Abstract
Background
Cardiac gunshot wounds with bullet embolism (BE) into the pulmonary artery are rare. Most pulmonary BE follow injuries of peripheral veins without concomitant cardiac injury. Herein, we describe a case of cardiac gunshot injury in which the bullet migrated from right atrium through the inferior vena cava down to right internal iliac vein and back to the left pulmonary artery. Such bullet migration is too rare and unusual and to our knowledge not reported before.
Case presentation
On March 4, 2019, a man of 39 had a bullet injury during celebratory gunfire. He was clinically stable with entrance on right posterior chest but no exit. Chest CT scan showed a bullet in the right atrium. The next day, the bullet migrated to the right pelvis as shown by plain chest and pelvic radiographs. CT angiography 3 weeks afterwards displayed the bullet in the right internal iliac vein. Meanwhile, the patient was asymptomatic, thus discharged home. However, 3 months later, he was readmitted because of chest pain, dyspnea, and sweating. A repeat chest CT scan showed the bullet in the left lower lobe pulmonary artery. Hence, pulmonary BE was suspected and eventually a 0.36 bullet was removed via left thoracotomy.
Conclusions
This is a case of symptomatic venous BE with typical diagnostic criteria (a small low-velocity bullet with inlet but no exit located away from anticipated trajectory with migration proven by serial radiographs). Endovascular removal was preferred but was not available. BE of the heart is exceedingly rare. Hence, diagnosis requires a high degree of clinical awareness.
Similar content being viewed by others
Background
To understand the effects of a bullet injury on the body, a range of factors should be considered. Besides the diameter of the bullet and its velocity, entrance profile and path of the bullet inside the body are important as well as the biological characteristics of the injured organ. Most high velocity bullets enter and leave the body in a straight trajectory while low velocity bullets may divert through bones or soft tissues and remain lodged, or may yet penetrate vessels, cardiac walls [1], or bowel [2] and behave as bullet emboli (BE) [3].
The first instance of a traumatic projectile embolism was published by Thomas Davis in 1834, when he reported a case of a wooden fragment that embolized from the venous circulation to the right ventricle in a 10-year old boy [3,4,5]. Bullet embolus to the pulmonary artery was first reported by Moresten in 1903 (Moresten cited in [2]). Bullet embolism is a rare phenomenon in trauma [6], with only 300 cases published before 2011 [4]. A review of 7500 gunshot wounds during the Vietnam War demonstrated a 0.3% incidence of bullet embolism [5, 6]. In the Afghanistan and Iraq Wars, a 1.1% (4/346) incidence rate was reported. The true incidence in the civilian population is largely unknown. However, the rate may be higher given the prevalence of lower velocity weapons and lower kinetic energy [7].
Bullet emboli are either arterial (75%) or venous (20%). Very occasionally, BE may pass from veins to arteries (or vice versa) through a traumatic arteriovenous fistula (AVF) or an intra-cardiac communication [2, 4, 7]. Such (paradoxical) BE constituted 2.4% of emboli in Springer et al.’s review (Springer et al. cited in [4]) while they reached 5% in other reports [2, 7].The phrase “venous bullet emboli” refers to emboli to the right heart or pulmonary arteries [7].
Eighty percent of arterial BE produce early symptoms due to obstruction of distal arteries and hence require early endovascular or surgical removal. In regard to venous BE, 83% travel in the direction of venous blood flow into a bigger proximal vein, right heart, or pulmonary arteries while a minority (15%) are carried distally by gravity. Unlike arterial BE, symptoms of venous BE are usually late and confined to just one-third of cases. Consequently, treatment of venous BE has remained controversial [1, 4, 5].
Migration of bullets into the pulmonary artery is described most often with lesions of peripheral veins without concomitant cardiac involvement [8]. Gunshot wounds of the heart with migration of the bullet into the pulmonary artery are rare [2, 8]. Herein, we present a very rare case of bullet embolism from the right atrium (RA) to right internal iliac vein and back to right heart and left pulmonary artery in which the patient survived trans-thoracic extraction of the bullet from left lower pulmonary lobar artery. This work has been reported in line with the CARE criteria [9]. The management of bullet embolism in the literature is reviewed and discussed.
Case presentation
On March 4, 2019, a man of 39 received a low-velocity bullet injury. It was an accidental bullet falling from a height. After a CT scan of the chest revealing a bullet in RA and a moderate right-sided hemothorax, the patient was referred next day to our teaching hospital for further care.
Luckily, the patient on arrival to our hospital was clinically stable apart from mild shortness of breath (SOB) and slight hypotension. There was a 4-cm non-bleeding wound located in right 6th intercostal space 7-cm lateral to the spine. Air entry on right lower back was reduced. Heart sounds were muffled, abdomen was soft on palpation, and peripheral pulses were palpable. His vital signs were a Bp of 95/55 mmHg, pulse rate (PR) of 110 bpm, and O2 saturation (PSO2) of 91% that increased to 96% with O2 supplementation via a mask.
