Abstract
Background
There are wide-ranging differential diagnoses for the myriad of neurological symptoms associated with non-ketotic hyperglycemia. Similarly, various secondary complications of diabetic ketoacidosis present with nonspecific clinical symptoms. These are inadvertently misdiagnosed as epilepsies and strokes with associated hyperglycemia. Direct association between these nonspecific symptoms and hyperglycemia has been proved by demonstrating their resolution with correction of the latter. This case series portrays the spectrum of few rare neuroimaging findings of uncontrolled hyperglycemia, which helps in proper and prompt diagnoses.
Case presentation
Five diabetic patients with uncontrolled hyperglycemia were observed. Striatal hyperdensity on computed tomography or striatal T1 hyperintensity on magnetic resonance imaging was observed in three patients who presented with movement disorders. The abnormality was bilateral in one case. These observations were consistent with hyperglycemia-induced hemichorea–hemiballismus syndrome. In another patient who had presented with focal seizures, magnetic resonance imaging revealed subcortical T2/FLAIR hypointensity in bilateral occipital regions, which has been described to be characteristic for non-ketotic hyperglycemia-related seizures. Yet another patient who had been treated for diabetic ketoacidosis had developed bilateral lower-limb weakness. In correlation with a background of rapid correction of hyponatremia, magnetic resonance imaging revealed symmetric areas of altered signal intensity in the bilateral perirolandic region showing an open ring pattern of diffusion restriction, suggesting extrapontine myelinolysis.
Conclusions
In all the cases, the clinical differentials were wide. Neuroimaging was mandatory in establishing hyperglycemia as the underlying cause for the movement disorders and seizures. Also, neuroimaging aided in timely identification of extra-pontine myelinolysis, which might have prevented further central pontine involvement in the patient with diabetic ketoacidosis.
Similar content being viewed by others
Background
Hyperosmolar hyperglycemic state (HHS) and diabetic ketoacidosis (DKA) are the most severe acute complications of diabetes mellitus. Secondary complications of DKA and HHS include cerebral edema, cerebral infarction, cortical venous thrombosis, osmotic demyelination and others. These have non-specific symptoms, most commonly presenting as deterioration of prior clinical status.
Uncontrolled non-ketotic hyperglycemia (NKH) without significant serum osmolality derangement can present with a myriad of symptoms such as seizures, focal neurological deficit, movement disorders, hyperthermia and vestibular dysfunction. These are inadvertently misdiagnosed as epilepsies and strokes with associated hyperglycemia. Many researchers have proved the direct association between these non-specific symptoms and hyperglycemia by demonstrating their reversal with targeted therapy. Regarding the secondary complications of DKA-, HHS- and NKH-induced neurological symptoms, imaging using computed tomography (CT) and magnetic resonance imaging (MRI) plays a significant role to help with proper and prompt diagnoses. Neuroimaging also excludes other major treatable causes.
Case presentation
Case 1
A 52-year-old male, with uncontrolled diabetes mellitus, had repeated episodes of abnormal movements of the left upper and lower limb for a period of two months. Clinically, the movement abnormality was diagnosed as chorea. On admission, glycated hemoglobin (HbA1c) was elevated (9.4%, normal range 4–5.6%). Blood examination was negative for ketone bodies. Non-contrast computed tomography (NCCT) of the brain (Fig. 1) demonstrated hyperdense right putamen and right caudate nucleus with age-related diffuse cerebral atrophy. A chronic lacunar infarct was incidentally noted in the left external capsule. Based on the imaging and clinical findings, a final diagnosis of hyperglycemia-induced hemichorea–hemiballismus (HCHB) syndrome was made.
Case 2
A 78-year-old male with diabetes mellitus presented with left upper-limb ballism. In spite of being on oral hypoglycemic agents, he had a high blood glucose level of 450 mg/dl (normal range 70–140 mg/dl) on admission. Urine and blood ketones were negative. HbA1c was elevated (9.5%, normal range 4–5.6%). Serum osmolality was normal (295 mOsm/kg, normal range 275 to 295 mOsm/kg) on admission. MRI (Fig. 2) revealed characteristic T1 hyperintensity involving the contralateral (right) putamen. After a three-month follow-up, there was persistence of ballism movements despite achieving glycemic control. A final diagnosis of hyperglycemia-induced HCHB syndrome was made based on the findings observed.
