Abstract
Background
Predictions about the hospital course of the coronavirus disease 2019 (COVID-19) patients are of paramount value. This research was designed to validate 4C mortality and CT severity scores (CT-SS) as prognostication tools of mortality and detect their relations among patients with COVID-19 who are hospitalized. The identification of other potential mortality risk factors was also evaluated.
Methods
Two hundred and ninety-six confirmed COVID-19 adult cases were prospectively included. They were allocated into 3 groups according to severity; 78 in moderate group, 97 in severe group, and 121 patients in critical group. Patient demographics, clinical characteristics, co-morbidities, lines of treatment, 4C mortality score and CT severity score were assessed upon admission.
Results
The study revealed that 90% and 84.3% sensitivities were observed for 4C mortality and CT-SS respectively as predictors of mortality. Significant correlation between both scores (r = 0.6. p = 0.0001) was detected. Multivariate analysis identified 6.9-fold increased risk of mortality for the patients with 4C mortality score > 9.5 (p = 0.001). CT-SS > 12, age ≥ 60, male gender, hypertension and diabetes mellitus were also found as significant independent factors associated with increased mortality.
Conclusions
Both of 4C mortality score and CT-SS have a high sensitivity as a risk-stratification scores with a considerable correlation. In addition, they represent the most independent risk factors associated with mortality in comparison to other clinical or laboratory indices.
Similar content being viewed by others
Background
The worldwide COVID-19 pandemic is posing a challenge to the world's healthcare systems. Risk stratification is necessary due to the diverse outcomes seen, from subpopulations that are primarily asymptomatic to subpopulations with significant fatality rates. Such risk classification can assist in more effectively directing efforts for both prevention and treatment of confirmed cases (i.e., hospitalization vs community isolation) [1].
Predictions of the patients' hospital course are crucial because patients at a high risk of dying could be prioritized for quick, aggressive treatment. Prior to further deterioration, high-risk patients may get steroid therapy and be quickly transferred to critical care [2].
Numerous prognosis scores for COVID-19 were found in a review article [3], and they differed in terms of context, expected outcome measure, and clinical characteristics covered. One of them is the 4C (Coronavirus Clinical Characterization Consortium) mortality Score [4], which is a risk-score that forecasts in-hospital mortality for COVID-19 patients who are hospitalized. The 4C Mortality Score requires just parameters that are often accessible at hospital presentations, making it simple to utilize. It is based on a patient cohort from the UK.
Early disease detection, disease management, and disease course monitoring all depend on high resolution CT chest imaging. Additionally, the imaging results can be used to determine the severity of the condition, which greatly aids clinicians in using their clinical judgment and ensures effective and prompt care [5]. Using a semi-quantitative grading technique based on the visual evaluation of each implicated lobe, the severity of a CT scan can be evaluated [6].
The accuracy and relation of 4C mortality score to CT severity score need to be evaluated.
This study was done to determine the validity of both of 4C mortality score and CT severity score as a predictor of mortality and their correlation in COVID-19 patients. In addition, the identification of other possible risk factors of mortality was evaluated.
Methods
Design, study population
This prospective study was performed in an isolation facility for COVID-19 patients at the Cardiothoracic Minia University Hospital, patients were enrolled from February 2021 to October 2021.
Inclusion criteria: adult patients > 18 years old with positive polymerase chain reaction (PCR) for SARS-Cov2.
Exclusion criteria: patients known to have chronic lung diseases and patients with congestive heart failure.
Evaluation
Data pertinent to demographics, clinical and laboratory data, co-morbidities, lines of treatment, ventilatory support, length of hospital stay, and outcome data were collected from all patients. 4C mortality score was calculated from all groups. The score of 4C mortality was validated and derived within the ISARIC (International Severe Acute Respiratory and Emerging Infection Consortium) World Health Organization Clinical Characterization Protocol UK study. The age, sex, Glasgow Coma Scale, blood urea nitrogen, C-reactive protein, respiratory rate, peripheral oxygen saturation, and number of comorbidities are all included in the 4C score. The 4C score has risk categories of low (0–3), intermediate (4–8), high (9–14), and very high (15), and spans from 0 to 21 [4].
All cases underwent non-contrast high resolution CT using 16 detector CT scanners (Lightspeed, GE Healthcare, WI), (Aquilion, Toshiba Medical System). The parameters of the CT scanning were used: tube voltage 120 kV; tube current 200–250 mAS; a high resolution-method, using thin slice thickness < 1.5 mm, and the scan matrix was 512 × 512 matrices. The area from the lower neck down to the upper abdomen just below the diaphragm was covered by the CT scan. Coronal and sagittal images were visualized in the lung and mediastinal windows using multi-planner reformat (MPR).
