Abstract
Background
Smoking is the leading risk factor for death worldwide. In Japan, although several evidence-based interventions (EBIs) for smoking cessation have been disseminated or adopted, there is a gap between scientific evidence and the actual implementation. This scoping review aimed to describe the knowledge gaps in local-level smoking cessation interventions in Japan, their implementation outcomes, implementation barriers and facilitators, and the use of implementation strategies.
Methods
This study comprised two approaches: (1) a comprehensive scoping review of primary and grey literature, and (2) a supplemental survey of organizations in the grey literature. For the scoping review, we included original studies or reports on smoking cessation interventions targeting adults aged 18 years and older, or providers of cessation support at various settings (community, workplace, school, and clinical settings) in Japan. The extracted data included basic characteristics, intervention categories, implementation outcomes, factors influencing implementation, and implementation strategies for each intervention. Responses to the supplemental survey were extracted same used for the scoping review. To gain a deeper understanding, semi-structured interviews were conducted with some of the organizations in the survey.
Results
A total of 600 interventions with 691 intervention components, based on EBIs in the 2020 US Surgeon General Report, from 498 articles were included in the data extraction; 32 of the 88 organizations responded to the survey. Regarding the overall knowledge about smoking cessation intervention components, behavioral counseling, and cessation medication in clinical settings were mostly reported (34.7%). Implementation outcomes were measured in 18 articles (3.0%) and penetration was mostly reported. Regarding influential factors, “available resources,” and “knowledge and beliefs about the intervention” for barriers, and “relative priority” for facilitators were mostly reported. Implementation strategies were measured in 29 articles (4.8%), and “Train and educate stakeholders” was mostly reported.
Conclusions
Most EBIs reported in the Japanese literature included smoking cessation treatments in clinical settings. While a few articles focused on the implementation indicators in Japan, significant knowledge and experience were extracted from the grey literature, especially in the workplace and community settings. Future research should focus more on implementation to reduce the knowledge gap regarding smoking cessation interventions.
Similar content being viewed by others
Background
Tobacco use is a major risk factor for cardiovascular and respiratory diseases, and over 20 different types of cancer [1]. In Japan, the smoking prevalence has decreased since 1995. However, the age-adjusted prevalence among adults was 17% in 2019, which is higher than those reported in other developed countries [2].
Evidence of efforts to reduce smoking prevalence is accumulating worldwide [3]. Several EBIs have been systematically implemented in Japan. At an individual level, smoking cessation treatment has been covered by national insurance since 2006 and is available at a copayment of approximately 10–30% of the total fees. In December 2020, smoking cessation treatment apps and carbon monoxide checkers were reimbursed, accelerating online smoking cessation treatments [4]. At a population level, the revised Health Promotion Law went into effect in April 2020, banning smoking indoors in most commercial facilities, restaurants, and offices [5]. While the main purpose of this law revision was to prevent secondhand smoking, it would also reduce smoking prevalence [6]. Regarding approaches for providers, several academic societies have collaborated to establish guidelines for smoking cessation treatments and are working to standardize them [7].
However, the actual implementation of the EBIs is partially limited in Japan. For instance, the number of clinics offering smoking cessation treatment in Japan is approximately 17,000, representing only approximately 15% of all medical facilities, moreover, access is disparate between rural and urban areas [8, 9]. In fact, less than 20% of those who quit smoking used smoking cessation treatment because of a lack of treatment access, lack of media campaigns promoting smoking cessation treatment, and lack of a quitline system [10]. As for smoke-free policies, according to the national survey conducted just one month before the law was fully implemented, approximately 40% of the facilities still allowed indoor smoking [11].
Implementation science aims to promote the adoption and integration of evidence-based interventions into real-world practice [12]. It provides a systematized approach to identifying barriers and facilitators (context of implementation settings), implementation strategies (packages of implementation interventions to address barriers in the context of implementation success), and implementation outcomes (process outcomes of implementation, which indicate implementation success) [13]. To the best of our knowledge, few studies have focused on smoking cessation interventions with an implementation science perspective worldwide, with research being conducted primarily in hospital settings [14,15,16,17,18] and a few in non-hospital settings [19,20,21,22], and no reviews have covered settings such as hospitals, communities, workplaces, and schools. Since the implementation of smoking cessation interventions varies globally, and even within countries despite the existence of global and national tobacco control policies [23], there is a need for studies focusing on implementation in a wide range of settings in a specific country.
In Japan, tobacco control measures at a national level are not sufficiently implemented, as only one element reached the best practice in WHO’s MPOWER measures [2]. On the other hand, a grassroots movement for tobacco control, including smoking cessation support, has been implemented widely and contributed to a decrease in smoking prevalence in Japan [24, 25]. The Japanese government also encourages health promotion effort at a local level, including tobacco control measures, in communities and workplaces, and the MHLW recognizes good practices as part of its Smart Life Project [26]. The Ministry of Economy, Trade and Industry (METI) also recommends health promotions for employees from a health management perspective and certifies companies with outstanding efforts [27]. Understanding the reality of smoking cessation interventions and their implementation in these local settings is useful for other countries that have not reached the best practice level in MPOWER because of a lack of national level policies to further promote smoking cessation support.
This study thus aimed to describe the knowledge gaps regarding local-level smoking cessation interventions in Japan, their implementation barriers and facilitators, and the use of implementation strategies. It focused on local-level interventions because national-level interventions require different implementation strategies owing to the scale and variety of stakeholders involved [28]. The research questions (RQs) in this study were as follows:
-
1)
What kinds of smoking cessation interventions (e.g., smoking cessation programs, support, education, and organizational policies) are provided in Japan?
-
2)
What kind of implementation outcomes are evaluated?
-
3)
What are the barriers and facilitators for the implementation of smoking cessation interventions?
-
4)
What are the implementation strategies to promote the use of smoking cessation interventions?
Methods
In our preliminary screening during the development of the review protocol, we found that the “implementation” of smoking cessation interventions at a local level is limited in primary literature and is more likely to be reported in grey literature, encompassing various document types produced at all levels of the government, academia, businesses, and industries in both print and electronic formats [29]. Scoping reviews involve the synthesis and analysis of a wide range of research and non-research material to provide greater conceptual clarity on a specific topic or field of evidence [30]. Therefore, we decided that a scoping review was the best method for identifying the implementation of smoking cessation interventions in Japan. Furthermore, as information in the grey literature tends to be limited due to reported case studies, we conducted a supplementary survey among the identified organizations reviewed in the grey literature to complement the information regarding the implementation of smoking cessation interventions. Therefore, this study comprised two approaches: (1) a comprehensive scoping review of the primary and grey literature, and (2) a supplemental survey of companies and organizations reported in the grey literature. A detailed description of the methodological steps of this scoping review is provided in our previously published protocol [31].