Case 3
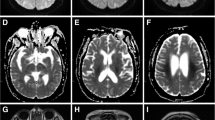
A 69-year-old male with diabetes mellitus presented with bilateral chorea for a period of two weeks. On admission HbA1c was elevated (9.0%, normal range 4–5.6%) and blood glucose was elevated (390 mg/dl, normal range 70–140 mg/dl). Urine ketones were negative. MRI brain (Fig. 3) revealed characteristic T1 hyperintensity involving the bilateral putamen. Based on the imaging and clinical findings, hyperglycemia-induced HCHB syndrome was diagnosed.
Axial fast spin echo T1W MR image (a) and axial T2 weighted (T2W) MR image (b) of brain in a 69-year-old male with hyperglycemia-induced HCHB syndrome. a Bilateral putaminal T1 hyperintensity (long arrows). b Peripheral T2 hyperintensity with central T2 hypo intensity (short arrows) involving the bilateral putamen
Case 4
A 46-year-old male with uncontrolled diabetes mellitus presented with complaints of multiple episodes of facial, right upper-limb spasmodic and jerking movements for a day. On admission, blood glucose was very high (530 mg/dl, normal range 70–140 mg/dl) and ketones were negative. HbA1c levels were also elevated (10.9%, normal range 4–5.6%). Serum osmolality was normal at 295 mOsm/kg (normal range 275–295 mOsm/kg). MRI (Fig. 4a, b) revealed asymmetric subcortical T2/FLAIR hypointensity with overlying gyral hyperintensity in the bilateral occipital regions. On susceptibility weighted imaging (SWI), subtle blooming was seen in the hypointense subcortical regions. The observed findings pointed to a final diagnosis of NKH-related seizures.
Case 5
A 25-year-old female with type I diabetes mellitus presented with altered sensorium and episodes of generalized tonic clonic seizure. On examination, the patient showed kussmaul breathing and had altered sensorium with a Glasgow Coma Scale (GCS) of E4V1M6. Laboratory investigations showed an elevated blood glucose level (632 mg/dL, normal range 70–140 mg/dl). Also elevated HbA1c (11.3%, normal range 4–5.6%), blood urea (53 mg/dl, normal range 5–20 mg/dl) and serum creatinine (1.5 mg/dL, normal range 0.6–1.1 mg/dL) were observed. Metabolic acidosis was confirmed on arterial blood gas examination. Serum sodium level was low (119 mmol/L, normal range 135–145 mmol/L). Initially, serum potassium level was normal (5 mmol/L, normal range 3.5–5.5 mmol/L). Rehydration with 0.9% saline and insulin infusion was immediately started at 0.1 U/kg/h. Unprecedented increase in sodium levels to 139 mmol/L was observed during the first day of treatment with drop in glucose levels by 320 mg/dl. A decrease in potassium levels to 2.6 mmol /L was also observed.
After the first day, the sensorium did not improve effectively and the GCS remained low (E4V2M6). Rehydration was continued with isotonic 5% glucose solution (100 ml/h) and insulin infusion at 0.1 U/kg/h. At the end of second day of therapy, glucose levels were normalized (140 mg/dl) and sodium levels had increased (147 mmol/L). However, the patient’s sensorium only started slowly improving after 36 h of admission (E4V4M6). After complete sensorium improvement at the end of second day, the patient became conscious and fully oriented. However, sudden onset bilateral lower-limb weakness and paresthesia was observed. Prolonged alteration of sensorium and bilateral lower-limb weakness despite the correction of the underlying hyperglycemia led to the suspicion of secondary complications of DKA such as cerebral edema, infarct, dural sinus thrombosis and the rare osmotic demyelination syndrome (ODS).
MRI (Fig. 5a) revealed symmetric well-defined T2 hyperintense areas with concentric inner hypo/hyperintensity in the subcortical and deep white matter of bilateral perirolandic region. DWI (Fig. 5b) showed mild diffusion restriction in the involved areas with an open-ring-like configuration toward the gray matter. No enhancement/blooming was seen.
