Abstract
Background
The long saphenous vein is one of the most used conduits for coronary artery bypass graft surgery. The aim of this study was to assess the existing evidence regarding the effects of preoperative ultrasound mapping of the long saphenous vein with special attention to leg wound complications in patients undergoing elective coronary artery bypass graft surgery.
Main text
A systematic literature search was conducted in PubMed, Cochrane, and Embase databases. Extraction of relevant data was performed including study characteristics, patient characteristics, and all reported outcomes. The Cochrane Risk of Bias tool was used to evaluate the risk of bias of the included studies. The primary outcome measure was leg wound infections.
Of 4514 papers screened in this systematic review, 36 papers underwent full-text assessment with final inclusion of 5 studies; 3 observational studies, and 2 randomized trials. The two randomized controlled trials showed no effects of preoperative ultrasound. Data from the three non-randomized studies was pooled in a meta-analysis, which suggested a significant reduction in the risk of harvest wound complications by ultrasound mapping prior to surgery (RR 0.32; 95%CI = [0.19–0.55]).
Conclusions
The main findings of this systematic review showed, that (1) the evidence in this field is limited and of low quality, i.e., low power or methodology and (2) despite limitations of the included studies, preoperative ultrasound mapping of the saphenous vein seems to be beneficial in terms of reducing the risk of postoperative leg wound complications.
Similar content being viewed by others
Background
Cardiovascular disease is the leading cause of deaths world-wide according to the World Health Organization, causing 17.9 million deaths annually [1]. Coronary artery disease (CAD) is the most prominent cause of morbidity and mortality [2]. Due to advances in both surgical techniques and percutaneous coronary intervention, an increasing percentage of patients with CAD are eligible for myocardial revascularization [3]. Coronary artery bypass grafting (CABG) remains the standard of care for patients with three-vessel or left main CAD and improves myocardial ischemia, cardiac function, and cardiac-related mortality rates [2, 4, 5]. CABG requires autologous conduits; one of the most frequently used is the long saphenous vein (LSV) [6, 7].
The reported incidences of wound related complications after LSV harvest ranges from 2 to 20% [8, 9]. Commonly reported leg wound complications related to saphenous vein harvesting include surgical site infection, pain, swelling, and impaired mobility [6]. Such complications are a major cause of patient morbidity, resulting in prolonged hospital stay and delayed recovery with the need for additional interventions such as debridement, antibiotic therapy, and dressing changes [6, 10, 11].
Ultrasonography (US) for preoperative vein mapping has been used to assess and determine the anatomical course of the LSV, thereby facilitating rapid and accurate location of the vein during surgery [12, 13]. Furthermore, preoperative vein mapping has been suggested to be of value in patients whose veins are not evident by physical examination due to edema, multiple varicosities, or complex saphenous vein anatomy [14]. Thus, unnecessary incisions can be avoided reducing complications at incision sites and wound healing disturbances [12].
A previous Best Bet study from 2013 supports the use of preoperative ultrasound assessment of the saphenous vein [15, 16]. However, only one of the included studies was comparing ultrasound mapping with conventional vein harvest [16]. Therefore, the aim of this present systematic review was to determine whether preoperative ultrasound mapping of the LSV reduces leg wound complications compared to conventional vein harvest.
Main text
Search strategy
The data search was performed on May 10th, 2022. This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [17]. No ethics approval was required for this review.
Publications were identified through a search of online databases: Cochrane Central Register of Controlled Trials, PubMed, and EMBASE. The search was not limited by language or publication status, and no date restriction was implemented. Following search terms were used to search the PubMed and adapted appropriately for EMBASE and Cochrane: (((“Coronary Artery Bypass”[Mesh]) OR (coronary bypass)) OR (cabg)) AND ((((“Ultrasonography”[Mesh]) OR (ultrasound)) OR (ultrasonics)) OR (mapping))) AND (((“Veins”[Mesh]) OR (saphenous)) OR (vein)). The bibliographies of all included studies were hand-searched for any relevant references that may have been missed by the literature searches.
Eligibility criteria
Citations retrieved from all literature sources were collated into an EndNoteTM 20 library. Eligible studies were included if they met the following inclusion criteria: participants were adults (18 years or older); participants were undergoing elective isolated CABG surgery with LSV as conduit; studies evaluating ultrasound mapping of the LSV prior CABG surgery compared to conventional harvesting; study designs included were randomized controlled trials (RCTs) and prospective and retrospective cohort studies, respectively.
Reviews and case reports were excluded.
Primary outcome measure
Occurrence of leg wound complications following harvest of the saphenous vein.
Secondary outcome measures
Additional leg incision, leg incision length, and harvest time.
