Abstract
Background
Breast cancer survivors who underwent breast conserving therapy (BCT) are still 10% more likely to develop a second breast cancer at follow-up, Digital mammography (DM) was advised in every practical guideline for follow-up after BCT; however, it was difficult to distinguish between actual recurrence and scar development at DM.
Our research objective is to assess the value of Digital Breast Tomosynthesis (DBT) on the final Breast Imaging Reporting and Data System lexicon (BI-RADS) assessment categories compared to diagnostic digital mammography (DM) of breast cancer patients treated with breast conservation therapy (BCT), and to determine the additive value of DBT to DM or the use of DBT with synthetic 2D images in the diagnostic workup following BCT.
Results
Four hundred and seventeen breast cancer patients who underwent breast-conserving therapy (BCT) and received diagnostic assessments, including digital mammography (DM), digital breast tomosynthesis (DBT), and reconstructed synthetic 2D images, were enrolled in the study.
There is a significant reduction in the proportion of studies classified as probably benign BI-RADS 3 in synthetic 2D + DBT and DM + DBT compared with those in DM alone, and this was demonstrated by the two readers and at double reading (all P = 0.01). There is a significant increase in the PPV of malignancy in synthetic 2D + DBT and DM + DBT compared with those in DM alone for reader 2 (P = 0.01) and at double reading (P < 0.04) without a significant difference in the proportion of studies classified as BI-RADS category 4 or 5 for both readers and at double reading (p > 0.3).
Regarding the mammographic abnormalities, we noted a significant reduction in asymmetry and a significant increase in architectural distortion in synthetic 2D + DBT and DM + DBT compared with those in DM alone, and this was demonstrated by the two readers and at double reading (all P = 0.01).
Conclusions
The addition of digital breast tomosynthesis (DBT) into the diagnostic process after breast-conserving therapy (BCT), either in conjunction with digital mammography (DM) or with synthetic 2D images in the diagnostic workup following BCT, significantly decreases the proportion of studies classified as probably benign, significantly increases the rate of studies classified as normal or benign, and significantly increase in the positive predictive value (PPV) of malignancy without significant difference in the patients classified as BI-RADS category 4 or 5. Moreover it improved diagnostic confidence in biopsy recommendations, regardless of mammographic density.
Similar content being viewed by others
Background
Breast cancer survivors who underwent breast conserving therapy (BCT) are still 10% more likely to develop a second breast cancer at follow-up appointments after five years. In the ipsilateral and contralateral breast, they can experience new primary or local recurrence [1, 2]. To enable early therapies that improve quality of life and survival, surveillance of these individuals attempts to find asymptomatic second breast tumors [3]. The use of cost-effective follow-up imaging is crucial since recurrence surveillance increases the workload on imaging centers [4].
Digital mammography (DM) was advised in every practical guideline for follow-up after BCT [5]; however, it was difficult to distinguish between actual recurrence and scar development at DM, and as a result, DM yield in the initial BCT months was poor [6]. Additionally, DM had considerably higher sensitivity in patients without a personal history of breast cancer (ranges between 73.5% and 76.5%) than matching postoperative breast screens (ranges between 63.5% and 67%) [7].
Digital breast tomosynthesis (DBT) has recently been added to DM or DBT with synthetic 2D mammograms have shown improved sensitivity and specificity in the identification of breast cancer with lower recall rates when compared to DM alone regarding the screening for the disease [8]. Additionally, DBT was more effective than DM in diagnostic contexts in terms of lesion conspicuity, location characterization that allows confidence in diagnosis [9, 10], which dramatically lowers recall rate and need less extra imaging [11], As a result, the American College of Radiology (ACR) advocated DBT using artificial two-dimensional (2D) pictures for the surveillance of breast cancer survivors [5].
With a high proportion of invasive tumors that appear as architectural distortion (AD), DBT decreased the additional investigations needed to distinguish between benign and malignant AD [12]. Intriguingly, DBT decreased recollection rates and enhanced cancer detection rates in women with breast cancer who had received treatment [13, 14]. DBT may therefore be helpful for breast cancer patients who have already had BCT [15].
To the best of our knowledge, no data are reported on the effect of applying DBT to DM in the diagnostic workup of breast cancer after BCT. The current study aimed to evaluate the effect of adding DBT to DM and DBT with synthetic 2D images in the diagnostic settings of breast cancer patients treated with BCT.