Scoping review
The scoping review methodological framework described by Arksey and O'Malley was used [32]. The Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) published by Tricco et al. as an extension of the PRISMA statement was followed [33], and our findings were reported in accordance with the PRISMA checklist (Additional file 1).
Literature search strategy and selection criteria
A comprehensive search strategy was reported in the published protocol. The search terms included “tobacco” AND “smoking cessation” OR “health promotion,” in both Japanese and English. The search period was from April 1994, when the first smoking cessation medication was approved in Japan, to September 2022. Searches were conducted in October 2021 for literature from April 1994 to September 2021, and in December 2022 for literature from September 2021 to September 2022 in PubMed, CHINAHL PsycINFO, and Ichushi (a Japanese medical bibliographic database) for peer-reviewed journal articles; and OpenGrey and government reports for grey literature. We reviewed four government sources for grey literature, including (1) Smoking and Health – Report of the Study Group on the Health Effects of Smoking by MHLW [34, 35], (2) the MHLW grants system [36], (3) case studies of the Smart Life Project Award by MHLW [27], and (4) case studies of Health & Productivity Stock Selection Program and the Certified Health & Productivity Management Outstanding Organizations Recognition Program by METI [28], based on consultation with Japanese tobacco researchers. The reference lists of all eligible peer-reviewed journal articles in English were checked for a comprehensive literature search, as suggested by PRISMA-ScR [33].
We included any original studies and reports on smoking cessation interventions targeting adults aged 18 years or older or providers of smoking cessation support. The targeted interventions involved smoking cessation treatment, programs, support, education, and organizational policies aimed at (1) increasing smoking cessation in target populations, primarily focusing on an individual approach; (2) decreasing smoking prevalence in target populations, primarily focusing on a population approach; and (3) developing the skills of individuals engaged in cessation support for adult smokers, primarily focusing on providers. Interventions for the population were included if they were conducted at a local level. Studies that did not primarily focus on tobacco control, did not contain original data, only evaluated drug efficacy, or focused on tobacco control policies at a national or prefectural level were excluded. Studies that did not contain sufficient information about the intervention (studies lacking information on intervention providers, target audience, and intervention settings) were also excluded.
Screening was conducted on two levels. The first screening was performed by reading titles and abstracts, and the second screening was performed by reading full articles. The first screening was conducted by two independent reviewers. The second screening was conducted by one researcher after two independent researchers conducted a pilot test on 10% of the randomly selected articles to confirm understanding of the coding manual among researchers. Conflict in the screening results were discussed at a meeting or via email to reach a consensus. The systematic review approach recommended by Levac et al. was followed for selecting the studies to enhance the rigor of the review [30].
Data extraction
The first and second authors developed a coding manual and template using Excel for data extraction. The unit of coding included each intervention, defined as a combination of provider, target audience, and intervention settings. We recorded basic study characteristics (author, publication year, country, objectives, characteristics of the study population and its size, and study design) and interventions (type of intervention, intervention component, provider, target populations, settings, duration of intervention, control group, recruitment rate, retention rate, and health outcomes) for RQ1; implementation outcomes (i.e., acceptability, appropriateness, adoption, cost, fidelity, penetration, and sustainability [37]) with detailed description, indicator type, and definition for RQ2; factors influencing implementation (facilitators and barriers) for RQ3; and implementation strategies for RQ4.
We defined EBI components for smoking cessation in accordance with the “sufficient” interventions provided in the Surgeon General Report [4] and added two components of “training and awareness programs to health workers” and “public awareness of tobacco consumption risks and benefits of tobacco cessation” from the WHO Framework Convention on Tobacco Control (FCTC) [38]. The interventions that were not EBIs were classified as “others.” Since a smoking cessation intervention could be multilevel, we allowed the selection of up to two intervention components when coding. For instance, when a workplace intervention consisted of a smoke-free policy at the facility and smoking cessation support for smoking employees, this was coded as one intervention and two intervention components (thus, the number of intervention components can be larger than number of interventions). For RQ1, we did not limit EBIs; however, for RQ2–4, we limited the EBIs for data extraction. Implementation outcome was classified according to Proctor’s definition [37]. For penetration, we included penetration to service recipients and service providers (e.g., the number of eligible persons who use a service, divided by the total number of persons eligible for the service; the number of providers who deliver a given service, divided by the total number of providers expected to deliver the service) [37], as well as penetration to service target organizations (e.g., the number of targeted organizations which apply a service, divided by the total number of organizations expected to apply the service). We made a distinction between penetration to service target organizations and adoption at an organization level, depending on the phase of implementation. Organizational adoption was applied when the study focus was on the early phase of project or policy implementation, and organizational penetration was applied when the study focus was on the current situation. Implementation facilitators and barriers were classified using the consolidated framework for implementation research (CFIR) [39], and the implementation strategies were classified using expert recommendations for implementing change (ERIC) [40, 41]. Components of RQ1, 2, and 4 were extracted from the methods section, whereas the components of RQ4 were extracted from the results section in the literature. To ensure consistency in the interpretation of the classified categories, the first and second authors performed a final check. If necessary, the classified categories were edited based on agreement between the first and second authors.
Survey
First, we identified municipalities, organizations, and companies conducting smoking cessation interventions by reviewing (3)(4) of the grey literature and mailing questionnaires to health officers of the identified organizations. (i.e., case studies of (3) Smart Life Project Award by MHLW and (4) Health & Productivity Stock Selection Program and the Certified Health & Productivity Management Outstanding Organizations Recognition Program by METI.) The questionnaire focused on identifying facilitators and implementation strategies. Based on a review article and previous literature in Japan, 22 barriers and facilitators were selected from the CFIR constructs, and 26 implementation strategies were selected from ERIC [21, 42,43,44]. The readability and suitability for the context of the questionnaire items were checked by three health officers implementing health promotion interventions in a Japanese company and a municipal office and revised according to their feedback (see Additional file 2 for detailed question items). The questionnaire survey was conducted in March 2022, and respondents answered either online or on paper. Responses were extracted to the same coding sheet used in the scoping review.
To gain a deeper understanding of the implementation context of the survey responses, qualitative semi-structured interviews were conducted with all organizations that responded that they were available for interviews in the quantitative survey. In the interviews, we aimed to understand the facilitators and implementation strategies that had been mentioned in the cross-sectional survey, including who did what, to whom, when, how often, and what implementation outcomes were aimed for, based on Proctor’s guideline for reporting implementation strategies [45]. Interviews were recorded, and the content was summarized by the interviewers. Qualitative follow-up data were used to complement the authors’ understanding of facilitating factors and implementation strategies in the cross-sectional survey.
