Abstract
Background
Bow Hunter syndrome (BHS) is a rare, but important cause of posterior circulation stroke. It is also known as Rotational vertebral artery syndrome and is caused by transient dynamic vertebro-basilar insufficiency on movement of the neck in the presence of certain soft tissue or bone anomalies in the cranio-vertebral region.
Case presentation
We present a case of Bow hunter syndrome in an 18-year-old adult male who presented with vomiting, occipital headache and loss of balance, with findings of posterior circulation stroke on imaging. Medical causes of young stroke, including vasculitis and clotting disorders were ruled out, following which a diagnostic conventional angiography and CT angiography was performed. The cause of vascular compromise in our case was the presence of vertebral anomalies, in particular, the presence of a partial ponticulus posticus with formation of an incomplete arcuate foramen. He was treated with cervical spine immobilisation and C1–C2 fixation. In addition, our patient had a single posterior inferior cerebellar artery (PICA) on the side of the dynamic insufficiency, which lead to bilateral cerebellar infarcts. Our case is unique because it demonstrates a combination of osseous and vascular developmental anomalies resulting in posterior circulation stroke.
Conclusions
Though uncommon, BHS should be considered in the list of differentials in otherwise unexplained cases of posterior circulation stroke. Conventional angiography with dynamic manoeuvres is the modality of choice for documenting the rotational vertebral artery occlusion.
Similar content being viewed by others
Background
Rotational transient vertebrobasilar insufficiency is a relatively rare cause of transient posterior circulation stroke. Many studies have put forward various causes for the same which include cervical spondylosis with osteophytes, compression by anterior scalene muscle, fibrous bands, specific positioning during surgery and vigorous physical activities. The most common of these include osteophytes and muscular compression by head rotation. Our case puts forward a rare cause of the rare entity, which is a unilateral partial ponticulus posticus forming an incomplete arcuate foramen. The case provides an insight on how normal variants like these can cause catastrophic events in an otherwise normal young individual.
Case presentation
An 18-year-old man presented with complaints of vomiting, occipital headache and swaying while walking. He also experienced loss of balance with an episode of fall. There was no significant past history or comorbidities including diabetes mellitus, hypertension or tuberculosis. The patient denied any addictions. No significant family history was elicited. On examination, he was conscious and oriented. He had normal power, tone and reflexes in all four limbs. Cerebellar signs viz. dysdiadochokinesia and past pointing were present. CSF analysis revealed no significant abnormality. ESR by Wintrobe method was 7 mm. He tested negative for ANA, Lupus anticoagulant and Anticardiolipin antibodies; Antithrombin and Protein C activity was within normal limits. 2D echocardiography was unrevealing.
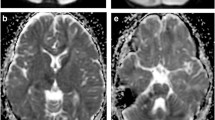
Plain CT brain showed hypodense areas in both cerebellar hemispheres. MRI brain with angiography was performed for further evaluation, which showed acute bilateral cerebellar infarcts (Fig. 1A). No supratentorial abnormality was seen. On angiography, a hypoplastic/stenotic left vertebral artery was present (Fig. 1B). A conventional four-vessel angiography was thence performed in neutral neck position as well as using dynamic manoeuvres involving movements of the neck. On rotation of the neck towards the right side, complete occlusion of a short segment of the distal left vertebral artery was observed (Fig. 2D). Right vertebral artery appeared normal, even on the dynamic acquisitions (Fig. 2C). Bilateral internal carotid artery and external carotid artery angiograms were normal (not shown).
Digital subtraction angiography images: In neutral positions (A and B), show normal contrast opacification of both vertebral arteries. On tilting the head towards the contralateral side (C and D), show complete abrupt occlusion of a focal short segment of the left vertebral artery (arrow in D) at the level of C1 vertebra
CT scan of the cervical spine with vertebral angiography was subsequently performed to ascertain the cause of the dynamic vertebral artery occlusion, which revealed multilevel vertebral segmentation anomalies (Fig. 3A). In addition, a partial ponticulus posticus was seen arising from the left arch of atlas (Figs. 3B and 4), leading to the formation of an incomplete arcuate foramen. A small accessory bony ossicle was also seen adjacent to the arcuate foramen (Figs. 3C and 4). These were seen encroaching upon the intervening left vertebral artery (Fig. 4). Additionally, note was made of a single left PICA (Fig. 4), with absent right PICA. Block vertebra at C2–C3 level was seen. All these anomalies in conjunction were the proposed cause of the dynamic vertebral artery occlusion/Bow Hunter syndrome.
Sagittal bone algorithm CT image of the cervical spine (A) shows block vertebra at C2–C3 and D1–D2 levels. Sagittal post-contrast CT images show: An accessory bony ossicle (arrow in C) with formation of an incomplete arcuate foramen due to a partial ponticulus posticus (arrow in B). Normal anatomy on the contralateral side (D)
Oblique coronal reformatted post-contrast post-processed (MIP) CT image shows a single posterior inferior cerebellar artery (PICA) arising from the vertebral artery on the left side (yellow arrow), with absent right PICA. An accessory bony ossicle (*) and an anterior bony spur (orange arrow) are seen encroaching upon the intervening left vertebral artery
The patient was treated with immobilisation and surgical cervical (C1–C2) fixation.
Discussion
The common causes of young posterior circulation stroke include cardioembolic disease, arterial dissection and vasculopathy. Bow hunter syndrome (BHS) is a rare condition which causes transient vertebro-basilar insufficiency due to dynamic motion of the neck. In this condition there is mechanical compression of the vertebral artery by any soft tissue or bone abnormalities at the posterior neck by rotation of the head to either side by more than 45 degrees. This is the reason for the condition being called rotational vertebral artery syndrome.