Methods
Patients selection
This prospective study was approved by our Institutional Review Board. Written informed consent was obtained from each patient after receiving information about the details of the study. From December 2016 to January 2020, a total of 417 breast cancer patients who underwent breast-conserving therapy (BCT) and received diagnostic assessments, including digital mammography (DM), digital breast tomosynthesis (DBT), and reconstructed synthetic 2D images, were enrolled in the study. Diagnostic evaluations were conducted in response to abnormalities detected during screening or short-interval follow-ups. Patients with palpable abnormalities were excluded, as the focus was on detecting abnormalities through screening before they became palpable by the patients. Additionally, patients with BI-RADS 0 classification were excluded from the statistical analysis. The average age of the patients was 56.1 ± 5.4 years, with a range from 27 to 69 years.
Mammographic techniques
A DM and DBT with synthetic 2D images were performed using (AMULET Innovality; FUJIFILM, Singapore). Mediolateral oblique (MLO) and craniocaudal (CC) projections were acquired in both DM and DBT images.
DBT images were acquired by the movement of the x-ray tube (over a 15° arc), and images were reconstructed (1-mm sections). From both CC and MLO views of the DBT, the synthetic 2D images were created by summation and filtration of reconstructed images. Additional ultrasound, or MRI were performed if considered necessary for further evaluation (according to the characteristics of the abnormality detected on the DM or DBT).
In the current study, 60 patients performed MRI (those who categorized as BIRADS IV and V by DBT and synthetic view + DM at double reading), 143 patients were recalled for US, and 272 patients those who categorized as BIRADS 1 and II by double readers we didn’t recall them for US.
Mammographic analysis
Four hundred- seventeen sets of DM, synthetic images, and DBT were reviewed by two radiologists with 11 and 12 years’ experience in breast imaging. Images were reviewed on the diagnostic workstation in two sessions by both readers, then double-read. In the first session a sequential review of synthetic 2D images with DBT (synthetic 2D + DBT), one month later in the second session, sequential review of DM images, and then with DBT (DM + DBT). In all images the comparison was performed between DM, synthetic 2D + DBT, and DM + DBT regarding the final evaluation of BIRADS category, and final BI-RAD categorization according to breast density classes, mammographically detected abnormalities (asymmetry, AD, mass, and microcalcification). Reviewers were blinded to the clinical examination but not to prior mammography including pre-surgical images if available.
Breast density was evaluated according to the ACR BI-RADS recommendations [16]. It was classified into four classes: a (entirely fatty), b (scattered fibroglandular tissue), c (heterogeneously dense), and d (extremely dense).
As said before, examinations of the BI-RADS 0 category were excluded from statistical analysis of BI-RADS assessment. Finally, 415 patients who underwent diagnostic examinations, including (DM, synthetic images, and DBT) with BI-RADS categories 1–5 were included.
Reference standard
The medical records were evaluated for outcomes. Histopathological evaluation (needle biopsy or surgical specimen) was the reference standard for BI-RADS category 4 or 5 patients, but in BIRADS 1, 2, and 3 follow up by imaging and clinically for at least 3 years was the reference standard.
Statistical analysis
Statistical analyses were performed by SPSS software (version 23.0, SPSS, Inc., Chicago, IL, USA). Comparisons between synthetic 2D + DBT, DM, and DM + DBT were performed according to the breast density, the type of mammographic abnormality, the final BI-RADS Category and the final outcome using the Chi-square test. Statistical significance was considered at a P-value < 0.05.
Results
Among 415 patients, 324 (78.1%) were diagnosed with invasive cancers, and 91 (21.9%) were diagnosed with carcinoma in situ. The time interval between BCT and diagnostic examinations was (mean 17.7 ± 8.2 months, range 8.3–22.1 months). Nineteen patients (4.6%) developed ipsilateral recurrence, and 31 patients (7.5%) developed contralateral cancer (Table 1).
