Abstract
Background
Rheumatoid arthritis (RA) is an inflammatory disease that can lead to progressive joint damage. Early identification of synovitis is key in the management of patients with RA. The aim of this study was to assess synovitis in patients with RA using 99mTc-glucosamine single photon emission computed tomography/computed tomography (SPECT/CT) imaging and compare this radiopharmaceutical's diagnostic performance with ultrasound (US) imaging. This prospective study included 22 participants with active RA and 380 joints were assessed with SPECT/CT and US imaging. SPECT/CT imaging of the joints of interest was performed in each participant three hours after injection of 99mTc-glucosamine, with US imaging of the same joints performed on the same day. The affected joints were qualitatively assessed for 99mTc-glucosamine uptake and compared with the findings on US imaging.
Results
Abnormal increased uptake of 99mTc-glucosamine, localized specifically to the synovial space, was noted in the affected joints. The overall sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy of 99mTc-glucosamine SPECT/CT imaging were 86%, 60%, 61%, 85% and 73%, respectively. A sensitivity of 100% was noted in the identification of synovitis in the carpal and knee joints. Disease activity in the distal interphalangeal (DIP) joints was not observed with either SPECT/CT or US.
Conclusions
SPECT/CT imaging with 99mTc-glucosamine is a valuable tool for assessing disease activity in the joints of patients with RA. It has a very high sensitivity in detecting synovitis and it correlates very well with US imaging in this regard.
Similar content being viewed by others
Background
Rheumatoid arthritis (RA) is a chronic inflammatory disease characterized by progressive damage to the joints. Joint damage begins early in the course of the disease as a consequence of the active inflammation, and can lead to progressive and irreversible disability [1]. Therefore, prompt diagnosis and early treatment are imperative in patients with RA. For early diagnosis to be feasible, an investigation that can offer an accurate assessment of disease activity, with very high sensitivity even in the setting of subclinical disease, is required. Several methods to evaluate disease activity in RA are available. These methods involve clinical assessment of involved joints, laboratory and imaging investigations, or a combination of two or more methods.
A number of validated clinical scoring systems, including the 28-Joint Disease Activity Score (DAS-28), the Simplified Disease Activity Index (SDAI) and the Clinical Disease Activity Index (CDAI), allow for the classification of the patient as being in remission or presenting with low, moderate or high disease activity [2, 3]. However, non-specific constitutional symptoms such as fatigue and malaise, rather than arthritis, predominate in some patients [4] and the subjective nature of a clinical assessment reduces the diagnostic accuracy of these validated clinical scoring methods. Laboratory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are nonspecific tests that are occasionally helpful in distinguishing between inflammatory and non-inflammatory conditions. However, these tests are not diagnostic for RA and may be abnormal in many infectious, malignant, and other disease conditions [5]. Several imaging modalities can also be used and have been shown to be useful in the management of patients with RA. The most commonly used modality is X-ray imaging, despite knowing that structural changes such as erosion may not be evident in early disease [6,7,8]. X-ray has the best-established role in identifying progressive joint damage. However, its sensitivity is inadequate for identifying synovitis and early erosive lesions [8, 9].
The new classification criteria often used to diagnose RA, proposed by the American College of Rheumatology/European League Against Rheumatism (ACR/EULAR), incorporated the role of ultrasound (US) and magnetic resonance imaging (MRI) in the detection of synovitis, thus enabling earlier diagnosis and correct classification of patients [3, 6]. In recent years, the use of US imaging in the assessment of inflammatory joints, especially due to RA, has increased.
Universally, US is one of the most widely available, safe and cost-effective imaging modalities used for evaluating patients with RA. In addition, it offers the prospect of a more accurate assessment of soft tissue inflammation than conventional clinical examination [10]. Synovitis and effusions are readily observed with US, and it has been shown to detect synovitis more accurately than clinical examination [10]. However, the drawback of US is that it is operator-dependent [4, 11] and cumbersome, especially when almost every single joint in both hands needs to be evaluated. Performing the procedure could become even more labor-intensive and time-consuming when additional joints besides those in the hands also need to be examined. The currently accepted practice, however, is to use morphological changes (synovial effusion and hypertrophy) occurring on US gray scale imaging and hypervascularity observed by power Doppler to grade disease activity [12]. Both US gray scale and power Doppler findings have been shown to be very sensitive to changes in disease activity [10].