Assessment of study eligibility
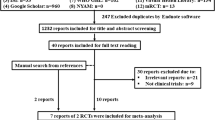
In accordance with the inclusion and exclusion criteria, titles and abstracts were screened on Covidence software (www.covidence.org) independently by two authors (AIE-A, RR). Full-texts articles were assessed for eligibility using a modified Cochrane Data Extraction Template. The review authors were not blinded to the authors’ names and affiliations. A consensus of the two reviewers was needed to include the studies in the literature review (Fig. 1).
Data extraction
The following data were extracted from the eligible studies: demographic information, study design, intervention details, and all reported outcomes. Data were only extracted if stated in the text or tables of the article, not in graphic representations.
Quality assessment
The possible risk of bias was assessed using either the Cochrane Risk of Bias Assessment [18] or the ROBINS-I tool [19] for the RCTs [20, 21] and non-RCTs [6, 12, 22], as appropriate (Table 1). Both risk of bias assessment tools include several domains whereby in which regard each study is evaluated independently. The two reviewers completed the risk of bias assessments independently and any disagreement was resolved by discussion.
Statistical analysis
Due to the considerable differences regarding levels of evidence between the RCTs and cohort studies, the results from the RCTs were evaluated independently and the results from cohort studies were pooled in a meta-analysis. The meta-analysis was calculated using the Mantel-Haenszel estimator. The primary outcome was tested according to the null hypothesis that there is no difference in the risk of leg wound complications. The fixed or random effect was utilized depending of the heterogeneity of the studies included in the meta-analysis using I2, i.e., if heterogeneity was small (I2 ≤ 50%) the fixed-effect model was used while the random-effects model was assumed in case of high heterogeneity (I2 > 50%). The effect size of the meta-analysis was reported in log risk ratio and presented as exponent values.
The statistical analysis was performed using Stata (StataCorp. 2019. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC).
Results
Description of included studies
Of 4514 papers screened in this systematic review, 36 papers underwent full-text assessment with final inclusion of five studies [6, 12, 20,21,22] (Fig. 1). Of the five included studies, two were RCTs [20, 21] and three were cohort studies [6, 12, 22], respectively. Studies were mainly excluded as the outcomes of interest were not reported.
Quality of the included studies
An overview of the methodological assessment of the included studies is displayed in Table 1. The Oxford Centre for Evidence Based Medicine tool was used to classify the quality of included studies [23]. Only one of the included studies used concealed allocation [21]. One of the randomized studies [20] did not provide information regarding the randomization protocol. None of the studies used blinding.
Baseline characteristics
Patient baseline characteristics are reported in Table 2. Apart from two studies, there was no statistically significant difference in baseline characteristics between the two groups. In Temizkan et al. [12], the mean age of patients and the rate of hypertension were higher in the unmapped group (p = 0.038). In the randomized study by Zarrepur et al. [21] there was a significantly higher number of diabetic patients in the mapped group (US) (p = 0.024).
Outcomes
All five studies reported occurrence of leg wound complications following harvest of the saphenous vein as an outcome. Details of the included studies is shown in Table 3. Outcome measures varied notably between the studies.
Harvest wound complications
Due to significant differences in the study designs and quality, we chose to assess the RCTs individually separating them from the non-RCTs, thus pooling the results from the three non-RCTs in a meta-analysis. In the meta-analysis, we found a statistically significant reduction in the risk of leg wound complications in the ultrasound group with a risk ratio of 0.32 (0.19–0.55) compared to the group without preoperative ultrasound mapping (Fig. 2). As the I2 value was very low, the fixed-effect model was assumed.
In Zarepur et al., each leg wound complication type was reported separately [21]. No statistically significant difference was found between the two groups regarding postoperative infection (p = 1.000), nor incidences of edema, hematoma, or deep vein thrombosis.
Luckraz et al. assessed the presence of postoperative leg wound complications by an ASEPSIS score (additional treatment, serous discharge, erythema, purulent exudates, separation of deep tissues, isolation of bacteria, stay as patient prolonged over 14 days) [20, 24]. The ASEPSIS score ranges from 0 to 70 with higher scores indicating higher probability of infection. There was a statistically non-significant higher mean ASEPSIS score of 25 in the group without ultrasound mapping compared to a mean score of 10 in ultrasound group (p = 0.08).
Leg incision
Only the study by Lopes et al. [22] reported the risk for bilateral leg incision. Six patients in the unmapped group (8.95%) required an additional incision, and this outcome did not occur in the mapped group (p = 0.0067). Furthermore, in the RCT by Luckraz et al. there was a significant reduction in the leg wound incision length in the mapped group (mean 16.8 vs 24.1 cm, p = 0.005) [20].