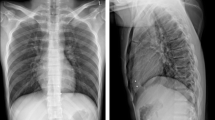
Unfortunately, neither the CT scan films nor reports were brought with him. Therefore, a chest X-ray (CXR) was ordered. The hemothorax was evident but no bullet was seen in the region of the chest. A chest tube was placed and drained 400 cc of blood (Fig. 1a). To our surprise, the bullet had descended to the right pelvis as shown by a plain pelvic film (Fig. 1b). When the initial CT scan of the chest (Fig. 1c, d) was reviewed later, the bullet was seen in RA along with mild pericardial effusion, and hence, a migrating bullet was our provisional diagnosis. Doppler ultrasonography revealed normal abdominal vessels and failed to locate the bullet. CT angiography was arranged (Fig. 1e) and showed the bullet outside the arterial tree but adjacent to iliac arteries (most likely inside the right internal iliac vein). Meanwhile, the chest drainage ceased and chest tube was removed after 5 days.
a Right-sided hemothorax drained by closed tube thoracostomy. b Bullet migrated to right pelvis. c, d First day CT scan of the chest showing a bullet in the right atrium with moderate right sided hemothorax. e CT angiography showing the bullet adjacent to iliac artery mostly in the right internal iliac vein
Although our patient had no evidence of arterial or venous occlusion, we advised him for surgical exploration to extract the bullet and save him from potential complications of a bullet migrating in the major abdominal veins. Unfortunately, the patient refused surgery and left the hospital despite our warnings.
The dramatic change occurred 3 months later when the patient was re-admitted due to sudden onset of SOB, chest pain, and sweating which gradually worsened. On examination, he had a rapid pulse but normal blood pressure. CT scan of the chest (Fig. 2a) revealed a new surprise! The bullet was seen in left pulmonary artery. An urgent left thoracotomy was done and a 0.36 in caliber bullet (Fig. 2b) was extracted from a basal branch of left pulmonary artery. The patient had an uneventful recovery and left the hospital 4 days after surgery. He was in a stable condition when seen 2 months later. The path of bullet migration is displayed by Fig. 3.
Discussion
A bullet embolism occurs when a small-caliber, usually low-velocity bullet, penetrates a single vessel wall and remains within the circulation [4, 5]. Nearly all of the cases in literature involve bullets 0.38 in caliber and smaller, with only one recorded case of a 0.40 in caliber bullet embolism [4]. In our case, the bullet caliber was equivalent to 0.36 in with an inlet but no exit. An inconsistent number of entry and exit wounds may be indicative of a retained bullet or projectile [4, 5]. Moreover, bullet embolism should be suspected when a bullet lies outside the established trajectory, or a wandering bullet is demonstrated on radiographs [5]. A whole body radiography ± CT scan are often needed to make the diagnosis while angiography is usually reserved for supplementary diagnosis or may be used as therapeutic endovascular extraction procedure [1].
Venous BE may be complicated by pulmonary embolism, cardiac valve dysfunction, endocarditis, abscess formation, venous thrombosis, dysrhythmias, intraventricular communications, tissue erosion, hemorrhage, and cardiac ischemia. It is of interest to note that such complications may not occur immediately after the initial injury but may develop months, years, and even decades later [1, 4, 5].
In the presence of symptoms, venous BE undoubtedly warrant removal preferably with endovascular techniques. It has been proposed that objects > 5 mm in diameter, irregularly shaped, freely mobile, or only partially embedded within the myocardium should be considered for extraction [4, 5]. Hartzler reported percutaneous transvenous removal of a bullet from the right ventricle in 1980 (Hartzler cited in [4]). Six years later, Ruff et al. reported the removal of a bullet from the hepatic vein with a retrieval basket [3]. Currently, the endovascular techniques are increasingly employed for retrieval of venous, intracardiac, and pulmonary BE due to their increased success rates and safety [4, 5].
The situation is quite different when venous BE are asymptomatic. Existing evidence suggests that there is no significant outcome difference between patients managed operatively versus non-operatively. Consequently, some authors recommend that retrieval of asymptomatic venous emboli should be considered only if an endovascular technique can be used, as the risks associated with invasive surgery may be too high to be considered on an elective basis [4].
Many authors reported cases of venous BE mostly managed by endovascular techniques [10,11,12,13] while others were managed by open surgery [14,15,16,17,18,19,20] or non-operatively [5, 21]. Open surgery was either used as a primary procedure or after failure of endovascular intervention. Likewise, non-operative approach was either chosen from the start or after failure of other techniques. The following are two patients’ stories depicting endovascular, non-operative, and operative treatments.