Positron emission tomography/computed tomography (PET/CT) imaging of RA using fluorine- 18-fluorodeoxyglucose (18F-FDG) is becoming a popular nuclear medicine imaging modality in patients with RA. Evidence has been reported extensively in the literature that PET-CT is very sensitive in evaluating disease activity [13,14,15,16,17,18,19]. Technetium-99-metastable ethylenedicysteine-deoxyglucose (99mTc-ECDG), also referred to as 99mTc-glucosamine, is a single-photon emission computed tomography (SPECT) radiotracer for functional imaging [20]. This radiopharmaceutical has not been as widely investigated as 18F-FDG in evaluating disease activity in patients with RA. However, few investigators have reported good sensitivity of 99mTc-glucosamine in evaluating the disease activity of patients with RA [11, 20]. Not every nuclear medicine center has access to a PET/CT camera, making 99mTc-glucosamine imaging an alternative in centers with only SPECT/CT cameras. However, 99mTc-glucosamine must be compared extensively to one of the valid, sensitive, and reliable imaging modalities, such as US, before it should be considered a good alternative to 18F-FDG imaging in patients with RA. No studies that extensively evaluated the diagnostic performance of this radiopharmaceutical in RA have been reported in the literature. Therefore, the aim of this prospective study was to compare the diagnostic outcome of 99mTc-glucosamine with US in the evaluation of disease activity in patients with RA.
Methods
Study design and population
For this prospective cross-sectional study, 22 patients diagnosed with RA by an experienced rheumatology consultant (25 years' experience) according to the ACR/EULAR classification criteria, were recruited to participate. The participants were recruited from the rheumatology clinic at our institution between February and October 2022. Twelve participants had confirmed RA affecting the hands, while 10 had confirmed RA affecting the knees.
Inclusion criteria
-
Participants who are ≥ 18 years of age
-
Participants must have been diagnosed with RA of the joints in the hands according to the ACR/EULAR classification criteria for RA.
Exclusion criteria
-
Pregnant participants
-
Lactating participants
-
Participants younger than 18 years of age
Synthesis of the radiopharmaceutical 99mTc-glucosamine
The ECDG ligand was synthesized according to the procedure described by Yang et al. [21]. The ECDG ligand was successfully formulated into buffered kits that were stably stored in a -80 °C freezer. Fifty to sixty millicurie (mCi) of Tc-99 m pertechnetate (99mTcO4-) was added to a prepared, lyophilized ECDG kit vial. The solution was then heated at 75 °C for 15 min. Quality control was performed on the radiolabeled product by testing pH (pH 5.5) and radiochemical purity (> 95%). Radiochemical purity was determined by using high performance liquid chromatography on a Varian Prostar 325 UV/Vis HPLC machine (Varian Medical Systems Inc.; Palo Alto, CA, USA) fitted with a radiometric GABI Star gamma detector (Raytest GmbH; Straubenhardt, Germany) and thin layer chromatography (Raytest GmbH; Straubenhardt, Germany).
99mTc-glucosamine administration
The prepared radiolabeled solution was added to 3 mL of sterile saline and then filtered into a sealed sterile vial. Additional saline was added to the vial to ensure a final volume of approximately 5 mL. A participant activity of 20–25 mCi was withdrawn for intravenous administration.
Imaging protocol and processing
All 22 participants were scanned using a dual-head gamma camera (Siemens Symbia T16 True Point SPECT-CT; Siemens Medical Solutions; Malvern, PA, USA). The SPECT/CT camera was equipped with a low-energy, high-resolution collimator (LEHR). Three hours after radiopharmaceutical administration, SPECT images of the relevant joints (either the hands/wrist or knees) were performed at 25 s/stop, with 3° steps, in a 128 × 128 matrix. This was followed by a low dose, non-contrast CT with the patient in the same bed position. Tube voltage of the CT was 110 kV and the tube current was 25mAs. Images were processed using the Syngo workstation (Siemens Medical Solutions; Malvern, PA, USA) on the gamma camera. SPECT images were reconstructed using an iterative algorithm and SPECT/CT fusion images were obtained using the multimodality Syngo imaging software on the workstation.
Ultrasound imaging
Ultrasound was performed by an experienced musculoskeletal ultrasonographer on the same day as the 99mTc-glucosamine using a Samsung HS70A (Innovative Ultrasound Imaging, Inc.; San Diego, CA, USA) high frequency 15 MHz transducer with power Doppler functions.