Coronal T2W MR image (a) and axial DW image (b) of brain in a 25-year-old female with extra-pontine myelinolysis (post-DKA correction). a Symmetric altered signal intensity involving the white matter of bilateral perirolandic region (long arrows). b Open-ring-like diffusion restriction in the involved areas (short arrows)
After 10 days, a follow-up MRI (Fig. 6) was done for case 5, which showed minimal increase in size and T2 signal intensity (Fig. 6a) of the involved areas with normalization of ADC values. MR spectroscopy with intermediate time of echo (TE) 135 ms (Fig. 6b) revealed an elevated choline peak and choline/creatinine ratio suggesting an increased cell-turnover.
There was no hypoxic insult in this case ruling out hypoxic ischemic encephalopathy as a differential. The lesions and symptoms were also not explained by ischemia or edema. In view of raise of serum sodium above the normal limits, the possibility of extrapontine myelinolysis was the most likely. Even after one month of follow-up, the patient had residual bilateral lower-limb weakness (Power—3/5), which did not improve further with therapy.
Discussion
Glucose forms the main source of energy for the neurons of the brain. Though the adult brain makes only 2% of the total body weight, it utilizes around 20% of the total energy derived from glucose [1]. In patients with diabetes mellitus, disturbances in glucose homeostasis occur resulting in severe alteration of normal brain function. Among the two main types of DM, type 1 is predominantly seen in children and young adults where the beta cells responsible for insulin production are destroyed by altered immune function, whereas in type 2 there is an age-related impairment in secretory function of beta cells [2, 3]. Several other types have been described, which are beyond the scope of this article.
HHS and DKA are the most severe acute complications of diabetes mellitus. Though DKA is usually seen in type 1 diabetic patients, it can also result in type 2 patients with conditions of extreme stress. HHS is usually seen in older patients with type 2 DM and an inadequately hydrated status. HHS and DKA can overlap and usually present with alteration of consciousness. Other typical clinical and laboratory findings usually help to clinch the primary diagnosis easily [4]. Secondary complications of DKA and HHS include cerebral edema, cerebral infarction, cortical venous thrombosis, osmotic demyelination and others. These have non-specific symptoms, most commonly presenting as deterioration of prior clinical status.
Uncontrolled NKH can present with a myriad of symptoms such as seizures, focal neurological deficit, movement disorders, hyperthermia and vestibular dysfunction [5]. These are inadvertently misdiagnosed as epilepsies and strokes with associated hyperglycemia. Many researchers have proved the direct association between these non-specific symptoms and hyperglycemia by demonstrating their reversal with targeted therapy [6]. Regarding the secondary complications of DKA-, HHS- and NKH-induced neurological symptoms, imaging using computed tomography (CT) and MRI plays a significant role to help with the proper diagnoses. Neuroimaging also excludes other major treatable causes.
As per previous literature, disappearance of signal abnormality with glycemic control has been observed in many patients [7]. In keeping with the clinical counterpart of this, complete resolution of symptoms was seen in the two patients (case 1 and 3) with symptoms of chorea. Follow-up on imaging could not be done for the reported cases with HCHB. Sites commonly involved include putamen, caudate nucleus, globus pallidus and anterior limb of internal capsule, in the same order of frequency. T1 hyperintense basal ganglia are not specific for NKH and can be observed in other conditions including chronic hepatic encephalopathy, post-cardiac arrest encephalopathy, hypoglycemic coma, and mild focal ischemia. Owing to its resolution following therapy, petechial hemorrhages rather than post ischemic calcifications, have been postulated to be the cause underlying the signal abnormality [7, 8]. Manganese and iron deposition have been found in other causes such as chronic hepatic encephalopathy and neurodegenerative disorders. Cases with bilateral putamina lesions with bilateral, unilateral and no movement disorder each in different patients have been described by various authors [7, 8]. In keeping with this, bilateral movement disorder and bilateral putamina lesions were observed in case 3.