The hypothesis of the condition was first put forward by Tatlow and Bammer in 1957 who studied the same in cadavers of patients who had transient symptoms of vertebral artery insufficiency with head rotation [1]. It was found that the main causes were cervical osteophytes and enlarged anterior scalene muscle in their study with cadavers. In 1978, Sorensen coined the term Bow Hunter syndrome for this transient vertebral artery insufficiency after his study in a patient who suffered from Wallenberg syndrome following archery [2]. The mechanism of this reversible condition is explained with a “two hit” model. In the first hit, one of the vertebral arteries is severely hypoplastic or stenotic due to congenital or acquired cause. In the second hit, there is affection of the contralateral vertebral artery by a structural variation or anomaly like bony spurs, fibrous bands or disc herniation [3].
The most common cause of BHS has been found to be cervical vertebral osteophytes [4]. The most common site of occlusion is at the atlantoaxial joint due to the following reasons. The artery is relatively fixed and immobilised at the foramen transversarium at this joint which makes it more prone for occlusion with head rotation [5]. Another hypothesis is the apparent lengthening of the artery due to asymmetric movement of contralateral joint between C1-C2 with head rotation ultimately causing arterial occlusion [6]. There are many other factors leading to ischemic compromise of the hindbrain, of which isolated posterior circulation with no adequate collateral supply is a major cause. If the contralateral unaffected artery is abnormal due to stenosis, dissection and hypoplasia the condition is triggered with inadequate blood supply from the contralateral side.
Our patient presented with features of posterior circulation stroke and was found to have bilateral cerebellar infarcts. He had a single posterior inferior cerebellar artery arising from the affected left vertebral artery. This very much reveals the significance of arterial anomalies in determining the management and outcome in such individuals. The commonest of the anomalies include unilateral vertebral artery hypoplasia.
Imaging studies play a pivotal role in the diagnosis. The modalities that are of use are radiographs, computed tomography, magnetic resonance imaging and digital subtraction angiography. Of these dynamic digital subtraction angiography plays the most important role in diagnosis. The procedure while being performed the patient can be instructed head rotation which confirms the diagnosis and makes it the gold standard imaging technique for BHS [3].
The rarity in our case also includes the presence of a ponticulus posticus which is a bony bridge between the posterior superior articular process and posterolateral margin of posterior arch of atlas. There are three types of the same: complete, incomplete and calcified. Our patient had an incomplete type, which caused compression of the left vertebral artery near its foramen with head rotation. A similar case was presented by Charles. Simpkin et al., where there was a bone bridge at the lateral mass over left vertebral artery foramen and which connects to the posterior arch of atlas forming an arcuate foramen [7].
The treatment of BHS is decided according to the etiology. Surgical options include cervical fusion, cervical decompression and endovascular stents within the unaffected vertebral artery to maintain adequate posterior circulation [3]. Conservative management includes long term anticoagulation and hard cervical collars with prevention of head rotation [8].
Conclusions
It is important for all radiologists to have a thorough knowledge of normal anatomy in order to recognize developmental variants. BHS is one such rare, albeit important syndrome highlighting the importance of identifying such normal variants, posing as risk factors to posterior circulation stroke.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- BHS:
-
Bow hunter syndrome
- CT:
-
Computed tomography
- PICA:
-
Posterior inferior cerebellar artery
- CSF:
-
Cerebrospinal fluid
- ESR:
-
Erythrocyte sedimentation rate
- ANA:
-
Antinuclear antibody
References
TissingtonTatlow WF, Bammer HG (1957) Syndrome of vertebral artery compression. Neurology 7:331
Sorensen BF (1978) Bow Hunter’s stroke. Neurosurgery 2:259–261
Choi K-D, Choi J-H, Kim J-S, Kim HJ, Kim M-J, Lee T-H et al (2013) Rotational vertebral artery occlusion: mechanisms and long-term outcome. Stroke 44:1817–1824
Rastogi V, Rawls A, Moore O, Victorica B, Khan S, Saravanapavan P et al (2015) Rare etiology of bow hunter’s syndrome and systematic review of literature. J Vasc Interv Neurol 8:7
Netuka D, Beneš V, Mikulík R, Kuba R (2005) Symptomatic rotational occlusion of the vertebral artery: case report and review of the literature. Zentralbl Neurochir 66:217–222
Barton JW, Margolis MT (1975) Rotational obstruction of the vertebral artery at the atlantoaxial joint. Neuroradiology 9:117–120
Simpkin CT, Davis KE, Davis BS, Vosko AM, Jorgensen ME (2017) Bow hunter’s syndrome in a patient with vertebral artery atresia, an arcuate foramen, and unilateral deafness: a case report. Radiol Case Rep 12:597–601
Cornelius JF, George B, N’dri Oka D, Spiriev T, Steiger HJ, Hänggi D (2012) Bow-hunter’s syndrome caused by dynamic vertebral artery stenosis at the cranio-cervical junction—a management algorithm based on a systematic review and a clinical series. Neurosurg Rev 35:127–135
Acknowledgements
Not applicable.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
NG and RB analyzed and interpreted the cross-sectional images. AS was a major contributor in writing the manuscript. AG performed the conventional angiography. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The need for ethics approval was waived by the institution ethics committee. Name of the ethics committee -Institutional Ethics Committee, Department of Pharmacology, Grant Government Medical College and Sir J.J. Group of Hospitals, Mumbai-400008. IEC registration number-ECR/382/Inst/MH/2013/RR-19.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gupta, N.A., Subash, A., Bhalde, R.P. et al. Dynamic vertebral artery occlusion aka bow hunter syndrome causing posterior fossa stroke in a young adult: a case report. Egypt J Radiol Nucl Med 55, 92 (2024). https://doi.org/10.1186/s43055-024-01265-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01265-4