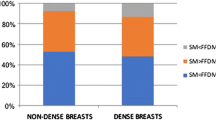
Final BI-RADS assessment categories were compared between DM, synthetic 2D + DBT, and DM + DBT (Table 2). There is a significant reduction in the proportion of studies classified as probably benign BI-RADS 3 in synthetic 2D + DBT and DM + DBT compared with those in DM alone, and this was demonstrated by the two readers and at double reading (all P = 0.01) (Figs. 1, 2). In concomitant with a significant increase in the proportion of studies classified as normal and benign (BI-RADS 1 and 2 respectively) in synthetic 2D + DBT and DM + DBT compared with those in DM alone regardless of breast density for both readers and at double reading (P = 0.03, 0.03 for reader 1, 0.01, 0.02 for reader 2 and 0.01 and 0.02 for double reading) (P < 0.03) (Fig. 3). There is a significant increase in the PPV of malignancy in synthetic 2D + DBT and DM + DBT compared with those in DM alone for reader 2 (P = 0.01) and at double reading (P < 0.04) without a significant difference in the proportion of studies classified as BI-RADS category 4 or 5 for both readers and at double reading (p > 0.3) (Fig. 4).
A 38-year- old female patient underwent breast conservative surgery. At DM MLO view a, synthetic 2D MLO view b, both readers demonstrated a focal asymmetry in right upper breast which is contiguous with the skin contour deformity. On diagnostic DBT c, this abnormality was resolved, and central lucency was clearly identified as post-surgical scar and assigned BIRAD category 2 by both readers. It remains stable on follow up
A 55-year- old female patient underwent breast conservative surgery. DM MLO view a, synthetic 2D MLO view b revealed focal asymmetry at the left upper breast. On diagnostic DBT c, central lucency was identified and a postoperative change at the site of scar was confirmed by ultrasound examination performed on the same day d. It regresses on size on follow up DBT e
A 46-year- old female patient underwent breast conservative surgery. Focal asymmetry at the left upper breast was described by both readers at DM MLO a, synthetic 2D MLO views b. On diagnostic DBT, MLO c, CC d, localized glandular tissue with linear fat strands were identified and assigned as BIRAD category 1 by both readers. Ultrasound correlative image e showed localized glandular tissue
A 40-year-old female patient underwent breast conservative surgery.DM CC View a, synthetic 2D CC view b revealed focal asymmetry at the outer half of the left breast. On diagnostic DBT, CC view c, revealed small speculated mass with irregular outline associated with architectural distortion and assigned as BIRADS 5 and confirmed by biopsy as recurrent IDC
On double reading of synthetic 2D + DBT, DM, and DM + DBT, there are no significant differences in the breast density at the final BI-RADS categorization (p > 0.07) (Table 3).
There was a significant increase in AD in synthetic 2D + DBT and DM + DBT compared with those in DM alone, and this was demonstrated by the two readers and at double reading (all P = 0.01) (Table 4).
Discussion
DM is considered the gold standard for detecting and diagnosing breast cancer [16]. But its flaw remains that overlapping of normal breast tissue can result in false-positive tests and pointless patient recalls [17]. DBT has solved the superimposition of breast tissue and reduced tissue overlapping by permitting consecutive slices through the breast tissue [18, 19].
From our study, we noted that the addition of DBT to either DM or synthetic 2D + DBT images significantly decreased the number of cases classified as BI-RADS 3, and this was demonstrated by the two readers and at double reading (all P = 0.01), increase the number of cases classified as normal or benign (BI-RADS 1, 2 respectively) compared with DM alone in the diagnostic settings of breast cancer following BCT for both readers and at double reading (P < 0.03), regardless of the patient’s mammographic density. This was also noted by Mumin et al. [20], that synthetic View images when reviewed with DBT are superior to DM in lesion detection, and characterization [20]. Moreover, the radiation dose was substantially reduced by 52%, which could provide evidence that synthetic view combined with DBT is acceptable to be used in routine clinical practice and may obviate the need for DM [20].
Two trials [18, 19] have shown that the DBT improved the visibility of lesions and reduced the requirement for unnecessary benign biopsies or further imaging for false-positive outcomes. Our postoperative data showed the same results, with a decline in BIRADS 3 and a commensurate raise in BIRADS 1 and 2. Additionally, as compared to DM alone, our findings show that DBT can reduce the short-term interval follow-up of benign postoperative alteration by 55.2%. This demonstrates DBT's ability to reduce tissue overlapping and get rid of breast tissue superimposition [21]. Also, DBT reduced the recall rate in 451 breast cancer patients by 29%, according to Sia et al. [22].