Yamanari et al. from Brazil reported the case of a man of 30 with a venous BE from the left external iliac vein to the lingular segment of the left pulmonary artery. Diagnosis was made with whole-body radiography and computed tomography. Two attempts to extract the bullet at time of pulmonary arteriography were unsuccessful, thus the patient was managed conservatively [1].
Hassan et al. reported the case of 23-year-old farmer who sustained a gunshot wound to his left upper chest secondary to a hunter’s errant shot. The projectile was impacted between cardiac apex and the diaphragm. The patient was treated conservatively and was discharged home but returned later on to the emergency department with chest pain. The projectile was then identified in the left inferior pulmonary vein. Operative management consisted of a median sternotomy, cardiopulmonary bypass, and a pulmonary venectomy [6].
In our country and many other countries with insufficient security, many people possess firearm weapons and may use them illegally contributing to an increase in civilian violence [22]. One common situation is shooting during social and national celebrations (celebratory gun fire) in which innocent persons may become injured or even killed. The case described herein was hit by a stray bullet falling from a height and therefore most likely it was of low velocity. “Bullets fired into the air usually fall back with terminal velocities much lower than their muzzle velocity when they leave the barrel of a firearm” [23].
The reported cases of pulmonary bullet embolism have mostly followed lesions of peripheral veins without concomitant cardiac involvement [8]. Cardiac gunshot wounds subsequently complicated by migration of bullets into the pulmonary arteries are reportedly rare [2, 8, 9]. Following trans-thoracic gunshot wound, the bullet in the index case penetrated the RA and made two migrations thereafter. First, it moved through the inferior vena cava (IVC) down to the right internal iliac vein. Such retrograde venous bullet migration is expected in the very large veins particularly in standing position and during coughing or a Valsalva maneuver [6]. Second, it returned back into the right heart to settle in the left lower pulmonary lobe artery. Such projectile pathway is very interesting and rare. We did not come through a similar case in the literature.
The patient was saved by surgical extraction of the bullet via left thoracotomy. However, one wonders what happened to the entrance wound of the bullet into the RA. Most likely this wound had sealed spontaneously after an initial bleed which produced the right hemothorax. The bullet could have caused an incomplete obstruction of the IVC or the iliac veins that is why there was no clinical evidence of venous occlusion.
Conclusions
We believe that radiographic confirmation of the location of an intravascular bullet is mandatory just prior to surgery as the bullet may suddenly change its location. The intraoperative use of fluoroscopy is also very helpful in such cases. Even without a Doppler ultrasonography, echo, and/or CT exam, if the plain radiographs show a change in position of bullet quickly from one body region to another, this should alert the physician to the possibility of intravascular bullet location.
Our case had the typical criteria of small-sized low-velocity bullet with inlet but no exit wounds and locations in body regions far from bullet trajectory. Due to symptoms and signs of pulmonary embolism, bullet extraction was indicated and was successfully accomplished by open surgery as our hospital lacked endovascular facilities. Two scenarios were involved in this case of pulmonary BE: a cardiac gunshot wound and migration of bullet through a peripheral vein.
Owing to their extreme rarity, no physician and no center had sufficient experience in management of intravascular migrating bullets. However, high clinical index along ancillary radiographic and imaging techniques may enable the physician in charge to make a timely diagnosis and initiate proper therapy.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- BE:
-
Bullet emboli
- Bp:
-
Blood pressure
- Bpm:
-
Beat per minute
- CXR:
-
Chest X-ray
- IVC:
-
Inferior vena cava
- PR:
-
Pulse rate
- PSO2 :
-
Oxygen saturation
- RA:
-
Right atrium
- SOB:
-
Shortness of breath
References
Yamanari MGI, Mansur MCD, Kay FU, Silverio PRB, Jayanthi SK, Funari MBG (2014) Bullet embolism of pulmonary artery: a case report. Radiol Bras 47(2):128–130
Bairagi A, Hardcastle TC, Muckart DJJ (2019) Left pulmonary artery bullet embolism following a penetrating cardiacgunshot injury.African. J Emerg Med 9:S61–S63
Ronsivalle J, Statler J, Venbrux AC, Arepally A (2005) Intravascular bullet migration: a report of two cases. Mil Med 170(12):1044–1047