Seizures in diabetic patients occur mostly due to hypoglycemia, DKA or hyperosmolar coma. Reports in literature have shown NKH in itself to present as seizures [9]. Apart from the usual post-ictal changes in MRI such as gyral hyperintensity and diffusion restriction [10], specific MRI findings of NKH have also been reported. Subcortical T2 hypointensity with other associated features such as overlying cortical T2 hyperintensity, focal cortical enhancement and bilateral T2 striatal hyperintensity have been observed in such patients. In keeping with this, MR imaging helped to confirm NKH as the underlying cause for the focal seizures in case 4. Unfortunately, this patient was lost to follow-up and repeat MRI was not done. As per literature, the subcortical hypointensity has resolved after the control of hyperglycemia in most cases. In few patients, the overlying cortical T2 hyperintensity had progressed to gliosis appearing as interval FLAIR hyperintensity [11]. The history of hyperglycemia and electroencephalogram (EEG) findings helped in excluding other mimicking conditions such as hypoxic insult, meningitis and moyamoya disease [12]. The cause of such hypointensity was presumed to be due to mineral deposition and ischemia, with blooming on gradient echo (GRE) sequences supporting the former as was observed in case 4 [13,14,15].
Neuroimaging helps to differentiate the secondary complications of DKA. In case 5, increase in sodium levels of more than 18 mEq over 48 h along with associated hypokalemia raised the suspicion of ODS clinically [16, 17]. MRI helped in revealing the symmetric lesions involving the subcortical and deep white matter of bilateral perirolandic region. Spastic quadriplegia has been observed in many cases of ODS. However, paraplegia observed in this case is very uncommon in ODS. This can be explained by the atypical perirolandic location rather than the usual pontine involvement of central pontine myelinolysis (CPM) [18]. Extrapontine sites of ODS occur most commonly in the basal ganglia and thalamus [19].
Cortico-subcortical location of extrapontine ODS is being increasingly described in the literature [20]. Typically, the lesions have been described to be oriented parallel to the long axis of the gyri and surrounded on three sides by its crown and sides. A thin rim of spared white matter has also been demonstrated between the lesions and the cortical gray matter. This location has been explained by the convergence of neural fibers at a subcortical location where all the myelinotoxic factors from the vascular rich gray matter reach the white matter [21]. Cortical involvement has been observed to be a multifactorial response to associated hypoxia, ischemia and other factors along with osmotic disturbances [22, 23]. The subcortical involvement has been suspected to be more specific for ODS [24, 25]. In keeping with this, the symmetric subcortical lesions and thin rim of spared white matter in case 5 showed a characteristic pattern for ODS. The deep white matter involvement, however, has not been described in the literature to the best of our knowledge.
Also, demyelinating conditions are the most common cause for ring lesions in DWI as has been observed in case 5 [26]. In a case study on ODS, serial MR spectroscopy had revealed an increased choline peak irrespective of the phase of the disease [27], whereas in case of stroke, only chronic infarcts (> 14 days) showed a mild increase in choline peak [28]. An elevated choline peak during the subacute phase of the pathology in this case ruled out the possibility of infarction, in keeping with the above studies. Though there are several reports of cortical and subcortical involvement in extrapontine myelinolysis (EPM) [25], case 5 is unique in that there is deep white matter involvement as well. It has been stated that the extrapontine changes temporally precede the central pontine changes [29,30,31]. Absence of further pontine or basal ganglia involvement even in the follow-up MRI was another unique feature of this case. It is presumed that the timely normalization of the rate of osmolality shift prevented further pontine involvement. Confirmation of diagnosis by histopathology was not available due to patient’s concerns regarding post-procedural neurological complications.
Conclusions
Neuroimaging aids in identifying the basal ganglia abnormalities of hyperglycemia-induced hemichorea, hemiballismus syndrome. Similarly, imaging also helps in demonstrating the typical subcortical hypointensity caused by non-ketotic hyperglycemia-related seizures. By knowing these typical imaging patterns, hyperglycemia can be ascertained to be the sole causative agent. Thereby, inadvertent misdiagnosis of seizures and strokes having mere association with hyperglycemia can be avoided. In rare scenarios of osmotic demyelination secondary to correction of diabetic ketoacidosis, extra-pontine involvement identified at imaging may help in timely correction of the osmolality shift preventing further central pontine involvement. Further research on a broader perspective will be required to explain the pathogenesis of this rare presentation of osmotic demyelination syndrome.