In this current study, the addition of DBT to DM or synthetic 2D + DBT improves the PPV of malignancy compared to DM alone without significantly changing the number of patients referred for biopsy in BI-RADS category 4 or 5. Additionally, there was no discernible difference between DM + DBT and synthetic 2D + DBT in terms of the PPV of malignancy and final BI-RADS classification. As a result, synthetic 2D + DBT can substitute DM alone or DM + DBT in the surveillance of patients with BCT, as it also lowers the degree of exposure. DBT proved to be useful in the diagnostic scenario for postoperative breast cancer patients.
Our findings showed that the addition of DBT to DM or synthetic 2D + DBT lowered the false-positive rate associated with breast biopsies, which was in line with earlier researches conducted in screening environments as in Lourenco et al. [23], Mayo H. Fujii et al. [24], and Bahl M. et al. [25], which concluded that the addition of DBT increased the detection rate of histologically favorable tumors compared with that attained with DM screening.
In contrast to Friedewald SM et al. [26], McCarthy AM et al. [27] and Greenberg JS et al. [28], who claimed that DBT had higher rates of cancer diagnosis than DM alone, a high cancer detection rate on DM exams in diagnostic settings like those in our study could account for the similar cancer detection rates at DM and DBT. A significant cancer detection rate was reported on DM and was not improved by DBT, which is consistent with prior studies Mayo H. Fujii et al. [24], and Bahl et al. [25].Uncertainty exists regarding the effects of higher cancer detection rates on death rates and interval breast cancer rates [29]. In contrast to DM, postoperative breast alterations (such as AD or asymmetry) may compromise the quality of synthetic 2D pictures. Fortunately, adding DBT can help overcome it. Additionally, in our investigation, there was no discernible difference between synthetic 2D + DBT and DM + DBT in terms of the PPV of malignancy or final BI-RADS classification. DBT was therefore helpful in the diagnostic situation for patients with postoperative breast cancer. In the monitoring of patients with BCT, synthetic 2D + DBT can take the role of DM alone or DM + DBT.
The accuracy of DBT differs according to the type of postoperative mammographic abnormality [21]. Mass presentation on DM results in higher true-positive findings with DBT, while asymmetry presentation leads to fewer false positives on DM + DBT [17]. This results are concomitant with our results in that DM + DBT or synthetic 2D + DBT significantly lowers the false positive rate of asymmetry than DM alone by both readers and at double reading as better margin analysis by DBT boosts the observer’s confidence in lesion interpretation and reduction of unnecessary biopsies, contrary to the previous results, our results show no significant difference in mass detection between DM, DM + DBT, or synthetic 2D + DBT by both readers and at double reading. This could be explained by the large size of the mass in our study (18.4 ± 7.1) which could be easily detected by any modality.
According to Murphy et al. [30], synthetic 2D + DBT has a significant advantage in the assessment of AD, all patients recalled for AD were more worried about malignancy on synthetic 2D + DBT than on DM alone. According to the results of our study, which showed that the synthetic 2D + DBT and DM + DBT significantly had better assessments of AD than DM alone by both readers and at double reading, the malignant features associated with AD (radiating thin straight lines, spiculation, focal retraction or distortion of breast parenchyma, blurring of normal tissue planes, or compression of tissue around a mass) are better appreciated at additional tomographic images [30].
Although the DBT is more effective than the DM at assessing asymmetry and AD, its significance in evaluating calcifications is still unclear [21]. However, because DBT is better at visualizing the distribution of microcalcifications, its integration with DM reduced recalls for calcifications [31]. This finding is consistent with our findings, which showed that there was no significant difference in the assessment of calcification between DM, synthetic 2D + DBT, or DM + DBT by either reader or at double reading. However, lower sensitivity may be a problem because of poor visibility and decreased spatial resolution acquired from multiple images.
The advantages of DBT go beyond the usefulness already recognized for screening situations, to sum up. In the diagnostic settings of postoperative patients, DBT enhances the BI-RADS final assessment categories with a notable increase in the rate of BI-RADS 1 and 2 categories. increases the diagnostic confidence in biopsy recommendations while reducing the number of BI-RADS 3 categories. DBT can therefore be added to improve treatment outcomes (including lower costs and reduced patient anxiety) by increasing the sensitivity and specificity of DM.
