Abstract
Background
Liver injuries such as metabolic-associated fatty liver disease, liver fibrosis, and steatosis are common in COVID-19 patients. Unenhanced CT can be used to diagnose the morphological traits of steatosis and cirrhosis. This study aims to provide a clear overview on the association between liver injuries and decreased hepatic CT attenuation values on chest CT images in patients with COVID-19.
Main text
Measuring HU values can be used as an additional method to diagnose liver injuries, even though HU values alone cannot definitively diagnose specific liver diseases. Chest CT is a common imaging procedure for diagnosing pneumonia, and during this CT examination, the upper abdomen, including the liver and spleen, is incidentally captured on the CT scan. Therefore, the assessment of liver injuries in chest CT of patients with COVID-19 can be performed by measuring the HU value of the liver and spleen. In this review, we summarize all the currently available CT findings in liver injuries associated with decreased hepatic CT attenuation values.
Conclusion
We found out that liver injuries such as hepatic steatosis and metabolic disease were more frequent in the COVID-19 patient, especially in severe and ICU patients. Compared to control group and COVID-19 patients with mild symptoms, the hepatic CT attenuation values and L/S ratios were lower in research group and severe COVID-19 patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
While the lungs are the primary target of COVID-19, the liver is also commonly affected [1]. Examination of liver tissue from COVID-19 patients reveals several abnormalities: congestion in blood vessels, breakdown of liver cells with areas of cell death, immune cell migration within the liver, and a moderate amount of fat accumulation within liver cells [2]. Several biological processes contribute to the development of liver complications following SARS-CoV-2 infection. These include hypoxia and circulatory changes, hepatotoxic drugs consumption, cytopathic effect via angiotensin-converting enzyme 2 (ACE2) receptors, and hyper-inflammatory reaction to COVID-19 [3]. The most frequent liver abnormality seen in COVID-19 patients is fatty liver, medically known as hepatic steatosis [4]. Furthermore, existing conditions such as metabolic-associated fatty liver disease (MAFLD) and liver fibrosis may worsen the inflammatory response in these patients [5].
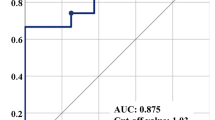
C-reactive protein (CRP) and D-dimer are well-established markers for predicting the severity of illness in COVID-19 patients. Scoring systems such as FIB-4 and APRI utilize readily available blood tests to assess liver fibrosis without needing invasive procedures [6]. Recent research suggests that among these markers (D-dimer, CRP, APRI, and FIB-4), the FIB-4 index appears to be the most accurate predictor for requiring mechanical ventilation (IMV). D-dimer and CRP have also shown some predictive value in this context. Furthermore, for predicting mortality, the FIB-4 index has shown the highest level of reliability, followed by D-dimer. This study proposes that using a FIB-4 threshold of greater than or equal to 1.9 might be more effective than traditional markers such as CRP and D-dimer in anticipating the need for mechanical ventilation and mortality risk in patients with SARS-CoV-2 infection [7].
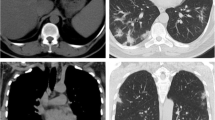
Ultrasound (US), computed tomography (CT), and magnetic resonance imaging (MRI) are established imaging modalities for liver evaluation [8]. US should be prioritized as the primary diagnostic modality for the initial assessment of the liver in patients presenting with abdominal symptoms. US is a popular tool for identifying fatty liver disease, especially in advanced cases. While it is good at distinguishing healthy livers from severely fatty ones (around 85% accurate), detecting moderate levels of fat (around 60% accurate) proves more challenging [9, 10]. Studies show that liver abnormalities are often seen on CT scans of COVID-19 patients [11, 12]. The most common finding is a decrease in liver density (26%), especially in severe cases (59%). Interestingly, measuring this density using CT scans—quantified liver/spleen attenuation—might help predict a patient’s outcome. An advantage is that since the liver is often included in routine chest CT scans for COVID-19, this information can be readily available without additional tests [13]. Also, MRI is recommended for elucidating liver abnormalities in COVID-infected patients where findings on US and CT are inconclusive [14].
