the manuscript; RDR and AS collected and analyzed the data; SB, AMA, and HR contributed to the design of the study; which was critically revised by all authors. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee for Clinical Research of the Faculty of Medicine Hasanuddin University and Dr. Wahidin Sudirohusodo Hospital Makassar has approved this study. All patients signed the informed consent and protocols of data protection related to anonymity and data confidentiality were complied with. Committee reference No.: 218/UN4.6.4.5.31/PP36/2021. Date: 5 April 2021.
Consent for publication
The patients in this study had agreed to the publication of data without the appearance of their names.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rusman, R.D., Daud, N.A., Parewangi, M.L. et al. Correlation of host factor with virological response to direct-acting antiviral treatment in hepatitis C patients. Egypt Liver Journal 12, 52 (2022). https://doi.org/10.1186/s43066-022-00217-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-022-00217-9