Each of the five lobes was visually assessed on a scale of 0 to 5, and the CT severity score (CT-SS) was derived depending on the degree of lobar involvement. The following scores were assigned: 0 (none), 1 (affecting < 5% of the lobe), 2 (affecting 5–25% of the lobe), 3 (affecting 26–49% of the lobe), 4 (affecting 50–75% of the lobe), and 5 (affecting > 75% of the lobe). So, each lobe might receive a maximum CT score of 5. The five lobe scores were added together to create the total CT score (range from 0 to 25). If the total score is ≤ 7, it is a mild category, 8–17; it is a moderate and ≥ 18; it is severe category [6]. (Figs. 1, 2).
Statistical analysis
Processing the data was carried out using Statistical Package for the Social Sciences (SPSS) software (version 22). Continuous data were represented as mean and standard deviation (SD) while categorical data was expressed using number and percent. For qualitative data between two or three groups, the Chi square test was employed, ANOVA one-way test for quantitative parametric data comparing the three groups.
In the context of the analysis of variance, post hoc analysis was carried out using the least significant difference test (LSD). P < 0.05 is considered significant. With the use of calculations for cut-off value, sensitivity, specificity, positive predicted value (PPV), negative predicted value (NPV), and area under curve (AUC), ROC curves (receiver operating characteristic) for both the 4C mortality score and CT-SS were created. Pearson's r correlation was utilized to test the correlation. A Cox Regression was performed to evaluate predictors of mortality using both univariate and multivariate analyzes.
Results
In this research, 296 patients with COVID-19 were included out of 310 patients who were recruited to the hospital during the enrollment period. Eight patients with underlying lung diseases and 6 patients with congestive heart failure were excluded.
According to disease severity at the time of admission [7] patients were divided into 3 groups: 78 moderate cases: (Group I), 97 severe cases (Group II) and 121 critical cases (Group III).
Moderate cases were patients who exhibit signs of pneumonia by radiography with an oxygen saturation (SpO2) ≥ 94% on room air. Severe cases were identified if one of the following criteria was met: SpO2 < 94% on room air, arterial partial pressure of oxygen to fraction of inspired oxygen ratios below 300 mm Hg, respiratory rates above 30 breaths per minute, or lung infiltrate levels above 50%. If one of the following characteristics was present: respiratory failure, septic shock, and/or multiple organ dysfunction requiring ICU monitoring, the disease was categorized as critical.
Clinical and demographic data are shown in (Table 1). Patients of moderate group of COVID-19 were significantly younger than those of severe and critical categories (p = 0.001). Males were statistically considerably more prevalent in moderate cases than in severe and critical cases (p = 0.023). Comparatively to the severe and critical patients, 55 patients (69.5%) in moderate group experienced dyspnea (p = 0.0001). Patients in the severe group vomited far more frequently than those in the other 2 groups (p = 0.007). Compared to those in the critical group, moderate and severe COVID 19 had a substantial increase in taste and smell loss (p = 0.0001). Additionally, the severe and critical groups had greater tachypnea and oxygen desaturation (p = 0.0001 for each).
Critical group had the highest value for both of 4C mortality score and CT-SS with a significant difference between them versus those of moderate and severe disease categories (p = 0.0001 for each) (Table 2).
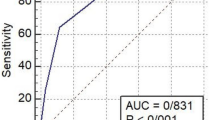
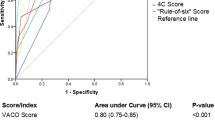
The outcomes of analysis of ROC for both of 4C mortality score and CT-SS as predictors of mortality are represented in Fig. 2 (A and B respectively). The AUC was 0.84 (95% CI 0.80–0.88, p = 0.001) for 4C mortality score at a cut-off value of 9.5 to predict sensitivity and specificity for mortality as 89.9% and 62.8% respectively (Fig. 3A). CT-SS sensitivity and specificity was observed as 84.3% and 64.7% respectively considering a threshold value of 12.5 with AUC of 0.83 (95% CI 0.77–0.89, p = 0.0001) (Fig. 3B).
There is a moderate positive correlation between CT severity score and 4C mortality score (r = 0.6) with statistical significance (p value = 0.0001) (Fig. 4).