In everyday clinical practice, CT scans are the most common way to image the liver. This is because they are widely available, provide detailed pictures with fast image capture, and offer the advantage of standardized analysis based on size and density measurements. Additionally, their excellent image quality makes them suitable for both routine and emergency situations [15]. Unenhanced CT, without contrast agents, is utilized to diagnose morphological traits of liver steatosis and cirrhosis. Additionally, for detecting nonspecific liver pathology, measuring Hounsfield Units (HU) values can serve as an additional method to diagnose liver injuries. HU values represent the X-ray attenuation properties of a material relative to water (0 HU) and air (− 1000 HU), obtained through a linear transformation of the measured attenuation coefficient. Normally, the liver parenchyma is homogeneous, with typical liver attenuation ranging from 50 to 60 Hus [16].
Liver density is assessed using a tube voltage of 120 kVp by calculating the average Hounsfield Units within a 1.5 cm2 circular region of interest (ROI) in four distinct regions spanning both lobes, each delineated by the hepatic veins. Spleen density, on the other hand, is derived from a 1.5 cm2 ROI positioned within the parenchyma. The regions of interest (ROIs) are strategically placed in both cases to steer clear of high-density zones (like calcifications) or low-density regions caused by vascular structures, cysts, or vessel entry points at the hila. Subsequently, the liver-to-spleen ratio (CT L/S) is computed, and steatosis is identified if the CT L/S index is equal to or less than 0.9 [17]. Assessment of hepatic steatosis (HS) through non-enhanced phase CT reveals that an ROI measurement in the right hepatic lobe below 40 HU indicates moderate hepatic steatosis with a liver fat percentage exceeding 30% [18, 19].
Chest CT is a common imaging procedure for diagnosing pneumonia and plays a crucial role in classifying COVID-19 pneumonia [20]. During CT examinations of patients with COVID-19, the upper abdomen, including the liver and spleen, is routinely visualized in the scans [21]. Therefore, evaluating liver abnormalities in the chest CT scans of COVID-19 patients can be achieved by measuring the Hounsfield Units values of the liver and spleen. This study aims to offer a comprehensive review of the CT findings related to liver injury caused by COVID-19 as reported thus far. The review specifically focuses on studies that investigated liver injury associated with changes hepatic CT attenuation values.
Methodology
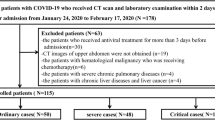
Medline was searched for “SARS-CoV-2 [MESH]” and “COVID-19 [MESH]” and “computed tomography [MESH]” and “liver injury [MESH]” and “liver steatosis [MESH],” to retrieve papers that published on liver injuries related to COVID-19 in chest CT. Published papers in PubMed, ScienceDirect, and Web of Sciences were used to search for original articles, reviews, and case reports in English between 2019 and March 2024. References of the articles were screened for other papers and included in this review when considered relevant.
The inclusion criteria for this paper were published papers about examining liver injury associated with COVID-19 by CT scan 9. However, the exclusion criteria conducted by eliminating articles were ones which examined liver disorders, according to the severity of COVID-19 and its relationship with biochemical abnormalities and liver disorders caused by drug consumption. Additionally, diabetes was included in the exclusion criteria since it contributes to fatty liver, which could confound the assessment of COVID-19-related liver injury. Finally, the articles were classified based on the findings of chest CT scan imaging.
Main text
This review included nine retrospective cohort studies (Table 1). Out of the 12 studies, five divided patients into a research group (positive COVID-19) and a control group (negative COVID-19) [22,23,24,25,26]. It should be noted that the research group in the Shumskaya et al. study was divided into three groups based on the severity of COVID-19 [26]. In other studies, patients were classified into two or three groups based on severity of symptoms in patients with COVID-19. These classifications included none severe group (NSG), severe group (SG) [27,28,29], ICU froup (IG), none ICU group (NIG) [30], fatty liver group (FL), non-fatty liver group (NFL) [31], positive oxygen demand OD (+), negative oxygen demand OD (−) [32], non-prognosis group (NPG), and prognosis group (PG) [33]. The most common clinical symptoms in mentioned studies included diarrhea, anorexia, abdominal pain, nausea, and vomiting.