Data collection and analysis
The data of each patient were collected using an Excel 2019 spreadsheet (Microsoft Corporation; Redmond, WA, USA) and analyzed by means of the statistical package Stata version 16 (StataCorp LP; College Station, TX, USA). Results for variables such as sex were presented as frequencies and percentages. Age was presented as the median and interquartile range. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and diagnostic accuracy for 99mTc-glucosamine imaging were calculated.
Image interpretation
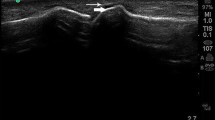
The attenuated corrected and non-corrected SPECT images were qualitatively assessed for an abnormally increased uptake of the radiopharmaceutical localized in the joint space on CT by an experienced nuclear medicine consultant (7 years’ experience). Abnormally increased uptake of 99mTc-glucosamine suggestive of disease activity was identified as activity exceeding that of the surrounding muscle. On US imaging, synovitis was identified by an experienced musculoskeletal radiology consultant (10 years' experience) by assessing synovial hypertrophy detected on US gray scale and a positive power Doppler signal. Both the nuclear medicine physician and radiologist were blinded to each other’s findings.
Ethical considerations
Ethics approval was obtained from the institutional Health Sciences Research Ethics Committee (HSREC) (reference number UFS-HSD2020/1292/2411). Written informed consent was obtained from each participating patient.
Results
The median age was 59 years (interquartile range [IQR] 49–68 years) and the vast majority of patients were female (n = 21; 95.5%). Optimal images with a good target-to-background ratio were obtained for all the participants. All the participants with positive disease on 99mTc-glucosamine imaging had an abnormally increased uptake of the radiopharmaceutical localized to the synovial space, with no bone uptake. An example is illustrated in Fig. 1, showing 99mTc-glucosamine SPECT/CT and SPECT images of the knee of a 72-year-old female with abnormal increase uptake of the radiopharmaceutical in both knees, localized to the synovial space, with no abnormal bone uptake. Twelve (54.5%) participants had the joints of their hands and wrists evaluated, while in the remaining 10 (45.5%) patients, the knee joints were evaluated. A total of 380 joints were evaluated for disease activity, representing 360 joints in both hands, which included the metacarpophalangeal (MCP) joints, proximal interphalangeal (PIP) joints and distal interphalangeal (DIP) joints. Twenty-four carpal joints and 20 knee joints were also assessed for disease activity. Each knee joint was further subdivided into four regions (suprapatellar, lateral, medial, and popliteal regions). Both US and 99mTc-glucosamine imaging did not detect disease activity in any of the DIP joints.
Assessing the total number of joints and regions, 99mTc-glucosamine imaging had an overall sensitivity of 86%, specificity of 60%, PPV of 61%, NPV of 85% and accuracy of 73%. The diagnostic performance of 99mTc-glucosamine imaging in the various group of joints is summarized in Table 1. The diagnostic accuracy of 99mTc-glucosamine imaging was 70% when considering all four regions in each of the knee joints (a total of 80 locations), as shown in Table 2.
Discussion
To the authors knowledge, this has been the first prospective study to directly compare SPECT/CT 99mTc-glucosamine imaging with US imaging in the evaluation of disease activity in joints affected by RA. Using arthroscopy or MRI as the gold standard, a number of studies found that gray scale and Doppler US imaging had a very high diagnostic accuracy in the evaluation of synovitis in patients with RA [8, 22]. We observed an overall sensitivity of 86% for 99mTc-glucosamine SPECT/CT imaging in identifying active disease in patients with RA compared to US imaging. This finding was consistent with an earlier hypothesis by Manolios et al. [11], who confirmed that 99mTc-glucosamine imaging of patients with RA had a good correlation with MRI findings and could identify synovitis in all affected joints [11]. In our study, the sensitivity of 99mTc-glucosamine imaging reached the 100% in the knee and carpal joints, compared to 83% in the joints of the hands. This finding might be suggestive of US being slightly more sensitive in detecting disease activity in the small joints of the hand than 99mTc-glucosamine imaging.