The results of both scoping reviews and the survey were summarized in a tabular format, which consists of intervention settings (community, workplace, school, and clinical settings) and intervention components at three levels (provider, population, and individual). We changed the category of hospital setting in our protocol [31] to clinical setting because we included studies in outpatient clinics.
Results
Study characteristics
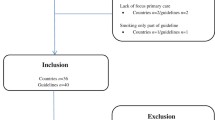
After removing duplicates, 4,764 records were extracted from the database and grey literature sources. A total of 498 articles were finally included after first screening the title and abstract, and secondly screening the full text, as shown in Fig. 1. The final included 420 reviewed articles (81 of them in English and 339 in Japanese) extracted by a database search, 13 peer-reviewed articles (five of them in English and eight in Japanese) added from a manual search of references of English peer-reviewed articles, and 65 articles through grey literature (46 administrative reports and 19 case studies). After the screening was completed, interventions with different target audiences or settings were categorized separately as different interventions, and 600 interventions from 498 articles were included in the data extraction. Details of the intervention characteristics are shown in Additional file 3 (English peer-reviewed articles only due to volume. Information on other articles is available by contacting the corresponding author).
Flow chart. (*The number of gray literature articles (3) case studies of the Smart Life Project Award by MHLW, and (4) case studies of Health & Productivity Stock Selection Program and the Certified Health & Productivity Management Outstanding Organizations Recognition Program by METI is shown separately as they comprise the target of the questionnaire survey)
For the cross-sectional survey, 32 out of 88 organizations identified in the grey literature (19 case studies from MHLW and METI) responded to the survey, 28 of which were businesses, two were municipalities, and two were insurers or non-profit organizations. The role of respondents were public health nurses (n = 14), person in charge in the organization (n = 13), management (n = 2), and others (n = 3). Interviews were conducted with 12 organizations, 11 of which were businesses.
Intervention components and settings
Among the 600 interventions, 691 intervention components were identified and classified by setting, as shown in Table 1. Approaches to providers accounted for 31, approaches to population accounted for 201, and approaches to individuals accounted for 459 of the intervention components, respectively. Behavioral counseling and cessation education accounted for 43.4% of the overall intervention components (300/691 intervention components), while others (interventions not classified as any EBIs) accounted for 19.8% of the same (137/691 intervention components), including smoking cessation advice. EBIs not extracted in this study included quality and performance measures, payment reform, enhancing the technology of electronic health records, quitlines, mass media campaigns, tobacco control programs, proactive behavioral counseling, and short-text message services. By settings, most interventions were conducted in clinical settings (n = 328), while the least were conducted in school settings (n = 53).
Implementation outcomes of smoking cessation interventions
Implementation outcomes were measured in only 18 articles (including four intervention studies), which accounted for only 3.0% of the total identified interventions (18/600 interventions) [46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64], as shown in Table 2. The implementation outcomes measured included penetration (seven interventions), adoption (four interventions), fidelity (four interventions), and acceptability (four interventions). For instance, as a measure of penetration, it was reported that when manuals and educational materials were prepared and training was provided for municipal health workers, the proportion of municipalities that provided brief smoking cessation advice to all smokers on the day of the group-specific health check-up increased 2.6 times in five years [56].
Barriers and facilitators for the implementation of smoking cessation interventions
Barriers and facilitators were extracted from twelve articles [46, 63,64,65,66,67,68,69,70,71,72,73]. Barriers were extracted from seven articles on smoke-free policy and behavioral counseling and cessation medications, and all of them were reported in the clinical setting. Identified barriers were similar between the two interventions, and the most frequently reported barriers were providers’ “knowledge and beliefs about the intervention,” “available resources,” and “patient needs and resources.” A barrier unique to specific hospitals included the “relative advantage” for a smoke-free policy in psychiatric wards, which referred to concerns about the impact of depriving patients of the opportunity to smoke on psychiatric symptoms rather than the effects of secondhand smoke prevention and smoking cessation [46].
Facilitators were extracted from four articles on community and workplace settings. In the articles, “cosmopolitanism,” “knowledge and beliefs about the interventions,” and “formally appointed internal implementation leaders” were reported. Facilitators were also extracted from the survey, with 32 organizations responding to an average of 5.2 facilitators [27, 28]. When the three most reported facilitators in the workplace and community were extracted per intervention, they were distributed across all domains (Table 3 and more details in Additional file 4). The most frequently reported facilitators, including survey results, were “relative priority,” followed by “evidence strength and quality,” and “patient needs and resources.”
Implementation strategies to accelerate smoking cessation interventions
There were 28 articles reporting implementation strategies, accounting for 4.7% of the total identified interventions (28/600 interventions) [51, 56, 74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99]. Nineteen of these were peer-reviewed articles. Implementation strategies were also extracted from the survey, with 32 organizations responding to an average of 11.3 implementation strategies [27, 28]. The three most reported strategies in the workplace and community were extracted per intervention. The most frequently used implementation strategy, including the survey results, was “train and educate stakeholders,” followed by “engage consumers” and “develop stakeholder interrelationships” (Table 4 and more details in Additional file 5). According to the survey results, the most frequently identified strategy was “develop stakeholder interrelationships” in the community (e.g., collaboration between city leaders, city board members, and health advisory committee members regarding tobacco control [example from the interview]) and “adapt and tailor to context” in the workplace (e.g., adjusting measures based on the differences in smoking prevalence and culture among offices and departments, even within the same company [example from the interview]).
Discussion
This scoping review described the knowledge gaps in local-level smoking cessation interventions in Japan, their implementation outcomes, implementation barriers and facilitators, and the use of implementation strategies. Regarding overall knowledge about the smoking cessation intervention components in Japan (RQ1), behavioral counseling and cessation medication in clinical settings were the most commonly used, and articles for community and workplace settings were quite limited. Workplaces have several advantages in implementing health promotion, including smoking cessation interventions, such as enabling access to a large number of people and encouraging sustained peer support and positive peer pressure, which have strong evidence for increasing the prevalence of smoking cessation [100]. While the number of peer-reviewed articles on interventions in workplaces was limited, much knowledge and experience were extracted from the grey literature and supplemental surveys in workplace settings. Moreover, articles on smoking cessation interventions in Japan did not fully cover the list of EBIs reported by the Surgeon General Report. For instance, there are no studies for quitlines despite of strong evidence. To accelerate the implementation of smoking cessation interventions in Japan, there is a need to improve smoking cessation treatment systems, including online treatment, and to develop and disseminate quitline systems [101].