Harvest time
Aguirre et al. reported that the median harvest time was significantly shorter in the mapped group (25 min [19, 21,22,23,24,25,26,27,28,29,30] vs 40 min [30–50]; p = 0.001) [6]. Similarly, Luckraz et al. found a significantly shorter time for vein harvesting per length of vein graft for the mapped group (36 ± 13 min compared to 47 ± 17 min for the non-mapped group, p = 0.04) [20].
Discussion
This systematic review assessed the existing literature regarding the effects of preoperative ultrasound mapping of the LSV on harvest site infections in patients undergoing CABG. We screened 4514 studies with final inclusion of 5 studies; 2 RCTs and 3 non-RCTs. Furthermore, we assessed reporting regarding additional leg incisions, incision length, and harvesting times.
Our meta-analysis based on three non-RCTs indicated a significant reduction of postoperative leg wound complications following preoperative ultrasound mapping [6, 12, 22]. The two RCTs included were assessed independently, and neither showed effects of preoperative vein mapping on harvest site infections [20, 21]. One of the RCTs, Zarepur et al. reported wound complications separately, indeed a higher number of patients would be needed to find any statistically significant difference between the groups. Only two studies [6, 22] reported the mean BMI as a confounder, while the study by Luckraz et al. [20] reported a mean body surface area, which is an important factor correlated with leg wound healing and complications.
Furthermore, one study showed statistically significant reduction in incision lengths, one study showed reduced risk of additional incisions, and two studies showed significantly shorter harvesting times. However, these outcomes are highly dependent on the experience of the surgeon performing the procedure which was not specified in the studies. Moreover, these secondary outcomes were not reported consistently in all of the included studies.
Despite the above reservations regarding the findings of the present systematic review and meta-analysis, our findings indicate that preoperative vein mapping leads to a better preoperative qualitative assessment of the LSV thus possibly reducing harvest site infection, incision lengths, the need for additional incisions, and harvesting times as compared to blind leg incision.
Other aspects of significance not within the scope of this present study are the learning curve and interobserver variability of utilizing ultrasound mapping as well as the cost-benefit aspects. All of these factor should be considered and investigated into before we can encourage the routine use of preoperative ultrasound mapping of the LSV. None of the included studies mentioned the effects of preoperative ultrasound mapping of the LSV on long term graft patency or perioperative graft strategy. Furthermore, as endoscopic vein harvesting was not within the scope of this study, this technique is known to reduce the risk of leg wound complications [26,27,28,29,30]. However, endoscopic equipment increases the cost of surgery and has different impediments as compared to a conventional harvesting technique. Therefore, open vein harvesting is still a widely used technique and efforts to improve this approach are warranted.
The strength of this study is a large comprehensive literature search performed using multiple databases by two independent reviewers. Thereby, the potential risk of missing relevant studies was very low. The meta-analysis in this study is based on three observational studies only, which is a considerable limitation. Furthermore, the findings from the meta-analysis regarding reduced harvest site infections were not confirmed by the two RCT’s. All included studies were ranked as lower quality studies with poor methodical quality. Furthermore, the lack of blinding and concealment in the included studies might induce a type 1 error, as the investigators might possibly evaluate the wounds of the UL group more favourably. The lack of randomization could lead to both type 1 or type 2 errors, while we find it more plausible the UL sound assessment were used more frequently on indication leading to utilizing UL on patients with more complex anatomy, possibly leading to type 2 errors.
Conclusions
Postoperative wound complications are a major concern following coronary bypass surgery. This systematic review including a metanalysis showed that the existing evidence in this field is of low quality. However, the studies suggest that preoperative ultrasound mapping might be beneficial in terms of reducing wound complications and harvest times while preventing unnecessary leg incisions. Indeed, these findings encourage large-scale randomized prospective studies in this field.