Wojda TR, Dingley SD, Wolfe S, Terzian WT, Thomas PG, Vazquez D, Sweeney J, Stawicki SP (2017) Foreign intravascular object embolization and migration: bullets, catheters, wires, stents, filters and more. In: Embolic diseases: unusual therapies and challenges. IntechOpen
Fernandez-Ranvier GG, Mehta P, Zaid U, Singh K, Barry M, Mahmoud A (2013) Pulmonary artery bullet embolism—case report and review. Int J Surg Case Rep 4:521–523
Hassan AM, Cooley RS, Papadimos TJ, Fath JJ, Schwann TA, Elsamaloty H (2009) Pulmonary bullet embolism-a safe treatment strategy of a potentially fatal injury: a case report. Patient Saf Surg 3:12
Yoon B, Grasso S, Hofmann LJ (2018) Management of Bullet Emboli to the heart and great vessels. Mil Med 183:e307–e313
Imbert P-Y, Goin G, Goudard Y, De La Villeon B, Bonnet PM, Sockeel P, Pauleau G (2016) Pulmonary artery bullet embolism following cardiac gunshot wound. Ann Vasc Surg 36:290.e11–290.e14
Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler A, Orgill DP, For the SCARE Group (2018) The SCARE 2018 statement: updating consensus surgical case REport (SCARE) guidelines. Int J Surg 60:132–136
Schroeder ME, Pryor HI, Chunk AK, Rahbar R, Arora S, Vasiri K (2011) Retrograde migration and endovascular retrieval of a venous bullet embolus. J Vasc Surg 53(4):1113–1115
Nolan T, Phan H, Hardy AH, Khanna P, Dong P (2012) Bullet embolization: multidisciplinary approach by interventional radiology and surgery. Semin InterventRadiol 29(03):192–196 New York: Thieme Medical Publishers
Miller KR, Benns MV, Sciarretta JD, Harbrecht BG, Ross CB, Franklin GA, Smith JW (2011) The evolving management of venous bullet emboli: a case series and literature review. Injury 42(5):441–446
Carter CO, Havens JM, Robinson WP, Menard MT, Gates JD (2012) Venous bullet embolism and subsequent endovascular retrieval—a case report and review of the literature. Int J Surg Case Rep 3(12):581–583
Yordanov Y, Pateron D, May A (2014) An unusual aetiology of abdominal pain: the forgotten bullet. BMJ Case Rep. https://doi.org/10.1136/bcr-2014-208268
Stallings LA, Newell MA, Toschlog EA, Thomas CC, Kypson AP (2013) Right ventricular bullet embolism: diagnostic and therapeutic decisions. Injury Extra 44(7):64–66
Pan GZ, Bastidas JG, Hasaniya NW, Floridia R Jr (2013) Bullet embolization from an aorto-caval fistula to the heart. Interact Cardiovasc Thorac Surg 16(5):710–711
Padula RT, Sandler SC, Camishion R (1969) Delayed bullet embolization to the heart following abdominal gunshot wound. Ann Surg 169(4):599
Manganas C, Iliopoulos J, Pang L, Grant PW (2003) Traumatic pulmonary arteriovenous malformation presenting with massive hemoptysis 30 years after penetrating chest injury. Ann Thorac Surg 76(3):942–944
Lu K, Sanjay G, Qureshi MA, Wright AS, Kantathut N, Noeller TP (2015) Approach to management of intravascular missile emboli: review of the literature and case report. Western J Emerg Med 16(4):489
Koirala B, Shrestha KR, Thapa B, Sayami P (2012) Migration of a piece of shrapnel: femoral vein to superior vena cava-azygous junction. Eur J Cardiothorac Surg 42(3):584–586
Duke E, Peterson AA, Erly WK (2014) Migrating bullet: a case of a bullet embolism to the pulmonary artery with secondary pulmonary infarction after gunshot wound to the left globe. J Emerg Trauma Shock 7(1):38–40
Taha AY (2005) Emergency thoracotomy for cardiac or great vessel injuries: a report of 5 cases. Basrah J Surg 11(1):100–109. https://doi.org/10.33762/bsurg.2005.55425
Celebratory Gunfire. In: Wikipedia. Available from https://en.wikipedia.org/wiki/Celebratory_gunfire. Accessed 15 Aug 2019.
Acknowledgments
We wish to thank Dr. Aram Baram (Assistant professor and consultant cardiothoracic and vascular surgeon) for providing surgical backup during surgery on this case. Our thanks are also extended to Dr. Rebaz J Abdul (consultant radiologist) for reviewing the images and Dr. Havana H Nadr for drawing Fig. 3.
Funding
None.
Author information
Authors and Affiliations
Contributions
BDA and OYN collected the relevant patient data and wrote part of the manuscript draft. TAY reviewed the case, wrote the final manuscript, and reviewed the literature. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval has been obtained from the Ethical Committee of the hospital. Patient’s consent to participate in the study was obtained.
Consent for publication
Written consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bakir, D.A., Othman, Y.N. & Taha, A.Y. Pulmonary bullet embolism following cardiac gunshot wound: case report of a bullet that traversed the heart twice. Cardiothorac Surg 28, 5 (2020). https://doi.org/10.1186/s43057-020-0017-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43057-020-0017-5