In the study groups that compared hepatic CT attenuation in control and research groups, four of them determined that the Hounsfield Units of patients in the research groups significantly decreased compared to those in the control group [22,23,24, 26], while, the results of the Radzina et al. [25] study were the opposite, showing an increase in HU in the livers of patients in the research group. Uchida et al. study [27] evaluated hepatic attenuation values in both severe and non-severe patients with COVID-19. This study found that lower liver density readings (CT attenuation values) and a lower liver-to-spleen density ratio were linked to how severe a patient’s COVID-19 was upon admission to the hospital. However, the investigation by Chen et al. [28] failed to achieve analogous outcomes with Uchida et al., as they found no significant statistical difference in hepatic CT attenuation values and L/S ratios between severe and non-severe groups. Parlak et al. [30] divided patients with COVID-19 into an intensive care unit group (IG) and a none intensive care unit group (NIG). They found that liver density and L/S ratio were significantly lower in the IG. Additionally, the study by Fataftah et al. [31] revealed a significant decrease in hepatic CT attenuation values in fatty liver group compared to the non-fatty liver group at the time of admission.
Additionally, Nakayasu et al. assessed the risk factors associated with predicting oxygen demand in patients with COVID-19. The study involved a comprehensive evaluation of variables such as age, sex, existing health conditions, laboratory outcomes, and CT scan results, encompassing hepatic attenuation value and visceral fat. Its primary objective was to pinpoint particular factors capable of forecasting the requirement for oxygen assistance in individuals with COVID-19. While the link between liver-to-spleen size ratio and oxygen needs is not fully established, a lower L/S ratio is a reliable indicator of fatty liver disease [32]. Guler et al. [33] examined alterations in the L/S ratio throughout the progression of the COVID-19. They established a correlation between the L/S ratio and various factors, including clinical manifestations, laboratory results, and lung CT scores. While the progressive group had a slightly lower liver-to-spleen ratio (L/S) compared to the non-progressive group upon admission, this difference was not statistically significant (p-value = 0.547). Interestingly, at follow-up, the L/S ratio showed a significant difference between the two groups (p-value = 0.009).
Discussion
Generally, a CT scan is used to evaluate the severity of pneumonia and can also calculate Hounsfield Units of different tissues. Using the CT attenuation L/S ratio, obtained by the formula of mean hepatic CT attenuation divided by mean splenic CT attenuation value, can be a suitable factor for evaluating liver injuries such as hepatic steatosis and parenchymal injuries in patients with COVID-19. However, the visual representation of alterations in liver parenchyma on imaging remains uncertain. While variations in hepatic attenuation can be detected in certain diffuse liver conditions, the L/S ratio is frequently employed to evaluate the presence of liver fat [34,35,36]. In our study, the findings of hepatic CT attenuation and CT attenuation L/S ratio in COVID-19 patients were collected and analyzed. The study revealed that in most investigations evaluating the Hounsfield Units of the liver in patients with COVID-19, hepatic HU values significantly decreased. Moreover, the reduction in hepatic CT values was more pronounced in patients with severe symptoms hospitalized in the ICU compared to those with mild-to-moderate symptoms and non-ICU patients.
COVID-19, caused by the SARS-CoV-2 virus, can disrupt how the body manages fat, particularly in severely ill patients. Research suggests that people with severe COVID-19 are four to six times more likely to have a MAFLD compared to those without the disease. This suggests a significant impact of COVID-19 on metabolic dysfunction and liver health, especially in severe cases [37]. Therefore, the values of hepatic CT attenuation and CT attenuation L/S ratio in these patients are lower than in patients with mild-to-moderate COVID-19. Lower liver density (measured by CT scan) and a smaller liver-to-spleen size ratio (L/S ratio) might be indicators of how severe COVID-19 is in a patient.
However, the evidence of two studies were completely contradictory. The study by Radzina et al. showed a significant increasing of hepatic HU values in research group, which could be due to the incomplete patients screening at the time of admission and during the course of treatment [25]. In addition, the study conducted by Chen et al. found a weak relationship between the severity of COVID-19 and the hepatic CT attenuation values and CT attenuation L/S ratio. This weak relationship could be attributed to the unavailability of liver CT records for some patients before admission to the hospital or errors in attenuation measurement due to the low quality of images obtained from the low-dose scanning protocol [28].