With regard to implementation outcomes (RQ2), a few studies measured them. When an intervention failed to produce the expected effect, this could be caused by either intervention or implementation failure [37]. Measuring implementation outcomes helps us understand the mechanism of success behind implementing an intervention by understanding the implementation process. For instance, fidelity of behavioral counseling can be collected over different time points from various sources such as medical record review (e.g., whether patients were asked, advised, assessed, assisted, or arranged for follow-up) or qualitative approaches included interviews for clinicians or patients [17]. Furthermore, implementation outcomes are not measured only after the implementation. Some implementation outcomes, such as acceptability, can be measured at the pre-implementation phase to each stage of implementation as it is changeable with experience. Since there are already several established EBIs for smoking cessation, it would be beneficial to focus on implementation success by measuring implementation outcomes. None of the 18 articles extracted in this study cited or reported Proctor’s implementation outcome framework. As variations in terminology reporting limited knowledge synthesis across studies [102], future research should use a common taxonomy with conceptual definitions.
Regarding barriers and facilitators (RQ3), the most frequently reported barriers were “available resources,” “knowledge and beliefs about the intervention,” and “patient needs and resources” in clinical settings. These barriers were consistent with previous studies that reported time limitations, low priority, lack of knowledge among healthcare professionals, and providers’ perception that patients were not interested in smoking cessation as barriers to primary care [103, 104], including a scoping review in South Asian regions [105]. The most frequently reported facilitator was “relative priority.” In Japan, the MHLW and METI started awarding and certifying organizations engaged in health promotion in 2012 and 2014, respectively [27, 28]. In addition, a revised Health Promotion Law was enacted in 2018 to reduce secondhand smoking [6]. Thus, these measures at a national level could contribute to prioritizing smoking cessation interventions for organizations. In our study, “patient needs and resources” were reported as both barriers and facilitators. This may be due to differences in implementation phases and settings. While most of barriers were extracted in the implementation phase in clinical settings (e.g., healthcare providers’ hurdles in providing smoking cessation to smokers), most of the facilitators were extracted in the adoption phase in workplace settings as the triggers for introducing smoking cessation interventions in the workplace (e.g., employee complaints about secondhand smoke exposure among non-smoking employees, or requests for implementing measures to support smoking cessation). Regarding implementation strategies (RQ4), the finding that training was the most frequently utilized strategy for smoking cessation interventions in clinical settings was consistent with a previous study [17]. In addition, our study showed that training was utilized not only for behavioral counseling and cessation medication, but also for smoke-free policies, public awareness, and web-based interventions in all settings.
As EBIs have already been established for smoking cessation, it is important to accelerate their implementation. Thus, research should be conducted on methods to increase the evidence of implementation and context by organizing and accumulating barriers, facilitators, strategies, and outcomes within the implementation science framework. In addition, because a knowledge gap was identified through this study, when considering future research funding priorities, it will be possible to prioritize investment in areas where evidence is lacking, which may lead to the promotion of implementation research.
This study has important implications for smoking cessation support practitioners. The findings can be used as a starting point for practitioners to consider what outcomes to measure, what factors may facilitate or inhibit smoking cessation, and what strategies to utilize when implementing a new smoking cessation intervention. For example, when a company is considering the introduction of a new behavioral counseling and cessation medication program, it may be useful to survey the employees’ needs and modify the strategy according to the actual situation in the office, or to consider not only seminars for smokers but also involve the families of employees.
Since this study suggests that organizations conducting smoking cessation interventions have data or insight of implementation outcomes, barriers, facilitators, and strategies, it is important to create reporting tools for implementation outcomes, CFIR, and ERIC that are easy to understand and use for practitioners, encouraging them to accumulate findings in the field. However, because ERIC adopts a conceptual category of implementation strategies, it may not provide enough information for practitioners to utilize. For example, the strategy of “engage consumer” is a large concept, and its sub-items such as “involve patients/consumers and family members” also lack specifics. In our study, we extracted specific examples of “involve patients/consumers and family members,” such as peer-support smoking cessation programs in which smokers and non-smokers are paired to try to quit smoking and a smoking cessation competition by business location, by reviewing case studies and conducting surveys and interviews. Such specific descriptions may be important for practitioners when considering their actions. Therefore, it would be beneficial to include these specific examples along with reporting in the framework of implementation science. Alternatively, utilizing the ERIC compilation and behavior change technique (BCT) taxonomy [106] could be beneficial for both practitioners and researchers to accumulate evidence.
This study also provides important insight for practitioners in countries with lagging tobacco control measures. Even in countries such as Japan, where tobacco control at a national level is insufficient, it could be effective to promote the use of smoking cessation interventions by strengthening the outer setting (i.e., measures by local government, organizational encouragement of health promotion by certificates) and encouraging individual characteristics (i.e., training health workers). Although the Heath & Productivity Stock Selection and Smart Life Projects implemented in Japan do not specifically focus on smoking cessation, they are likely to increase the priority of smoking cessation measures since they are one of the prerequisites for application to them. In addition, smoking cessation treatment is an important measure that can be implemented even if national policies listed in MPOWER are behind it, and the results of this study suggest that improving provider awareness and knowledge is important, since this is a major implementation barrier.
Strengths and limitation of this study
In this study, we extracted findings that could not be extracted from peer-reviewed articles alone, by utilizing grey literature and quantitative and qualitative research. In particular, the supplemental quantitative survey was able to uncover many findings, with an average of 5.2 responses extracted per organization for facilitators and 11.3 responses per organization for implementation strategies. The number of facilitators was limited to four; however, by including the survey results, we were able to extract more facilitators. Regarding implementation strategies, although the number of articles was large, some strategies could only be extracted through the survey, suggesting that hidden knowledge has accumulated in the field. Furthermore, the interviews allowed us to understand the context of the strategies and facilitators. Combining reviews with quantitative and qualitative research, as in this study, may be useful in understanding the implementation of EBIs already in place.
This study had several limitations. First, despite our efforts to conduct a comprehensive review, the limited number of organization survey results was reflected due to low response rate. Additionally, since our survey collected one response per organization, responses might have been influenced by the respondent’s role/position/time at the organization. Second, although we developed detailed coding manuals for systematic analysis and coding, the results may be affected by misclassification of coding. Third, while implementation strategies for interventions in specific settings are typically developed based on previously identified barriers and facilitators, in this study, the influential factors and the implementation strategies were identified independently and may not align with each other. Finally, as the study only included smoking cessation interventions conducted in Japan, the results may not be generalizable to other contexts. However, the findings of barriers and facilitators as well as implementation strategies could provide important insights for other countries where tobacco control measures at a national level are lagging, as in Japan.