Table 3 depicts characteristics of alive and dead patients. The total number of dead patients was 89, 86 in critical group out of 121 and 3 cases in severe group. Alive patients were significantly younger than dead ones (54.7 vs 65.3, p = 0.001) and 70% of non-survivors their ages ≥ 60 years. Non survivors were more in males and had more comorbidities and higher inflammatory markers than survivors. In addition, both of CT-SS and 4C mortality scores were higher as compared to survivors. Regarding ventilatory support, 50% of non survivors used non-invasive and invasive mechanical ventilation, nevertheless no remarkable difference was existent in terms of the length of hospital stay between survivors and non-survivors (9.06 days vs 8.8 days, p = 0.7).
Univariate analysis suggests that clinical variables associated with mortality included age ≥ 60 (p = 0.001), male sex (p = 0.02), hypertension and diabetes mellitus (p = 0.0001 for each), oxygen saturation < 90% (p = 0.0001), 4C mortality score > 9.5 and CT-SS > 12 (p = 0.0001 for each). While the only variables correlated with mortality in multivariate analysis were oxygen saturation < 90%, 4C mortality score and CT SS (p = 0.0001, p = 0.001 and p = 0.02 respectively). (Table 4).
Discussion
It is necessary to develop a quick, accurate scale to identify patients who are most at risk of dying. In the past, scoring systems have been applied to the healthcare system to stratify risk, predict outcomes, and efficiently manage patients [8]. Numerous risk stratification systems in COVID-19 are used to forecast death. In the current study, we used the 4C mortality score and CT severity score among different COVID-19 patient categories to validate their role as a predictor of mortality and to determine their correlations. The range of the 4C mortality score is 0 to 21. Considering this, the anticipated mortality rates is as follows: Low-risk groups ranged from 1.2 to 1.7%, intermediate-risk groups from 9.1 to 9.9%, high-risk groups from 31.4 to 34.9%, and extremely high-risk groups from 61.5 to 66.2% [4].
Our study revealed that the average 4C mortality score in moderate group of patients was 4.8. This value corresponds to an intermediate risk group for mortality with an in-hospital mortality rate of 9.9% in Knight et al., 2020 study [4], but none of the patients in this group in the present study passed away. The severe group got a 4C mortality score of 9.2 and this value had a hospital mortality rate of 34.9% in the original study [4], while just 3.1% of the patients in this group died in the current research. When we calculated this score for the critical group, we found that its mean value was 12.5 and that it corresponded to a high-risk category with 34.9% of in-hospital mortality. However, we found a significantly higher mortality in this group, where 86 out of 121 cases passed away, representing a 71.1% in-hospital mortality rate (Fig. 5).
At a cut-off value of 9.5 for the 4C mortality score across all studied patients, this value had an AUC of 0.84 (95% CI 0.84–0.88, p = 0.001), a sensitivity of 89.9%, a specificity of 62.8%, and positive and negative predicted values for mortality of 51% and 93.5%, respectively. According to Knight and colleagues [4], AUC was 0.79, 95% confidence interval: 0.78 to 0.79) and sensitivity 92.5% at a cut-off value of ≥ 9 to rule in mortality.
Using the same score in a Saudi Arabian study [9], at a cutoff value of 4C mortality score > 9 it had a sensitivity of 70.5%, specificity of 73.97%, positive predictive value of 62.4%, and negative predictive value of 80.2% at AUC of 0.81. The difference in sensitivities in the current study and previous studies can be attributed to difference in populations and criteria of disease severity classification (Fig. 6).
A CT scan can be a useful tool for determining the severity of each patient's condition [6]. Quantitative approaches or software that uses deep learning algorithms to quantify the percentage of affected lung volumes can also be utilized to evaluate the severity [10]. In the present study, we used visual method for assessing CT severity and the mean value of CT severity score among all studied patients was 12.6 (moderate severity) with a sensitivity and specificity of 84.3% and 64.7% respectively for predicting mortality. The mean CT-SS of COVID-19 patients in another Egyptian study was 13.6 (moderate severity) [11].
We found that there was a moderate to strong significant positive correlation between 4C mortality score and CT severity score in COVID-19 patients. Our study is the first to use the 4C mortality score explicitly along with the CT severity score as a prognostication tool. Therefore, a moderate severity CT severity score can be utilized as a complementary for a mortality risk indicator.
The current study revealed that the overall mortality rate was 30.1% and patients of critical group represented 75% of this number. A previous Egyptian multicenter, retrospective study [12] was conducted on all PCR confirmed COVID-19 cases admitted to 6 quarantine hospitals with a total of 3712 hospitalized patients were included; of them, 900 deaths were recorded (24.2%). The higher mortality in our study than an aforementioned one could be attributed to that, patients of critical group represented 41% of the studied patients. No classification of patients according to severity was done in the multicenter study.