The limitation of our study included the potential impact of the time interval between BCT and the diagnostic examinations on the BI-RADS assessment categories. In our investigation, the time interval averaged 13.7 ± 4.2 months, with a range of 8.3 to 20.1 months. This variation in time intervals may contribute to differences in results when compared to other studies.
Conclusions
The addition of digital breast tomosynthesis (DBT) into the diagnostic process after breast-conserving therapy (BCT), either in conjunction with digital mammography (DM) or with synthetic 2D images in the diagnostic workup following BCT, significantly decreases the proportion of studies classified as probably benign, significantly increases the rate of studies classified as normal or benign, and significantly increase in the positive predictive value (PPV) of malignancy without significant difference in the patients classified as BI-RADS category 4 or 5. Moreover it improved diagnostic confidence in biopsy recommendations, regardless of mammographic density.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AD:
-
Architectural distortion.
- BCT:
-
Breast conservation therapy.
- BI-RADS:
-
Breast Imaging Reporting and Data System lexicon.
- CC:
-
Craniocaudal.
- DBT:
-
Digital Breast Tomosynthesis.
- DM:
-
Digital Mammography.
- MLO:
-
Mediolateral oblique,
- MRI:
-
Magnetic resonance imaging,
- PPV:
-
Positive predictive value
References
Darby S, McGale P, Correa C et al (2011) Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: a meta-analysis of individual patient data for 10 801 women in 17 randomized trials Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Lancet 378(9804):1707–1716
Cuzick J, Sestak I, Baum M et al (2010) Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol 11(12):1135–1141
Lu WL, Jansen L, Post WJ et al (2009) Impact on survival of early detection of isolated breast recurrences after the primary treatment for breast cancer: a meta-analysis. Breast Cancer Res Treat 114(3):403–412
Swinnen J, Keupers M, Soens J et al (2018) Breast imaging surveillance after curative treatment for primary non-metastasised breast cancer in non-high-risk women: a systematic review. Insights Imaging 9:961–970
Monticciolo DL, Newell MS, Moy L et al (2018) Breast cancer screening in women at higher-than-average risk: recommendations from the ACR. J Am Coll Radiol 15:408–414
Lin K, Eradat J, Mehta NH et al (2008) Is a short-interval postradiation mammogram necessary after conservative surgery and radiation in breast cancer? Int J Radiat Oncol Biol Phys 72:1041–1047
Hymas RV, Gaffney DK, Parkinson BT et al (2012) Is short-interval mammography necessary after breast conservation surgery and radiation treatment in breast cancer patients? Int J Radiat Oncol Biol Phys 83:519–524
Hofvind S, Hovda T, Holen AS et al (2018) Digital breast tomosynthesis and synthetic 2D mammography versus digital mammography: evaluation in a population-based screening program. Radiology 287:787–794
Gennaro G, Toledano A, di Maggio C et al (2010) Digital breast tomosynthesis versus digital mammography: a clinical performance study. Eur Radiol 20:1545–1553
Raghu M, Durand MA, Andrejeva L et al (2016) Tomosynthesis in the diagnostic setting: changing rates of BI-RADS Final assessment over time. Radiology 281(1):54–61
Noroozian M, Hadjiiski L, Rahnama-Moghadam S et al (2012) Digital breast tomosynthesis is comparable to mammographic spot views for mass characterization. Radiology 262:61–68
Lamb LR, Bahl M, Hughes KS et al (2018) Pathologic upgrade rates of high-risk breast lesions on digital two-dimensional vs tomosynthesis mammography. J Am Coll Surg 226:858–867
Sia J, Moodie K, Bressel M et al (2016) A prospective study comparing digital breast tomosynthesis with digital mammography in surveillance after breast cancer treatment. Eur J Cancer 61:122–127
Osman NM, Ghany EA, Chalabi N (2018) The added benefit of digital breast tomosynthesis in second breast cancer detection among treated breast cancer patients. Egypt J Radiol Nucl Med 49(4):1182–1186
Mainiero MB, Moy L, Baron P et al (2017) ACR appropriateness criteria® breast cancer screening. J Am Coll Radiol 14:S383-s390
American College of Radiology. BI-RADS atlas: breast imaging reporting and data system. Reston, VA: American College of Radiology; 2013.