Conclusions
This scoping review revealed knowledge gaps regarding local-level smoking cessation interventions in Japan, implementation barriers and facilitators, and the use of implementation strategies. Most EBIs reported in the comprehensively searched Japanese literature involved smoking cessation treatments in clinical settings. While a few articles focused on the implementation of smoking cessation interventions, significant knowledge and experience were extracted from the grey literature, especially in the workplace and community settings. Future research should focus on implementation using an implementation science framework to narrow the knowledge gap regarding smoking cessation interventions in the countries where tobacco control measures at a national level are lagging.
Availability of data and materials
The datasets used and/or analyzed in this study are available from the corresponding author upon reasonable request.
References
World Health Organization. Tobacco. https://www.who.int/health-topics/tobacco Accessed 13 Mar 2023.
World Health Organization. WHO report on the global tobacco epidemic, 2021: Addressing new and emerging products fresh and alive. Geneva: World Health Organization; 2021. https://www.who.int/publications/i/item/9789240032095. Accessed 13 Mar 2023.
U.S. Department of Health and Human Services. Smoking cessation: a report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. 2020. [https://www.hhs.gov/sites/default/files/2020-cessation-sgr-full-report.pdf. Accessed 13 Mar 2023.
Ministry of Health, Labor, and Welfare. What is a smoking cessation treatment? e-healthnet. https://www.e-healthnet.mhlw.go.jp/information/tobacco/t-06-007.html. Accessed 13 Mar 2023.
Ministry of Health, Labor, and Welfare. Stop! Unwanted secondhand smoking. https://jyudokitsuen.mhlw.go.jp/. Accessed 2 Mar 2022.
Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behavior: systematic review. BMJ. 2002;325:188.
The Japanese Circulation Society, The Japan Lung Cancer Society, Japanese Cancer Association, The Japanese Respiratory Society. Standard procedure for smoking cessation treatment (8th Edition). Tokyo: Authors; 2021. https://www.j-circ.or.jp/kinen/anti_smoke_std/. Accessed 13 Mar 2023.
Yoshimi I. Prefectural comparison using smoking and smoking cessation items in the 2nd NDB open data. J Health Welf Stat. 2018;65:18–23.
Japan Society for Tobacco Control. List of smoking cessation clinics in Japan. 2021. http://www.nosmoke55.jp/nicotine/clinic.html. Accessed 13 Mar 2023.
Ministry of Health Labor and Welfare. Factsheet 3: smoking cessation support and treatment (in Japanese). 2018. https://www.e-healthnet.mhlw.go.jp/information/pdf/factsheet05.pdf. Accessed 13 Mar 2023.
Ministry of Health, Labor and Welfare. Survey results about the smoking environment in 2019. 2020. https://www.mhlw.go.jp/toukei/saikin/hw/kenkou/kituen/r01/index.html. Accessed 13 Mar 2023.
Eccles MP, Mittman BS. Welcome to implementation science. Implement Sci. 2006;1:1.
Bauer MS, Damschroder L, Hagedorn H, Smith J, Kilbourne AM. An introduction to implementation science for the non-specialist. BMC Psychol. 2015;3:1–12.
de Ruijter D, Mergelsberg E, Crone M, Smit E, Hoving C. Identifying active ingredients, working mechanisms, and fidelity characteristics reported in smoking cessation interventions in Dutch primary care: a systematic review. Nicotine Tob Res. 2022;24:654–62.
France EK, Glasgow RE, Marcus AC. Smoking cessation interventions among hospitalized patients: what have we learned? Prev Med. 2001;32:376–88.
Sharpe T, Alsahlanee A, Ward KD, Doyle F. Systematic review of clinician-reported barriers to provision of smoking cessation interventions in hospital inpatient settings. J Smok Cessat. 2018;13:233–43.
Ugalde A, White V, Rankin NM, Paul C, Segan C, Aranda S, et al. How can hospitals change practice to better implement smoking cessation interventions? A systematic review. CA Cancer J Clin. 2022;72:266–86.
Selove R, Neil-Sztramko S, Leng J, Walker PD, Salloum RG, Ginossar T, et al. Use of implementation science in tobacco control intervention studies in the USA between 2000 and 2020: a scoping review protocol. BMJ Open. 2020;10: e038617.
Parkinson R, Jessiman-Perreault G, Frenette N, Allen Scott LK. Exploring multilevel workplace tobacco control interventions: a scoping review. Workplace Health Saf. 2022;70:368–82.
Mlinarić M, Hoffmann L, Kunst AE, Schreuders M, Willemsen MC, Moor I, et al. Explaining mechanisms that influence smoke-free implementation at the local level: a realist review of smoking bans. Nicotine Tob Res. 2019;21:1609–20.
Wolfenden L, Goldman S, Stacey FG, Grady A, Kingsland M, Williams CM, et al. Strategies to improve the implementation of workplace-based policies or practices targeting tobacco, alcohol, diet, physical activity and obesity. Cochrane Database Syst Rev. 2018;11(11):CD012439.
McFadyen T, Chai LK, Wyse R, Kingsland M, Yoong SL, Clinton-McHarg T, et al. Strategies to improve the implementation of policies, practices or programs in sporting organizations targeting poor diet, physical inactivity, obesity, risky alcohol use or tobacco use: a systematic review. BMJ Open. 2018;8: e019151.
Hebbar PB, Dsouza V, Bhojani U, Prashanth NS, van Schayck OC, Babu GR, et al. How do tobacco control policies work in low-income and middle-income countries? A realist synthesis. BMJ Glob Health. 2022;7(11): e008859.
Murphy F, Crossley G. Smoking cessation: State owned tobacco companies in China and Japan are at odds with their countries’ commitments. BMJ. 2019;365:l2328.
Maki K, Kayoko K. Review of literature on the state of smoking cessation support in Japan (in Japanese). J Jpn Acad Commun Health Nurs. 2012;15:133–43.
Ministry of Health Labor and Welfare. Smart Life Project Award. https://www.smartlife.mhlw.go.jp/award/. Accessed 2 Feb 2022.
Ministry of Economy Trade and Industry. Health & Productivity Stock Selection Program, and Certified Health & Productivity Management Outstanding Organizations Recognition Program. https://www.meti.go.jp/policy/mono_info_service/healthcare/kenko_keiei.html. Accessed 2 Feb 2022.