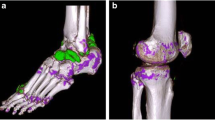
The overall specificity of 99mTc-glucosamine imaging in our study was 60%. Angelides et al. [20] reported that 99mTc-glucosamine uptake was present at sites of osteoarthritis (OA) and subclinical OA. We suspect that the specificity of 60% might be associated with radiopharmaceutical uptake in unknown sites of osteoarthritis, subclinical disease, or a combination of both. The site with the highest level of specificity (90%) were the knees when considered as a single site, and not split into the four separate regions. However, when broken down into the different regions, the specificity dropped to 44%, which was most probably due to abnormal 99mTc-glucosamine uptake in the medial and lateral regions, with specificities of 15% and 17%, respectively, as shown in Table 2. Again, this might be attributed to the identification of subclinical disease not observed on the US imaging, or non-specific uptake in co-existing OA. What might have favored the identification of subclinical disease was the fact that in six of the ten participants who had a follow-up US six weeks after their baseline US, sonographic evidence of synovitis was discovered in a total of 10 knee regions previously negative for synovitis on the baseline US examination, although it had been positive on the baseline 99mTc-glucosamine imaging. An example of this observation is illustrated in Fig. 2, which shows 99mTc-glucosamine SPECT/CT and SPECT images of the knee of a 51-year-old female with abnormal increase uptake of the radiopharmaceutical in all four regions of the left knee joint. Baseline ultrasound imaging was initially negative for disease in the popliteal, medial, and lateral regions of the joint, but positive on subsequent 6 weeks follow-up imaging. This figure also shows that SPECT/CT imaging localizes the radiopharmaceutical uptake in the synovial space without bone involvement. This was a finding peculiar to all the participants.
99mTc-glucosamine SPECT/CT and SPECT images of the knee of a 51-year-old female showing abnormal increase uptake of tracer in all four regions of the left knee joint. Baseline US imaging was initially negative for disease in the popliteal, medial, and lateral components, but positive on subsequent six weeks follow-up imaging
It has been reported in the literature that various nuclear medicine imaging modalities compare well with conventional imaging in identifying active disease in patients with RA [13, 14, 23,24,25,26,27,28,29].
The most popular modality is 18F-FDG PET/CT imaging, which seems to be similar to 99mTc-glucosamine imaging, as both radiopharmaceuticals are radiolabeled analogs of glucose.
Beckers et al. determined that positive 18F-FDG PET findings correlated well with US imaging in detecting active disease in the joints of patients with RA [17], similar to the finding observed in our study. We, however, do recommend that a more robust study similar to ours be performed with 18F-FDG PET/CT.
A limitation of this study was not identifying and/or excluding participants with possible co-existing OA. It has previously been shown that patients with OA might have mildly increased 99mTc-glucosamine uptake [20], a finding that might be difficult to differentiate from subclinical RA. This is however an area that might need further investigation in the future.
Conclusions
This study demonstrated that SPECT/CT imaging with 99mTc-glucosamine had a high sensitivity in detecting synovitis in patients with RA, which compares well with US imaging. However, the specificity was low, which could be attributed to nonspecific uptake of the radiopharmaceutical in patients with co-existing OA or the identification of subclinical disease that had been missed on US imaging. We are of the opinion that this is an area that might warrant more research for clarity. Overall, 99mTc-glucosamine might have a role to play in the evaluation of disease activity in patients with RA, especially in centers that do not have PET/CT cameras for 18F-FDG PET/CT imaging.
Availability of data and materials
All data and material of the article are readily available.
Abbreviations
- RA:
-
Rheumatoid arthritis
- DAS-28:
-
28-joint disease activity score
- SDAI:
-
Simplified disease activity index
- CDAI:
-
Clinical disease activity index
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- ACR/EULAR:
-
American college of rheumatology/European league against rheumatism
- US:
-
Ultrasound