Studies have shown a link between lower liver density and higher mortality rates in COVID-19 patients. Patients with liver HU ≤ 40 had nearly twice the mortality rate compared to those with HU > 40. The significant increase in HU observed in the fatty liver (FL) group may be attributed to liver parenchymal damage, such as fibrosis or a reduction in liver fat content, leading to the resolution of liver steatosis. Interestingly, this notable HU change is not exclusive to the FL group. In the NFL group, several patients initially had HU values within the normal range (40–60) upon admission. However, after 10–14 days of COVID-19 treatment, they exhibited substantial deviations from their baseline HU levels. The alteration in liver texture density in the NFL group could also be associated with fibrosis, decreased liver fat content, and the regression of steatosis [31]. Among patient in this study, approximately one-quarter exhibited abnormal liver enzymes. Interestingly, no significant changes were observed in liver enzyme levels during hospitalization for either the FL or NFL group. This suggests that the alteration in liver parenchyma, as measured by Hounsfield Units, is unlikely to be solely attributed to liver injury or fibrosis. Notably, a study by Wu et al. found that common liver function tests, including measurements of enzymes, bilirubin, and protein levels, did not directly correlate with the severity of COVID-19 cases. Importantly, liver damage in patients with mild COVID-19 is typically temporary and often resolves without specific treatment [38, 39].
Several studies have investigated the effects of COVID-19 on liver injuries, but they were excluded from our analysis. Crisan et al. [40] examined blood tests and MAFLD in COVID-19 survivors and non-survivors. They found no significant link between fatty liver disease (liver steatosis) and either the severity (p = 0.61) or survival rate (p = 0.56) of COVID-19 patients. Guo et al. [41] evaluated the occurrence of low liver CT density in COVID-19 patients and revealed that it is more common in these patients. Their results also showed that liver injury strongly correlates with the patient’s sex, COVID-19 severity, and low liver CT density. There are a few studies that have investigated chest CT findings in COVID-19 patients, these investigations have not explained liver CT attenuation but have reported blood test and abdominal CT findings in COVID-19 patients [42,43,44].
Identification specific factors that could predict the need for oxygen support in COVID-19 patients revealed that the L/S ratio, lymphocyte count, D-dimer levels, and abdominal circumference could serve as predictive indicators for the onset of oxygen requirement. Hence, focusing on the L/S ratio along with laboratory tests and underlying conditions may aid in identifying patients with more severe disease more accurately. Patients with advancing lung CT scores demonstrated notably increased CRP levels during follow-up [32]. Studies suggest a positive correlation between elevated CRP levels and both lung involvement and disease severity [45].
To summarize, liver dysfunction linked to decreased hepatic CT attenuation values was found to be associated with disease severity in COVID-19 patients. Recognizing these connections can offer critical insights for effectively managing patients throughout the course of the illness. Studies have shown that liver hypoattenuation, characterized by reduced liver-to-spleen CT attenuation ratios, is more prevalent in severe cases of COVID-19. Radiological features of COVID-19-induced hepatitis include hepatomegaly, altered liver echogenicity on ultrasound, and hypoattenuation on CT scans. Imaging modalities like CT scans plays crucial roles in evaluating liver damage in COVID-19 patients.
This review acknowledges several limitations. Firstly, the small number of patients in some studies may have led to biased results. Secondly, most studies assessed CT images upon admission, but the reports showed changes in hepatic attenuation during the course of COVID-19 in patients. Thirdly, the absence of contrast-enhanced liver imaging is a limitation, as unenhanced chest CT scans were repeatedly used in COVID-19 cases, with a focus on examining alterations in the upper abdomen, specifically the L/S ratio.
Conclusions
The analysis of liver injuries in COVID-19 patients through hepatic CT attenuation values and CT attenuation L/S ratios reveals valuable insights into disease severity and liver health. The observed decrease in hepatic Hounsfield Units in severe cases, alongside the impact of COVID-19 on fat metabolism and the prevalence of MAFLD, underscores the intricate relationship between the virus and liver function. Despite conflicting findings in some studies, between reduced liver density and disease severity underscores the diagnostic utility of CT scans. Their ability to visualize the upper abdomen, encompassing the liver and spleen, offers a potential avenue for detecting liver damage in patients with COVID-19. The limitations of current research, such as sample sizes and imaging protocols, emphasize the need for further investigation to elucidate the role of liver imaging in COVID-19 management. Overall, understanding the implications of hepatic CT attenuation values in COVID-19 patients can aid in better patient care and treatment strategies during the course of the illness.