Availability of data and materials
Not applicable
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CABG:
-
Coronary artery bypass graft surgery
- CAD:
-
Coronary artery disease
- DVT:
-
Deep vein thrombosis
- EVH:
-
Endoscopic vein harvesting technique
- H:
-
High risk of bias
- LSV:
-
Long saphenous vein
- L:
-
Low risk of bias
- NR:
-
Not reported
- OR:
-
Odds ratio
- PVD:
-
Peripheral vascular disease
- +W :
-
Presence of wound complications
- RCTs:
-
Randomized controlled trials
- RR:
-
Risk ratio
- US:
-
Ultrasonography
- +US:
-
Ultrasound mapped group
- U:
-
Unclear risk of bias
References
WHO, Cardiovascular Diseases. 2021; Available from: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
Neumann F-J et al (2018) 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 40(2):87–165
Doenst T et al (2019) PCI and CABG for treating stable coronary artery disease: JACC review topic of the week. J Am Coll Cardiol 73(8):964–976
Caliskan E et al (2020) Saphenous vein grafts in contemporary coronary artery bypass graft surgery. Nat Rev Cardiol 17(3):155–169
Velazquez EJ et al (2016) Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med 374(16):1511–1520
Aguirre V et al (2019) Surgeon’s focussed ultrasound examination of the long saphenous vein reduces surgical time and wound complications. Heart Lung Circ 28(11):1735–1739
Aldea GS et al (2016) The society of thoracic surgeons clinical practice guidelines on arterial conduits for coronary artery bypass grafting. Ann Thorac Surg 101(2):801–809
Garland R et al (2003) A retrospective audit of long-term lower limb complications following leg vein harvesting for coronary artery bypass grafting. Eur J Cardiothorac Surg 23(6):950–955
Swenne CL et al (2004) Surgical-site infections within 60 days of coronary artery by-pass graft surgery. J Hosp Infect 57(1):14–24
Athanasiou T et al (2003) Leg wound infection after coronary artery bypass grafting: a meta-analysis comparing minimally invasive versus conventional vein harvesting. Ann Thorac Surg 76(6):2141–2146
Allegranzi B et al (2016) New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 16(12):e276–e287
Temizkan V et al (2013) Comparison of conventional technique and ultrasonographic mapping in saphenous vein harvesting. Heart Surg Forum 16(5):E248–E251
Head HD, Brown MF (1995) Preoperative vein mapping for coronary artery bypass operation. Ann Thorac Surg 59(1):144–148
Lemmer JH Jr et al (1988) Preoperative saphenous vein mapping for coronary artery bypass. J Card Surg 3(3):237–240
Khan OA et al (2011) Towards evidence-based medicine in surgical practice: best BETs. Int J Surg 9(8):585–588
Broughton JD et al (2013) Could routine saphenous vein ultrasound mapping reduce leg wound complications in patients undergoing coronary artery bypass grafting? Interact Cardiovasc Thorac Surg 16(1):75–78
Shamseer L et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350:g7647
Higgins JPT et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Sterne JA et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Luckraz H et al (2008) Pre-operative long saphenous vein mapping predicts vein anatomy and quality leading to improved post-operative leg morbidity. Interact Cardiovasc Thorac Surg 7(2):188–191
Zarepur R et al (2016) Efficacy of preoperative color doppler sonography of lower extremity veins on postoperative outcomes in candidates of saphenectomy: a randomized clinical trial. Electron Physician 8(9):2855–2859
Lopes FC et al (2018) Use of doppler ultrasound for saphenous vein mapping to obtain grafts for coronary artery bypass grafting. Braz J Cardiovasc Surg 33(2):189–193
Jeremy Howick et al. “The 2011 Oxford CEBM Levels of Evidence (Introductory Document)”. Oxford Centre for Evidence-Based Medicine. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence. Accessed 1 June 2022.
Wilson APR et al (1986) A scoring method (asepsis) for postoperative wound infections for use in clinical trials of antibiotic prophylaxis. Lancet 327(8476):311–312
Paletta CE et al (2000) Major leg wound complications after saphenous vein harvest for coronary revascularization. Ann Thorac Surg 70(2):492–497
Ouzounian M et al (2010) Impact of endoscopic versus open saphenous vein harvest techniques on outcomes after coronary artery bypass grafting. Ann Thorac Surg 89(2):403–408
Allen K et al (2005) Endoscopic vascular harvest in coronary artery bypass grafting surgery: a consensus statement of the International Society of Minimally Invasive Cardiothoracic Surgery (ISMICS) 2005. Innovations (Phila) 1(2):51–60
Sastry P et al (2013) The influence of endoscopic vein harvesting on outcomes after coronary bypass grafting: a meta-analysis of 267,525 patients. Eur J Cardiothorac Surg 44(6):980–989
Williams JB et al (2012) Association between endoscopic vs open vein-graft harvesting and mortality, wound complications, and cardiovascular events in patients undergoing CABG surgery. JAMA 308(5):475–484
Oddershede L et al (2012) Economic evaluation of endoscopic versus open vein harvest for coronary artery bypass grafting. Ann Thorac Surg 93(4):1174–1180
Acknowledgements
None
Funding
The authors received no financial support for the research, authorship, or publication of the article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the analysis and interpretations of results, and to writing and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
All authors have agreed for publication of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Media, A.S., Rajendran, R., Kimose, H.H. et al. Effect of preoperative ultrasound mapping of the saphenous vein on leg wound complications after coronary artery bypass surgery: a systematic review. Cardiothorac Surg 30, 21 (2022). https://doi.org/10.1186/s43057-022-00080-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43057-022-00080-9