- MRI:
-
Magnetic resonance imaging
- PET/CT:
-
Positron emission tomography/computed tomography
- 18F-FDG:
-
Fluorine-18-fluorodeoxyglucose
- 99mTc-ECDG:
-
Technetium-99-metastable ethylenedicysteine-deoxyglucose
- SPECT:
-
Single-photon emission computed tomography
- mCi:
-
Millicurie
- 99mTcO4-:
-
Tc-99 m pertechnetate
- LEHR:
-
Low-energy, high-resolution collimator
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- HSREC:
-
Health sciences research ethics committee
- IQR:
-
Interquartile range
- MCP:
-
Metacarpophalangeal
- PIP:
-
Proximal interphalangeal
- DIP:
-
Distal interphalangeal
- OA:
-
Osteoarthritis
References
Smolen JS, Aletaha D (2010) The assessment of disease activity in rheumatoid arthritis. Clin Exp Rheumatol 28:18–27
Hodkinson B, van Duuren E, Pettipher C, Kalla A (2013) South African recommendations for the management of rheumatoid arthritis: an algorithm for the standard of care in. S Afr Med J 103:577–585
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO et al (2010) Rheumatoid arthritis classification criteria: an American College of rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis 69:1580–1588
Ally MMTM, Visser C (2010) Rheumatoid arthritis. S Afr Orthop J 9:30–33
Shojania K (2000) Rheumatology: 2. what laboratory tests are needed? Can Med Assoc J 162:1157–1163
Kgoebane K, Ally MMTM, Duim-Beytell MC, Suleman FE (2018) The role of imaging in rheumatoid arthritis. S Afr J Radiol 22:1316
Scheel AK, Hermann KGA, Ohrndorf S, Werner C, Schirmer C, Detert J et al (2006) Prospective 7 year follow up imaging study comparing radiography, ultrasonography, and magnetic resonance imaging in rheumatoid arthritis finger joints. Ann Rheum Dis 65:595–600
Backhaus M, Kamradt T, Sandrock D, Loreck D, Fritz J, Wolf KJ et al (1999) Arthritis of the finger joints: a comprehensive approach comparing conventional radiography, scintigraphy, ultrasound, and contrast-enhanced magnetic resonance imaging. Arthritis Rheum 42:1232–1245
Backhaus M, Burmester GR, Sandrock D, Loreck D, Hess D, Scholz A et al (2002) Prospective two year follow up study comparing novel and conventional imaging procedures in patients with arthritic finger joints. Ann Rheum Dis 61:895–904
D’Agostino MA, Terslev L, Aegerter P, Backhaus M, Balint P, Bruyn GA et al (2017) Scoring ultrasound synovitis in rheumatoid arthritis: a EULAR-OMERACT ultrasound taskforce – Part 1: definition and development of a standardised, consensus-based scoring system. RMD Open. https://doi.org/10.1136/rmdopen-2016-000428
Manolios N, Ali M, Camden B, Aflaky E, Pavic K, Markewycz A et al (2016) Evaluating disease activity in patients with ankylosing spondylitis and rheumatoid arthritis using 99mTc-glucosamine. Eur J Rheumatol 3:65–72
do Prado AD, Staub HL, Bisi MC, da Silviera IG, Mendonca JA, Polido-Periera J, et al (2018) Ultrasound and its clinical use in rheumatoid arthritis: where do we stand? Adv Rheumatol 58:19
Amat J, Chanchou M, Olagne L, Descamps L, Flaus A, Bouvet C et al (2020) Utility of 18F-fluorodeoxyglucose positron emission tomography in inflammatory rheumatism, particularly polymyalgia rheumatica: a retrospective study of 222 PET/CT. Front Med 7:394
Watanabe T, Takase-Minegishi K, Ihata A, Kunishita Y, Kishimoto D, Kamiyama R et al (2016) (18)F-FDG and (18)F-NaF PET/CT demonstrate coupling of inflammation and accelerated bone turnover in rheumatoid arthritis. Mod Rheumatol 26(1):80–87
Chaudhari AJ, Ferrero A, Godinez F, Yang K, Shelton DK, Hunter JC et al (2016) High-resolution (18)F-FDG PET/CT for assessing disease activity in rheumatoid and psoriatic arthritis: findings of a prospective pilot study. Br J Radiol 89:20160138
Wang SC, Xie Q, Lv WF (2014) Positron emission tomography/computed tomography imaging and rheumatoid arthritis. Int J Rheum Dis 17:248–255
Beckers C, Ribbens C, André B, Marcelis F, Kaye O, Mathy L et al (2004) Assessment of disease activity in rheumatoid arthritis with 18F-FDG PET. J Nucl Med 45:956–964
Fosse P, Kaiser MJ, Namur G, de Seny D, Malaise MG, Hustinx R (2018) 18F-FDG PET/CT joint assessment of early therapeutic response in rheumatoid arthritis patients treated with rituximab. Eur J Hybrid Imaging 2:6
Beckers C, Jeukens X, Ribbens C, Andre B, Marcelis S, Leclercq P et al (2006) 18F-FDG PET imaging of rheumatoid knee synovitis correlates with dynamic magnetic resonance and sonographic assessments as well as with the serum level of metalloproteinase-3. Eur J Nucl Med Mol Imaging 33:275–280