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
Tellez L, Mateos RMM (2020) COVID-19 and liver disease: an update. Gastroenterol Hepatol (English Edition) 43(8):472–480
Tabary M et al (2020) Pathologic features of COVID-19: a concise review. Pathol-Res Pract 216(9):153097
Daoudi NE et al (2023) Mechanisms and management options of liver injury in COVID-19. In: Chen J-T (ed) Bioactive compounds against SARS-CoV-2. CRC Press, Boca Raton, pp 172–179. https://doi.org/10.1201/9781003323884-13
Spogis J et al (2021) Sonographic findings in coronavirus disease-19 associated liver damage. PLoS ONE 16(2):e0244781
Campos-Murguía A et al (2021) Liver fibrosis in patients with metabolic associated fatty liver disease is a risk factor for adverse outcomes in COVID-19. Dig Liver Dis 53(5):525–533
Huang I et al (2020) C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis. Ther Adv Respir Dis 14:1753466620937175
Tapia-Calderón DK et al (2024) Hepatic injury biomarkers in COVID-19. Ann Hepatol 29:101459
Vernuccio F et al (2021) Advances in liver US, CT, and MRI: moving toward the future. Eur Radiol Exp 5(1):52
Ferraioli G, Monteiro LBS (2019) Ultrasound-based techniques for the diagnosis of liver steatosis. World J Gastroenterol 25(40):6053
Hernaez R et al (2011) Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology 54(3):1082–1090
Zeb I et al (2012) Computed tomography scans in the evaluation of fatty liver disease in a population based study: the multi-ethnic study of atherosclerosis. Acad Radiol 19(7):811–818
Boll DT, Merkle EM (2009) Diffuse liver disease: strategies for hepatic CT and MR imaging. Radiographics 29(6):1591–1614
Gul Y et al (2022) The relationship of liver and pancreas density with chest computed tomography score progression and laboratory findings in patients with COVID-19. J Comput Assist Tomogr 46(6):848–853
Ippolito D et al (2023) Liver involvement in patients with COVID-19 infection: a comprehensive overview of diagnostic imaging features. World J Gastroenterol 29(5):834
Szklaruk J, Bhosale P, Luersen G (2015) State-of-the-art cross-sectional liver imaging: beyond lesion detection and characterization. J Hepatocell Carcin. https://doi.org/10.2147/JHC.S85201
Tisch C et al (2019) Hounsfield unit values of liver pathologies in unenhanced post-mortem computed tomography. Int J Legal Med 133(6):1861–1867
Byun J et al (2019) CT indices for the diagnosis of hepatic steatosis using non-enhanced CT images: development and validation of diagnostic cut-off values in a large cohort with pathological reference standard. Eur Radiol 29(8):4427–4435
Wells MM et al (2016) Computed tomography measurement of hepatic steatosis: prevalence of hepatic steatosis in a Canadian population. Can J Gastroenterol Hepatol 2016:1–7
Lawrence DA, Oliva IB, Israel GM (2012) Detection of hepatic steatosis on contrast-enhanced CT images: diagnostic accuracy of identification of areas of presumed focal fatty sparing. Am J Roentgenol 199(1):44–47
Fang Y et al (2020) Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology 296(2):E115–E117. https://doi.org/10.1148/radiol.2020200432
Palomar-Lever A et al (2020) Hepatic steatosis as an independent risk factor for severe disease in patients with COVID-19: a computed tomography study. JGH Open 4(6):1102–1107
Ali A et al (2021) Hepatic steatosis: a risk factor for increased COVID-19 prevalence and severity—a computed tomography study. Egypt Liver J 11(1):1–9
Tahtabasi M et al (2021) Frequency of hepatic steatosis and its association with the pneumonia severity score on chest computed tomography in adult COVID-19 patients. World J Crit Care Med 10(3):47
Medeiros AK et al (2020) Higher frequency of hepatic steatosis at CT among COVID-19-positive patients. Abdom Radiol 45(9):2748–2754
Radzina M et al (2022) Post-COVID-19 liver injury: comprehensive imaging with multiparametric ultrasound. J Ultrasound Med 41(4):935–949
Shumskaya YF et al (2023) Influence of liver attenuation on the severity of course COVID-19: a retrospective cohort study. medRxiv p 2023.02.27.23286488
Uchida Y et al (2020) Significance of liver dysfunction associated with decreased hepatic CT attenuation values in Japanese patients with severe COVID-19. J Gastroenterol 55(11):1098–1106