Availability of data and materials
There are no raw data used in this study. This case series is purely based on images. Other than images, to confirm uncontrolled hyperglycemia, glycated hemoglobin (HbA1c) and serum osmolality were considered which is presented in the article itself. There are no data or statistical analysis involved. There are no raw data and no information that can be provided in a supplementary file or depositing it in a public repository. Therefore, data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- CNS:
-
Central nervous system
- CPM:
-
Central pontine myelinolysis
- CT:
-
Computed tomography
- DKA:
-
Diabetic ketoacidosis
- DM:
-
Diabetes mellitus
- DWI:
-
Diffusion-weighted imaging
- EEG:
-
Electroencephalogram
- EPM:
-
Extrapontine myelinolysis
- GCS:
-
Glasgow Coma Scale
- GRE:
-
Gradient echo sequences
- HbA1c:
-
Glycated hemoglobin
- HCHB:
-
Hemichorea–hemiballismus syndrome
- HHS:
-
Hyperosmolar Hyperglycemic State
- MRI:
-
Magnetic resonance imaging
- NAA:
-
N-acetyl aspartate
- NCCT:
-
Non-contrast computed tomography
- NKH:
-
Non-ketotic hyperglycemia
- ODS:
-
Osmotic demyelination syndrome
- SWI:
-
Susceptibility weighted imaging
- TE:
-
Time of Echo
- T1W:
-
T1 weighted
- T2W:
-
T2 weighted
References
Mergenthaler P, Lindauer U, Dienel GA, Meisel A (2013) Sugar for the brain: the role of glucose in physiological and pathological brain function. Trends Neurosci 36(10):587–597
Saberzadeh-Ardestani B, Karamzadeh R, Basiri M, Hajizadeh-Saffar E, Farhadi A, Shapiro AMJ et al (2018) Type 1 diabetes mellitus: cellular and molecular pathophysiology at a glance. Cell J 20(3):294–301
Lee PG, Halter JB (2017) The pathophysiology of hyperglycemia in older adults: clinical considerations. Diabetes Care 40(4):444–452
Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN (2009) Hyperglycemic crises in adult patients with diabetes. Diabetes Care 32(7):1335–1343
Borensztein A, Walker RH, Schell R, Guber HA (2015) Hyperglycemia-induced involuntary movements: 2 case reports and a review of the literature. AACE Clin Case Rep 1(3):e165–e169
Chua CB, Sun CK, Hsu CW, Tai YC, Liang CY, Tsai IT (2020) “Diabetic striatopathy”: clinical presentations, controversy, pathogenesis, treatments, and outcomes. Sci Rep 10(1):1–11
Oh SH, Lee KY, Im JH, Lee MS (2002) Chorea associated with non-ketotic hyperglycemia and hyperintensity basal ganglia lesion on T1-weighted brain MRI studya meta-analysis of 53 cases including four present cases. J Neurol Sci 200(1–2):57–62
Zheng W, Chen L, Chen JH, Lin X, Tang Y, Lin XJ et al (2020) Hemichorea associated with non-ketotic hyperglycemia: a case report and literature review. Front Neurol 11:1–6
Çokar Ö, Aydin B, Özer F (2004) Non-ketotic hyperglycaemia presenting as epilepsia partialis continua. Seizure 13(4):264–269
Flacke S, Wüllner U, Keller E, Hamzei F, Urbach H (2000) Reversible changes in echo planar perfusion- and diffusion-weighted MRI in status epilepticus. Neuroradiology 42(2):92–95
Raghavendra S, Ashalatha R, Thomas SV, Kesavadas C (2007) Focal neuronal loss, reversible subcortical focal T2 hypointensity in seizures with a nonketotic hyperglycemic hyperosmolar state. Neuroradiology 49(4):299–305
Hiremath SB, Gautam AA, George PJ, Thomas A, Thomas R, Benjamin G (2019) Hyperglycemia-induced seizures—understanding the clinico- radiological association. Indian J Radiol Imaging 29:343–349
Putta SL, Weisholtz D, Milligan TA (2014) Occipital seizures and subcortical T2 hypointensity in the setting of hyperglycemia. Epilepsy Behav Case Rep 2(1):96–99
De Martino SRM, Toni F, Spinardi L, Cirillo L (2020) Magnetic resonance imaging findings in patients with non-ketotic hyperglycaemia and focal seizures. Neuroradiol J 33(5):416–423