Katanoda K, Jiang Y, Park S, Lim MK, Qiao YL, Inoue M. Tobacco control challenges in East Asia: proposals for change in the world’s largest epidemic region. Tob Control. 2014;23:359–68.
Schopfel J. Towards a Prague definition of grey literature. [Published online first, 2010]. https://lilloa.univ-lille.fr/handle/20.500.12210/71858.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implementation Sci. 2010;5:1–9.
Nagasawa T, Saito J, Odawara M, Imamura H, Kaji Y, Yuwaki K, et al. Smoking cessation interventions and implementations in Japan: a study protocol for a scoping review and supplemental survey. BMJ Open. 2022;12(12): e063912.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Ministry of Health, Labor, and Welfare. Smoking and Health – Report of the Study Group on the Health Effects of Smoking (new edition). (in Japanese). Health Dojinsha. 2002.
Ministry of Health Labor and Welfare. Smoking and Health – Report of the Study Group on the Health Effects of Smoking (2016). (in Japanese). 2016. https://www.mhlw.go.jp/stf/shingi2/0000135586.html. Accessed 13 Mar 2023.
Ministry of Health, Labor, and Welfare. MHLW grants system. https://mhlw-grants.niph.go.jp/. Accessed 2 Feb 2022.
Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38:65–76.
World Health Organization. WHO Framework Convention on Tobacco Control. Geneva: World Health Organization; 2003. https://www.who.int/fctc/text_download/en/. Accessed 13 Mar 2023.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;7(4):50.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:1–14.
Waltz TJ, Powell BJ, Matthieu MM, Damschroder LJ, Chinman MJ, Smith JL, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. 2015;10:1–8.
Kava CM, Ruiz RA, Harris JR, Hannon PA. Worksite tobacco control - a qualitative study on perspectives from employers and employees at small worksites. BMC Public Health. 2022;22:904.
Saito J, Odawara M, Takahashi H, Fujimori M, Yaguchi-Saito A, Inoue M, et al. Barriers and facilitative factors in the implementation of workplace health promotion activities in small and medium-sized enterprises: a qualitative study. Implement Sci Commun. 2022;3:23.
Odawara M, Saito J, Yaguchi-Saito A, Fujimori M, Uchitomi Y, Shimazu T. Using implementation mapping to develop strategies for preventing non-communicable diseases in Japanese small- and medium-sized enterprises. Front Public Health. 2022;10: 873769.
Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8:139.
Hashimoto K, Makinodan M, Matsuda Y, Morimoto T, Ueda S, Kishimoto T. Smoking bans in mental health hospitals in Japan: barriers to implementation. Ann Gen Psychiatry. 2015;14:35.
Katsumata Y, Kobayashi M, Hamano N. Effects of using smoking cessation cards on pregnant women who smoke and their husbands who smoke (in Japanese). Proceedings of the Nursing Association of Japan: maternal nursing. 2013;43:26–9.
Kawabe M, Kojima M, Nagaya T, Suzuki S. Effects on the attitudes and behaviors of facility users as a result of the implementation of a total smoking ban at the university and affiliated hospitals (in Japanese). Jpn J Public Health. 2011;58:266–73.
Komaki K, Yoshida Y, Suzuki S, Nasuno J, Ichimura A, Arai M, et al. Effect of a 5-year total ban on smoking in Saitama Prefectural University (in Japanese). Kinen Kagaku. 2011;4:1–5.
Tanaka M, Tanaka H, Taniuchi K. Implementation of clinical paths to support smoking cessation in specialized oncology hospitals (in Japanese). J Health Welf Stat. 2009;56:13–9.
Ozaki I, Konishi M, Katakura K. A Study on practicable and effective e-mail-based intervention methods for improving lifestyles (in Japanese). J Jpn Acad Commun Health Nurs. 2008;10:33–9.
Hagimoto A, Masui S, Nakamura M, Bai Y, Oshima A. Effects of skill level on individual behavioral for smoking cessation (in Japanese). Jpn J Public Health. 2007;54:486–95.
Hasuo S, Tanaka H, Wakisaka S, Yuasa M, Tomonari K, Oshima A. Efficacy of nurses on the job training to better advise cessation among hospitalized smokers (in Japanese). Jpn J Public Health. 2004;51:496–506.
Lee JS, Kawakubo K, Kawamura H. Assessment of worksite health promotion environment (in Japanese). J Occup Health. 2003;45:57–66.
Masaki K, Tateno H, Nomura A, Muto T, Suzuki S, Satake K, et al. A randomized controlled trial of a smoking cessation smartphone application with a carbon monoxide checker. NPJ Digit Med. 2020;3:35.
Tsuji I. Research on the promotion of Health Japan 21 (second term) (in Japanese). MHLW Grants System. 2015. https://mhlw-grants.niph.go.jp/project/25287 Accessed 13 Mar 2023.
Shimomitsu T. Research on setting effective development measures and policy targets for health promotion support environments (in Japanese). MHLW Grants System. 2010. https://mhlw-grants.niph.go.jp/project/18118. Accessed 13 Mar 2023.
Hayashi K. Research on support and promotion of comprehensive measures for health promotion through tobacco control (in Japanese). MHLW Grants System. 2009. https://mhlw-grants.niph.go.jp/project/16562. Accessed 13 Mar 2023.
Inoue H. Research on the effectiveness of smoking control measures through collaboration between medical institutions and municipal health centers (in Japanese). MHLW Grants System. 2003. https://mhlw-grants.niph.go.jp/project/9061. Accessed 13 Mar 2023.
Nakahara T. A Study on the community health service based on habitants/consumers by applying social marketing theory. (summary research report) (in Japanese). MHLW Grants System. 2000. https://mhlw-grants.niph.go.jp/project/4742. Accessed 13 Mar 2023.
Nakahara T. A Study on the community health service based on habitants/consumers by applying social marketing theory (in Japanese). MHLW Grants System. 1998. https://mhlw-grants.niph.go.jp/project/2748. Accessed 13 Mar 2023.
Kawai A, Kitada M, Nakai M, Abe T, Iida M, Ostubo Y, et al. Promoting smoke-free psychiatric hospitals prior to the amended Health Promotion Act – how did the amended Health Promotion Act change smoking measures in psychiatric hospitals? (in Japanese). Jpn J Tob Control. 2021;16:74–82.
Sezai I, Taniguchi C, Yoshimi I, Hirano T, Wakao F. How self-efficacy toward, perceived importance of, and beliefs about smoking cessation support impact-related behaviors in Japanese nursing professionals (in Japanese). Int J Environ Res Public Health. 2022;19:2304.