Chen F et al (2021) Clinical features and risk factors of COVID-19-associated liver injury and function: a retrospective analysis of 830 cases. Ann Hepatol 21:100267
Lei P et al (2020) Liver injury in patients with COVID-19: clinical profiles, CT findings, the correlation of the severity with liver injury. Hep Intl 14(5):733–742
Parlak S et al (2021) The effect of hepatic steatosis on COVID-19 severity: chest computed tomography findings. Saudi J Gastroenterol Off J Saudi Gastroenterol Assoc 27(2):105
Fataftah JZ et al (2022) The effect of COVID 19 on liver parenchyma detected and measured by CT scan hounsfield units. J Res Med Sci Off J Isfahan Univ Med Sci 27:26
Nakayasu H et al (2023) The liver-to-spleen ratio is a risk factor predicting oxygen demand in COVID-19 patients. Infect Med 2(2):105–111
Guler E et al (2021) Correlation of liver-to-spleen ratio, lung CT scores, clinical, and laboratory findings of COVID-19 patients with two consecutive CT scans. Abdom Radiol 46:1543–1551
Kodama Y et al (2007) Comparison of CT methods for determining the fat content of the liver. Am J Roentgenol 188(5):1307–1312
Ma X et al (2009) Imaging-based quantification of hepatic fat: methods and clinical applications. Radiographics 29(5):1253–1277
Yasui S et al (2012) Importance of computed tomography imaging features for the diagnosis of autoimmune acute liver failure. Hepatol Res 42(1):42–50
Sharma P, Kumar A (2020) Metabolic dysfunction associated fatty liver disease increases risk of severe Covid-19. Diabetes Metab Syndr 14(5):825–827
Wu J et al (2020) Liver diseases in COVID-19: etiology, treatment and prognosis. World J Gastroenterol 26(19):2286
Garrido I, Liberal R, Macedo G (2020) COVID-19 and liver disease—what we know on 1st May 2020. Aliment Pharmacol Ther 52(2):267–275
Crisan D et al (2021) Liver injury and elevated FIB-4 define a high-risk group in patients with COVID-19. J Clin Med 11(1):153
Guo H et al (2020) Analysis of liver injury factors in 332 patients with COVID-19 in Shanghai, China. Aging (Albany NY) 12(19):18844
Tirumani SH et al (2021) Are asymptomatic gastrointestinal findings on imaging more common in COVID-19 infection? Study to determine frequency of abdominal findings of COVID-19 infection in patients with and without abdominal symptoms and in patients with chest-only CT scans. Abdom Radiol 46(6):2407–2414
Liemarto AK et al (2021) Liver abscess with necrosis in post COVID-19: a case report. Ann Med Surg 72:103107
Moctezuma-Velázquez P et al (2022) NAFLD determined by Dallas Steatosis Index is associated with poor outcomes in COVID-19 pneumonia: a cohort study. Internal Emerg Med pp 1–8
Wang L (2020) C-reactive protein levels in the early stage of COVID-19. Med Malad Infect 50(4):332–334
Acknowledgements
We would like to express our sincere gratitude to Dr. SMJ Mortazav and Dr. Lembit Sihver for their invaluable time and expertise in reviewing and providing feedback on our manuscript. Their insightful comments and suggestions significantly improved the clarity and strength of our work.
Transparency statement
We affirm that this manuscript presents an honest, accurate, and transparent account of the study being reported. No significant aspects of the study have been omitted. Any deviations from the planned study design or registered protocol, if applicable, have been clearly explained and justified.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
NA and HG have participated in data curation, methodology, investigation, collected resources, and writing—original draft. HG was involved in editing and performed supervision. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All authors have read and approved the final version of the manuscript and take complete responsibility for the integrity of the data and the accuracy of the data analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdi, N., Ghaznavi, H. CT attenuation values predict liver injury in COVID-19 patients. Egypt J Radiol Nucl Med 55, 154 (2024). https://doi.org/10.1186/s43055-024-01330-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01330-y