Amar JY, Bhattacharya AK, Uzo-Okereke AM, Chou CA, Vo KD, Goyal MS et al (2022) Location-atypical lesions in non-ketotic hyperglycemic epilepsy: expanding the clinico-radiographic phenotype. Epileptic Disord 24(6):1102–1109
Dhawan VB, Guru BN (2022) MRI findings in osmotic demyelination syndrome—a report of two cases. J Clin Diagn Res 16(12):10–12
Tandukar S, Rondon-Berrios H (2019) Treatment of severe symptomatic hyponatremia. Physiol Rep 7(21):1–7
King JD, Rosner MH (2010) Osmotic demyelination syndrome. Am J Med Sci 339(6):561–567
Zunga PM, Farooq O, Dar MI, Dar IH, Rashid S, Rather AQ et al (2015) Extra pontine osmotic demyelination syndrome. Ann Neurosci 22(1):51–53
Lv X, Hong Q, Lin X, Chen W, Tian Y (2021) Osmotic demyelination syndrome: clinical, neuroimaging characteristics, and outcomes in a series of 18 cases. Biomed Res Int 28:1–9
Okeda R, Kitano M, Sawabe M, Yamada I, Yamada M (1986) Distribution of demyelinating lesions in pontine and extrapontine myelinolysis—three autopsy cases including one case devoid of central pontine myelinolysis. Acta Neuropathol 69(3–4):259–266
Lambeck J, Hieber M, Dreßing A, Niesen W-D (2019) Central pontine myelinosis and osmotic demyelination syndrome. Dtsch Arztebl Int 116(35–36):600–606
Roh JH, Kim JH, Oh K, Kim SG, Park KW, Kim BJ (2009) Cortical laminar necrosis caused by rapidly corrected hyponatremia. J Neuroimaging 19(2):185–187
Bourgouin PM, Chalk C, Richardson J, Duang H, Vezina JL (1995) Subcortical white matter lesions in osmotic demyelination syndrome. Am J Neuroradiol 16(7):1495–1497
Tatewaki Y, Kato K, Tanabe Y, Takahashi S (2012) MRI findings of corticosubcortical lesions in osmotic myelinolysis: report of two cases. Br J Radiol 85(1012):87–90
Finelli PF, Foxman EB (2014) The etiology of ring lesions on diffusion-weighted imaging. Neuroradiol J 27(3):280–287
Guo Y, Hu JH, Lin W, Zheng KH (2006) Central pontine myelinolysis after liver transplantation: MR diffusion, spectroscopy and perfusion findings. Magn Reson Imaging 24(10):1395–1398
Lin AQ, Shou JX, Li XY, Ma L, Zhu XH (2014) Metabolic changes in acute cerebral infarction: findings from proton magnetic resonance spectroscopic imaging. Exp Ther Med 7(2):451–455
Garg P, Aggarwal A, Malhotra R, Dhall S (2019) Osmotic demyelination syndrome—evolution of extrapontine before pontine myelinolysis on magnetic resonance imaging. J Neurosci Rural Pract 10(1):126–135
Babanrao SA, Prahladan A, Kalidos K, Ramachandran K (2015) Osmotic myelinolysis: Does extrapontine myelinolysis precede central pontine myelinolysis? Report of two cases and review of literature. Indian J Radiol Imaging 25(2):177–183
Lee C, Ko C (2021) Temporal brain MRI changes from extrapontine myelinolysis to central pontine myelinolysis: a case report. Cureus. 13(11):1–5
Acknowledgements
Not applicable.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
“Dr. SBP and Dr. AJ analyzed and interpreted the MRI and CT brain images of patients with uncontrolled hyperglycemia. Both the authors read and approved the manuscript”.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This manuscript does not report or involve the use of any animal or human data based on a clinical trial and does not involve human or animal tissue, hence it is not applicable.
Consent for publication
Consent to publish obtained from the individuals and their identity is not disclosed in the manuscript.
Competing interests
The authors declare that they have no competing interests in this section.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Panneer, S.B., Jain, A. Neuroimaging in uncontrolled hyperglycemia: a case series and literature review. Egypt J Radiol Nucl Med 55, 36 (2024). https://doi.org/10.1186/s43055-024-01195-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01195-1