On comparison the baseline characteristics of survivors and non-survivors, we found that about 70% of non-survivors, their ages more than 60 years. This finding is consistent with the results of previous study [13] that showed a higher mortality rate in older patients with COVID-19, particularly in those aged ≥ 60 years. We found also that a higher existing comorbidities and mortality, this coincides to the results of a prospective study that was conducted in Spain, in which comorbidities especially hypertension was the most reported previous comorbidity in the non-survivors’ group (61.10%, p < 0.0001) [14]. In addition, both of 4C mortality score and CT severity score were significantly higher in non-survivors than survivors. Regarding the use of ventilatory support, it was revealed that the use of NIV and IMV were more in non-survivors. Another study in China showing that non-survivors were more likely to have received noninvasive mechanical ventilation [57%, p < 0.001], invasive mechanical ventilation [35%, p < 0.001] than survivors [15].
On analysis the associated factors related to mortality, we found that age more than 60 had a significant role in mortality with an odd ratio of 2.7 and this coincides with results of Abdel Ghaffar et al. study [12]. Data from China and Italy reported also that the case fatality rate of COVID-19 significantly increases with age [16]. This may be attributed to immunosenescence, and risk for immunopathology in elderly with decreased B and T lymphocyte activities are major contributors to older persons' susceptibility to severe infection and death [17].
It was found that male gender had a significant risk factor of mortality (OR 1.7) in comparison with females Owing to the higher expression of ACE II in males, which is the main receptor for the binding of SARS-CoV-2 to host cells [18], can contribute to this finding. We found also that either of hypertension and diabetes mellitus had a high odd ratio for mortality on univariate analysis (OR 3.13, p = 0.0001, OR 3.14, p = 0.0001 respectively). A meta-analysis included a total of 24 observational studies with 99,918 COVID-19 patients found that hypertensive patients have a 2.17-fold higher risk for COVID-19 mortality (OR: 2.17; 95% CI 1.67–2.82; P < 0.001) [19].
Another meta-analysis included thirteen studies with a total number of 3027 patients with SARS-CoV-2 infection; they reported that diabetes is associated with an almost fourfold greater risk for severe disease and death in patients with COVID-19 (odds ratio (OR) = 3.68, 95% confidence interval (CI) [2.68–5.03]; P < 0.001) [20].
The current research found that both of 4C mortality score more than 9.5 and CT-SS > 12 had a significant odd ratio of mortality in both of univariate and multivariate analyzes. No previous studies deal with this issue.
Strength and limitation of the study
The current study is the first to correlate the severity of COVID-19, as indicated by CT affection, to other clinical and laboratory variables included in the 4C mortality score, with the goal of highlighting the need for an integrated assessment of COVID 19 patients that includes both clinical and radiological assessment to help us to detect critical cases early.
On analyzing the risk variables associated to mortality, to lower the risk of death; promptly and individually tailor treatment regimens can be utilized for those with a high 4C and CT-severity scores.
Some of the limitations of this study that it is a cross-sectional one and no follow up of survivors after hospital discharge was done, in addition; it is a single center study.
No comparison of 4C mortality score with other simple scores like CURB-65 or Quick COVID-19 Severity Index (QCSI) was evaluated. Further investigation is required to verify the validity of 4C mortality and CT severity scores.