Yamamura Y, Togari T, Matsuoka H. A study of the implementation status of dental hygienist–enabled smoking cessation support and related factors (in Japanese). J Jpn Soc Dent Hyg. 2022;16:25–37.
Kai T, Maki T, Takahashi S, Warner DO. Perioperative tobacco use interventions in Japan: a survey of thoracic surgeons and anesthesiologists. Br J Anaesth. 2008;100:404–10.
Li M, Okamoto R, Tada A, Kiya M. Factors Associated with prenatal smoking cessation interventions among public health nurses in Japan. Int J Environ Res Public Health. 2020;17:6135.
Michibayashi C, Omote S, Nakamura M, Okamoto R, Nakada AI. Competency model for public health nurses working on tobacco control in local governments in Japan: a qualitative study (in Japanese). Jpn J Nurs Sci. 2020;17: e12288.
Shinmura H, Kayaba K, Kunisawa N, Wakabayashi C, Yanagawa H. A nationwide survey of municipalities’ policy for smoking control and its implementation in relation to its priority grading by public health officers (in Japanese). Jpn J Public Health. 2004;51:814–21.
Nagao T, Fukuta J, Hanioka T, Nakayama Y, Warnakulasuriya S, Sasaki T, et al. A multicenter tobacco cessation intervention study in the dental setting in Japan. Int Dent J. 2022;72:123–32.
Arima S, Yayama S, Mikami H, Tanigawa M, Minegishi H, Tanaka A, et al. The status of smoking cessation support by nurses in general hospitals, and related factors (in Japanese). Jpn J Public Health. 2010;57:203–13.
Matsuda A, Hasegawa J, Tominaga M, Watanabe K, Yoshida M, Abe H, et al. Status of smoking cessation guidance for physicians and patients: examination by Tottori Medical Association (in Japanese). J Tottori Med Assoc. 2005;33:181–7.
Yamahata A, Sato H, Fukuma S, Minagawa N, Abe M. The pharmacist’s role in smoking lntervention and suggestions for future involvement (in Japanese). J Jpn Soc Hosp Pharm. 2004;40:697–701.
Tanihata T. Study on the status and evaluation of tobacco control measures by health centers and the "Healthy Japan 21 Local Plan" of prefectures and municipalities. (summary study report) (in Japanese). MHLW Grants System. 2002 https://mhlw-grants.niph.go.jp/project/7376. Accessed on 14 March 2023.
Onda M, Kuwanoe T, Hashimoto A, Horiguchi M, Domichi M, Sakane N. Pharmacist-delivered smoking cessation program in community pharmacy (the FINE program) in Japan-the development of a training course and a feasibility study. J Pharm Pract. 2021;34:625–30.
Tanaka K, Senjyu H, Tawara Y, Tanaka T, Asai M, Tabusadani M, et al. Effects of systematic intervention for chronic obstructive pulmonary disease on follow-up and smoking cessation rates and changes of the pulmonary function: a 7-year longitudinal study in a Japanese rural city. Intern Med. 2018;57:2315–23.
Tanaka H, Yamato H, Tanaka T, Kadowaki T, Okamura T, Nakamura M, et al. Effectiveness of a low-intensity intra-worksite intervention on smoking cessation in Japanese employees: a three-year intervention trial. J Occup Health. 2006;48:175–82.
Kadowaki T, Okamura T, Funakoshi T, Okayama A, Kanda H, Miyamatsu N, et al. Effectiveness of annual interventions for smoking cessation in an occupational setting in Japan. Environ Health Prev Med. 2004;9:161–4.
Hanioka T, Ojima M, Tanaka H, Naito M, Hamajima N, Matsuse R. Intensive smoking-cessation intervention in the dental setting. J Dent Res. 2010;89:66–70.
Watanabe F, Shinohara K, Dobashi A, Amagai K, Hara K, Kurata K, et al. Assessment of assistance in smoking cessation therapy by pharmacies in collaboration with medical institutions- implementation of a collaborative drug therapy management protocol based on a written agreement between physicians and pharmacists. Yakugaku Zasshi. 2016;136:1243–54.
Yoshinaga A, Kurosawa K. “Sociability”-based smoking cessation program in a workplace that made all 11 challengers quit smoking for 3 months (in Japanese). Kinen Kagaku. 2018;12:1–11.
Matsumoto N, Takada M, Shima T. Construction of smoking cessation support system to preoperation patients and roles of non-smoking outpatient nurse (in Japanese). Med J Jpn Red Cross Kyoto Daiichi Hosp. 2018;1:100–4.
Nagao T, Seto K, Fukuda J, Kurita K, Sato Y, Kitagawa Y, Kusama M, et al. Effectiveness of smoking cessation interventions for oral disease multicenter study (in Japanese). J Jpn Assoc Dent Sci. 2018;37:52–7.
Mori M, Hoshi Y, Takahashi W, et al. Successfully reduced smoking rates accomplished by encouragement of smoking cessation at annual health check-up (in Japanese). Jpn J Tob Control. 2012;7:103–8.
Kawasaki T, Shikaura S, Matsui M, Ushikubo A. Evaluation of the usefulness of valenicline in the workplace: first report of a pilot study (in Japanese). Matsushita Med J. 2011;50:79–85.
Ishikawa M, Yukari I, Hamanaka Y, Nakama K, Ueki A, Takamura H. From the nurses’ station smoking status and smoking cessation guidance for diabetic patients in our hospital (in Japanese). Practice. 2009;26:320–6.
Nakai K, Takahashi Y, Kiyohara K. Outcomes of a smoking cessation support intervention for smoking college students in a university smoke-free project (in Japanese). Kinen Kagaku. 2008;2:22–8.
Matsui T, Takagaki S, Okane R, Okada Y, Yasumoto Y. Current status of smoking cessation treatment at our hospital: by efforts as a team medicine (in Japanese). J Kyoto Med Assoc. 2008;55:97–100.
Abe M, Yauchi M. No-smoking policy on the premises of Ishinomaki Red Cross Hospital (in Japanese). Jpn Red Cross Med J. 2008;58:389–92.
Matsuzawa Y, Fujimoto K, Kubo K. Effects of passive smoking control measures and individual smoking cessation guidance on smoking rates in the workplace (in Japanese). J Jp Soc Resp Care Rehab. 2007;17:143–7.
Yasuda T, Konno Y, Okino M, Fukuda M, Takaoka K, Hotta D, et al. A manual on smoking-cessation for out-patients for all doctors (in Japanese). J Sapporo Soc Insur Gen Hosp. 2005;14:84–7.