Bahl M, Mercaldo S, Vijapura CA et al (2019) Comparison of performance metrics with digital 2D versus tomosynthesis mammography in the diagnostic setting. Eur Radiol 29:477–484
Hakim CM, Chough DM, Ganott MA et al (2010) Digital breast tomosynthesis in the diagnostic environment: a subjective side-by-side review. AJR Am J Roentgenol 195:W172–W176
Poplack SP, Tosteson TD, Kogel CA et al (2007) Digital breast tomosynthesis: initial experience in 98 women with abnormal digital screening mammography. AJR Am J Roentgenol 189:616–623
Mumin NA, Rahmat K, Fadzli F et al (2019) Diagnostic efficacy of synthesized 2D digital breast tomosynthesis in multi-ethnic malaysian population. Sci Rep. 9(1):1459
Yoon JH, Kim EK, Kim GR et al (2020) Comparing recall rates following implementation of digital breast tomosynthesis to synthetic 2D images and digital mammography on women with breast-conserving surgery. Eur Radiol. https://doi.org/10.1007/s00330-020-06992-6
Skaane P, Sebuodegard S, Bandos AI et al (2018) Performance of breast cancer screening using digital breast tomosynthesis: results from the prospective population-based Oslo Tomosynthesis Screening Trial. Breast Cancer Res Treat 169:489–496
Lourenco AP, Barry-Brooks M, Baird GL et al (2015) Mainiero MB. Changes in recall type and patient treatment following implementation of screening digital breast tomosynthesis. Radiology 274:337–342
Fujii MH, Herschorn SD, Sowden M (2019) Detection rates for benign and malignant diagnoses on breast cancer screening with digital breast tomosynthesis in a statewide mammography registry study. AJR 212:706–711
Bahl M, Gaffney S, McCarthy AM et al (2018) Breast cancer characteristics associated with 2D digital mammography versus digital breast tomosynthesis for screening detected and interval cancers. Radiology 287:49–57
Friedewald SM, Rafferty EA, Rose SL et al (2014) Breast cancer screening using tomosynthesis in combination with digital mammography. JAMA 311:2499–2507
McCarthy AM, Kontos D, Synnestvedt M et al (2014) Screening outcomes following implementation of digital breast tomosynthesis in a general-population screening program. J Natl Cancer Inst 13:106
Greenberg JS, Javitt MC, Katzen J et al (2014) Clinical performance metrics of 3D digital breast tomosynthesis compared with 2D digital mammography for breast cancer screening in community practice. AJR 203:687–693
Houssami N (2015) Digital breast tomosynthesis (3D-mammography) screening: data and implications for population screening. Expert Rev Med Dev 12:377
Murphy MC, Coffey L et al (2018) Can the synthetic C view images be used in isolation for diagnosing breast malignancy without reviewing the entire digital breast tomosynthesis data set? Ir J Med Sci 187:1077–1081
Bernardi D, Macaskill P, Pellegrini M et al (2016) Breast cancer screening with tomosynthesis (3Dmammography) with acquired or synthetic 2D mammography compared with 2D mammography alone (STORM-2): a population-based prospective study. Lancet Oncol 17:1105–1113
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial or not for the profit sectors.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design, Material preparation, data collection and analysis were performed by all authors, and all authors wrote and commented on the first draft of the manuscript and all of them read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This prosepective study was approved by the Reasearch Ethics Committee of the Faculty of Medicine at Assiut University in Egypt in Written informed consent was obtained from each patient after receiving information about the details of the study.
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study
Competing interests
The authors whose names are listed on the title page and shared in the Manuscript entitled: "Digital Breast Tomosynthesis in the diagnostic settings of breast cancer patients treated by conservation therapy ", certified that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria, educational grants, participation in speakers, membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmed, S.A., Hassan, R.A., Makboul, M. et al. Digital breast tomosynthesis in the diagnostic settings of breast cancer patients treated by conservation therapy. Egypt J Radiol Nucl Med 55, 67 (2024). https://doi.org/10.1186/s43055-024-01237-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01237-8