Conclusions
Our findings reveal that both of 4C mortality and CT severity scores have a good sensitivity as a predictor of mortality with a high correlation between them. At a cut-off value of 4C mortality score > 9.5 and CT severity score > 12, they represent the most significant independent risk factors associated with mortality from COVID in comparison to other patient characteristics.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AUC:
-
Area under curve
- COVID:
-
Corona Virus Disease
- CT-SS:
-
Computed tomography severity score
- LSD:
-
Least significant difference test
- NPV:
-
Negative predicted value
- PCR:
-
Polymerase chain reaction
- PPV:
-
Positive predicted value
- QCSI:
-
Quick COVID severity index
- ROC:
-
Receiver operating characteristic
References
Wu JT, Leung K, Bushman M, Kishore N, Niehus R, de Salazar PM et al (2020) Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat Med 26(4):506–510
Bouadma L, Lescure FX, Lucet JC, Yazdanpanah Y, Timsit JF (2020) Severe SARS-CoV-2 infections: practical considerations and management strategy for intensivists. Intensive Care Med 46:579–582
Wynants L, Van Calster B, Collins GS, Riley RD, Heinze G, Schuit E et al (2020) Prediction models for diagnosis and prognosis of covid-19 infection: systematic review and critical appraisal. BMJ 369:m1328
Knight SR, Ho A, Pius R, Buchan I, Carson G, Drake TM et al (2020) ISARIC4C investigators. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO clinical characterization protocol: development and validation of the 4C Mortality Score. BMJ 370:3339
Liu J, Yu H, Zhang S (2020) The indispensable role of chest CT in the detection of coronavirus disease 2019 (COVID-19). Eur J Nucl Med Mol Imaging 47:1638–1639
Francone M, Iafrate F, Masci GM, Coco S, Cilia F, Manganaro L et al (2020) Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. Eur Radiol 30(12):6808–6817
COVID-19 Treatment Guidelines Panel. Coronavirus disease 2019 (COVID-19) treatment guidelines. National Institutes of Health. https://www.covid19treatmentguidelines.nih.gov/on 5/21/2021
Oprita B, Aignatoaie B, Gabor-Postole DA (2014) Scores and scales used in emergency medicine. Practicability in toxicology. J Med Life 7((Spec No. 3)):4–7
Aletreby WT, Mumtaz SA, Shahzad SA, Ahmed I, Alodat MA, Gharba M et al (2022) External validation of 4C ISARIC mortality score in critically ill COVID-19 patients from Saudi Arabia. Saudi J Med Med Sci 10(1):19–24
Huang L, Han R, Ai T, Yu P, Kang H, Tao Q et al (2020) Serial quantitative chest CT assessment of COVID-19: a deep learning approach. Radiol Cardiothorac Imaging 2(2):e200075
Hafez MA, El Hinnawy YH, Nabil DM, Tadros SF (2021) Diagnostic performance of chest computed tomography in coronavirus disease 2019 infection and its correlation with disease severity. Kasr Al Ainy Med J 27:1–6
Abdel Ghaffar MM, Omran D, Elgebaly A, Bahbah EI, Afify S, AlSoda M et al (2022) Prediction of mortality in hospitalized Egyptian patients with Coronavirus disease-2019: a multicenter retrospective study. PLoS ONE 17(1):e0262348
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z et al (2019) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395:1054–1062
Laguna-Goya R, Utrero-Rico A, Talayero P, Lasa-Lazaro M, Ramirez-Fernandez A, Naranjo L et al (2020) IL-6-based mortality risk model for hospitalized patients with COVID-19. J Allergy Clin Immunol 146(4):799–807
Chen L, Yu J, He W, Chen L, Yuan G, Dong F et al (2020) Risk factors for death in 1859 subjects with COVID-19. Leukemia 34(8):2173–2183
Chen Y, Klein SL, Garibaldi BT, Li H, Wu C, Osevala NM et al (2021) Aging in COVID-19: vulnerability, immunity and intervention. Aging Res Rev 65:101205
Pawelec G (2018) Age and immunity: what is “immunosenescence”? Exp Gerontol 105:4–9
Bienvenu LA, Noonan J, Wang X, Peter K (2020) Higher mortality of COVID-19 in males: sex differences in immune response and cardiovascular comorbidities. Cardiovasc Res 116(14):2197–2206
Du Y, Zhou N, Zha W, LV Y, (2021) Hypertension is a clinically important risk factor for critical illness and mortality in COVID-19: a meta-analysis. Nutr Metab Cardiovasc Dis 31(3):745–755
Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J et al (2020) Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect 81(2):e16–e25
Acknowledgements
Lot of thanks for all study participants.
Funding
No funding was received for performing this study.
Author information
Authors and Affiliations
Contributions
A.F.S., A.F.M. and T.E.E. contributed to Conceptualization; A.F.S., A.F.M., T.E.E., and A.H.E. contributed to methodology; A.H.E. contributed to data collection and initial analysis; A.F.S., A.F.M, T.E.E. and A.H.E. contributed to writing—original draft preparation and editing. All authors have read and agreed to the published version of the manuscript. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods that used in this study were done in accordance to the declaration of Helsinki and clinical practice guidelines. The study protocol was approved by the Research Ethics Committee of Faculty of Medicine, Minia University, Approval number (10/2/2021). An informed written consent was obtained from patients before enrollment and this was mentioned in the study protocol.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Said, A.F., El-Fateh, A.H., Esmaeel, T.E.Z. et al. 4C mortality score and CT severity score among COVID-19 patients: a single center prospective study. Egypt J Radiol Nucl Med 55, 34 (2024). https://doi.org/10.1186/s43055-024-01210-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01210-5