Angelides S, El-Mashaleh M, Anagnostou M, Howe G, Spencer D, Kumar V et al (2014) The role of 99mTc-labelled glucosamine (99mTc-ECDG) in the evaluation of rheumatic joint disease: a screening experience. Nucl Med Commun 35:655–665
Yang DJ, Kim CG, Schechter NR, Azhdarinia A, Yu DF, Oh CS et al (2003) Imaging with 99mTc ECDG targeted at the multifunctional glucose transport system: feasibility study with rodents. Radiology 226:465–473
Szkudlarek M, Court-Payen M, Strandberg C, Klarlund M, Klausen T, Ostergaard M et al (2001) Power Doppler ultrasonography for assessment of synovitis in the metacarpophalangeal joints of patients with rheumatoid arthritis: a comparison with dynamic magnetic resonance imaging. Arthritis Rheum 44:2018–2023
Roimicher L, Lopes FPPL, de Souza SAL, Mendes LF, Domingues RC, Da Fonseca LMB et al (2011) 99mTc-anti-TNF-α scintigraphy in RA: a comparison pilot study with MRI and clinical examination. Rheumatology 50:2044–2050
Duer A, Østergaard M, Hørslev-Petersen K, Vallo J (2008) Magnetic resonance imaging and bone scintigraphy in the differential diagnosis of unclassified arthritis. Ann Rheum Dis 67:48–51
Kim JY, Choi YY, Kim CW, Sung YK, Yoo DH (2016) Bone scintigraphy in the diagnosis of rheumatoid arthritis: is there additional value of bone scintigraphy with blood pool phase over conventional bone scintigraphy? J Korean Med Sci 31:502–509
Höpfner S, Krolak C, Treitl M, Becker-Gaab C, Kellner H, Tiling R (2007) Imaging in the early diagnosis of changes in the hand of patients suffering from rheumatoid arthritis. Is ultrasound a true alternative for low-field magnetic resonance scanning, 3-phase bone scintigraphy and conventional x-rays?] [Article in German]. Z Rheumatol 66:56–62
Alexandre DJA, Carmo CCM, Romeiro LD, Gutfilen-singer G, Amarante JLM, De Souza SAL et al (2021) 99mTc-antitumor necrosis factor-alpha scintigraphy for the detection of inflammatory activity in rheumatoid arthritis. Nucl Med Commun 42:389–395
Rinkin C, Fosse P, Malaise O, Chapelier N, Horrion J, Seidel L et al (2021) Dissociation between 2-[18F]fluoro-2-deoxy-D-glucose positron emission computed tomography, ultrasound and clinical assessments in patients with non-severe rheumatoid arthritis, including remission. BMC Rheumatol 5:31
de Groot M, Patel N, Manavaki R, Janiczek RL, Bergstrom M, Ostor A et al (2019) Quantifying disease activity in rheumatoid arthritis with the TSPO PET ligand 18F-GE-180 and comparison with 18F-FDG and DCE-MRI. Eur J Nucl Med Mol Imaging Res 9:113
Acknowledgements
The authors acknowledge all the radiographers, nurses and staff of the Department of Nuclear Medicine and staff of the Division of Rheumatology, Department of Internal Medicine, Universitas Academic Hospital. The authors also acknowledge Goorhoo Pryaska for preparation of the radiopharmaceutical, and Dr. Daleen Struwig, medical writer, for technical and editorial preparation of the article.
Funding
Funds were received from the Multi-, Inter- and Trans- (MIT) Disciplinary Collaborative Research Grant under the University of the Free State (UFS) and Central University of Technology Free State (CUT) research collaboration project, and the South African National Research Foundation (NRF) (Grant Number 129902).
Author information
Authors and Affiliations
Contributions
OE was the major contributor in writing the article and the collecting data, JH and CD were contributors in writing and proofreading the article, GA and ML proof read the article and were involved with the study design, BJV played a big role in data collection, and JS analyzed and interpreted all the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the University of the Free State Health Sciences Research Ethics Committee (HSREC), with reference number UFS-HSD2020/1292/2411. Informed consent was taken from each participant, signing an informed consent form in the process.
Consent for publication
This was gotten from each participant when the signed the informed consent form.
Competing interests
The authors declare that there is no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Evbuomwan, O., Engelbrecht, G., Driver, C. et al. Head-to-head comparison of ultrasound and 99mTc-glucosamine SPECT/CT imaging of patients with rheumatoid arthritis: a single center prospective study. Egypt J Radiol Nucl Med 54, 223 (2023). https://doi.org/10.1186/s43055-023-01168-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01168-w