Hata Y, Yasuda H, Mitsuhashi K, Takebayashi T, Takaoka K, Hotta D, et al. The program for the complete smoking cessation project in our hospital and the project-related problems we have experienced (in Japanese). J Sapporo Soc Insur Gen Hosp. 2003;50:298–302.
Ohbayashi H, Akita H, Nosaka H, Yamase H. The efficacy of comprehensive smoking cessation class, combined with nicotine patch and gum replacement therapy (in Japanese). Ann J Resp Soc. 2001;39:732–8.
Hayashi M, Nakagawa T, Kusano R, Narita K, Yonehara Y, Akutsu M, et al. Smoking prevention in the workplace outpatient department for smoking cessation and smoking cessation classes by “Shien-no-kai” (in Japanese). Hitachi Med J. 2006;44:29–31.
Nakamura M. Research on the development of an environment for effective smoking cessation that contributes to reducing cancer risk, the development of support measures, and the institutionalization of measures to promote smoking cessation (in Japanese). MHLW Grants System. 2013. https://mhlw-grants.niph.go.jp/project/22511. Accessed on 14 March 2023.
Kishimoto T. Establish comprehensive smoking cessation measures for mental disabilities (in Japanese). MHLW Grants System. 2011. https://mhlw-grants.niph.go.jp/project/19854. Accessed on 14 March 2023.
Kawahara K. Research on technical support for local health promotion plans (in Japanese). MHLW Grants System. 2005. https://mhlw-grants.niph.go.jp/project/11917. Accessed on 14 March 2023.
Yamato H. Research on the effectiveness of comprehensive smoking control measures consisting of space separation and smoking cessation support, and dissemination of effective smoking control programs (in Japanese). MHLW Grants System. 2004. [https://mhlw-grants.niph.go.jp/project/10499. Accessed on 14 March 2023.
Oshima A. A study on comprehensive intervention and its evaluation for smoking habit in the community (summary research report) (in Japanese). MHLW Grants System. 1999. https://mhlw-grants.niph.go.jp/project/3743. Accessed on 14 March 2023.
Kashima O, Kawamoto H. Utilize the Medical Association-run PCR Center to educate citizens and physician members and verify the Gyoda model (smoke prevention classes for all elementary school students in the city, same-day survey at the coming-of-age ceremony) (in Japanese). J Saitama Med Soc. 2022;56:154–8.
Cahill K, Lancaster T. Workplace interventions for smoking cessation. Cochrane Database Syst Rev. 2014;(2):CD003440.
Nakamura M. Factsheet 7: smoking cessation support and treatment. Tokyo. Japan Association for Development of Community Medicine. 2021.
Lengnick-Hall R, Gerke DR, Proctor EK, Bunger AC, Phillips RJ, Martin JK, et al. Six practical recommendations for improved implementation outcomes reporting. Implement Sci. 2022;17:16.
Meredith LS, Yano EM, Hickey SC, Sherman SE. Primary care provider attitudes are associated with smoking cessation counseling and referral. Med Care. 2005;43:929–34.
Tildy BE, McNeill A, Perman-Howe PR, Brose LS. Implementation strategies to increase smoking cessation treatment provision in primary care: a systematic review of observational studies. BMC Prim Care. 2023;24:32.
Iqbal S, Barolia R, Petrucka P, Ladak L, Rehmani R, Kabir A. Smoking cessation interventions in South Asian Region: a systematic scoping review. BMC Public Health. 2022;22:1096.
McHugh S, Presseau J, Luecking CT, Powell BJ. Examining the complementarity between the ERIC compilation of implementation strategies and the behavior change technique taxonomy: a qualitative analysis. Implement Sci. 2022;17:56.
Acknowledgements
We thank Dr. Kota Katanoda, Dr. Kimiyasu Hirano, Dr. Chie Taniguchi, Dr. Izumi Sezai, Dr. Makoto Watanabe, Dr. Fumihiko Wakao, and Dr. Yosuke Uchitomi for their valuable comments on the research; Ms. Keiko Kato, a librarian at the National Cancer Center, for technical support in searching the literature. We also gratefully acknowledge the support provided by the National Center Consortium in Implementation Science for Health Equity (N-EQUITY), funded by the Japan Health Research Promotion Bureau (JH) Research Fund (No 2019-(1)-4), and JH Project fund (JHP2022-J-02). We are also grateful to four health officers, Ms. Keiko Takeda, Ms. Kana Yamamoto, Mr. Noboru Komatsu, and Mr. Kenta Teramoto, for their meaningful feedback on the validity of the survey items. In addition, we are also grateful for Ms. Hikari Nagao, Ms. Risa Kato, Ms. Emi Ibusuki, Ms. Hanako Saito, and Ms. Mari Ikeda for her cooperation with this study as a research staff member.
Funding
This work was supported by a Health Labor Sciences Research Grant (Comprehensive Research on Lifestyle Related Diseases, including Cardiovascular Diseases and Diabetes Mellitus) from the Ministry of Health, Labour and Welfare (Program Grant Number JPMH21FA1001, JPMH23FA1001), the National Cancer Center Research and Development Fund (30-A-18, 2021-A-19), and the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant-in-Aid for Scientific Research (21K17319).
Author information
Authors and Affiliations
Contributions
JS, TN, and TS conceived the idea and developed the research questions and methods. JS and TN facilitated each stage of the scoping review. TN, JS, MO, HI, YK, KY, and KN conducted the screening, data charting, and categorized the extracted data. TN and JS contributed meaningfully to the drafting and editing of the manuscript. MO, HI, YK, KY, KN, and MN aided in developing the research questions and study methods. All authors critically reviewed and revised the manuscript regarding its content and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All data for this project were collected by searching online literature databases and websites, as well as surveying workplaces and organizations. Approval from the Ethical Committee of the National Cancer Center in Japan was not required because the subject of the survey included the worksite or organization and not an individual. The survey aimed to ask about the objective situation of the workplace or organization rather than any subjective information, and no personal information was collected.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA Checklist.
Additional file 2.
Survey Questionnaire.
Additional file 3.
Table 1 with detail (English literature only).
Additional file 4.
Table 3 with detail.
Additional file 5.
Table 4 with detail.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nagasawa, T., Saito, J., Odawara, M. et al. Smoking cessation interventions and implementations across multiple settings in Japan: a scoping review and supplemental survey. Implement Sci Commun 4, 146 (2023). https://doi.org/10.1186/s43058-023-00517-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43058-023-00517-0




