Abstract
Background
Endometriosis is a chronic gynecological condition affecting women of reproductive age and may cause pelvic pain and infertility. MRI is the best imaging technique for mapping and preoperative staging of endometriosis as it provides a tool for the assessment of deep infiltrating endometriosis. The aim of this study was to evaluate the role of magnetic resonance imaging (MRI) in detection and characterization of endometriosis in correlation between it and the laparoscopic findings according to ENZIAN classification.
Methods
We assessed 100 patients by MRI dedicated pelvis protocol for endometriosis with an assessment of the ovaries, uterus, uterosacral ligaments (USL), broad ligaments, and round ligaments, cul-de-sac, rectosigmoid colon, bladder, ureters, and rectovaginal septum. All these patients are submitted for laparoscopy, and then, data from both investigations were correlated.
Results
MRI provided a road map for surgeons before laparoscopy. The sensitivity of MRI was 87.5% in small deep infiltrating endometriosis (DIE) (grade A1) and 100% in large DIE (A2). MRI detected 82.3% of uterosacral ligament involvement, specificity 80%. Detection rate in rectal involvement was 71.4%, specificity 75%. There was 100% sensitivity and specificity in adenomyosis and urinary bladder endometriosis.
Conclusions
Preoperative detection of endometriotic lesions is recommended using a dedicated MRI endometriosis protocol to choose the surgical approach and for proper multidisciplinary teamwork planning.
Similar content being viewed by others
Background
Endometriosis is defined as presence of ectopic endometrial glands and stroma outside the normal uterine tissue. It is an estrogen-based condition, and it is a common cause of pelvic pain, dyspareunia, dysmenorrhea, infertility and sometimes can be asymptomatic, affecting approximately 10% of premenopausal women. Symptoms usually depend on the site and the depth of the infiltration and whether the endometriosis is complicated by adhesions [1].
The main and typical localizations of endometriosis are: ovarian endometrioma, retrocervical endometriosis, deep bowel endometriosis, urinary bladder endometriosis and abdominal wall endometriosis [2].
Radiologists should be familiar with the various imaging manifestations of that disease as preoperative mapping of disease extension is important to decide whether surgical intervention is indicated, and if so, for proper preoperative planning.
Magnetic resonance (MR) imaging has been recently widely used for the detection and characterization of pelvic endometriosis and has established its effectiveness [2].
It must be remembered that benign endometriomas, like many pelvic malignancies, may exhibit restricted diffusion. Although women with endometriosis are at risk for developing clear cell and endometrioid epithelial ovarian cancers (i.e. endometriosis-associated ovarian cancers), imaging findings such as enhancing mural nodules should be confirmed before the diagnosis of ovarian malignancy is offered. The presence of dilated fallopian tube, especially hematosalpinx, is often associated with pelvic endometriosis [3].
In superficial endometriosis—also known as Sampson's syndrome—superficial plaques are scattered across the peritoneum, ovaries, and uterine ligaments.
Deep infiltrating endometriosis—also known as Cullen’s syndrome—can involve the pelvic ligaments, anterior rectosigmoid colon, bladder, uterus, and cul-de-sac, as well as surgical scars; the lesions often have poorly defined margins and T2 signal hypo-intensity as a result of fibrosis. The presence of sub-centimetric foci with T2 hyperintensity representing ectopic endometrial glands within these infiltrating fibrotic masses may help establish the diagnosis [4].
T1-weighted fat-suppressed pulse sequences are recommended for all MR examinations of the female pelvis because such sequence facilitates the detection of small endometriomas and aids in their differentiation from mature cystic teratomas [4].
Our work aimed to evaluate the role of magnetic resonance imaging (MRI) in detection and characterization of endometriosis in correlation between it and the laparoscopic findings according to ENZIAN classification.
Methods
The study was conducted during the period from July 2020 till July 2022. Out of 200 scanned patients, only 100 patients were selected in this retrospective single-institution study, and the included patients underwent dynamic ultrasound followed by MRI endometriosis protocol then laparoscopy.
Inclusion criteria were patient in child bearing period with clinical diagnosis of endometriosis who could do the MRI (not claustrophobic, not pregnant, and has no renal impairment), and patients who did laparoscopic correlation.
Exclusion criteria included patients who did not perform laparoscopy or failed to complete MRI study, due to renal function impairment or claustrophobia or MRI incompatible prosthesis implementation.
The study was approved by the Institutional Ethics Committee, approval number 23–2020. No consent was obtained from patients due to the nature of the study.
Patient aged 27 to 42 years, MRI was performed anytime during the month after 4–6 h fasting, and enema was administered 2–3 h before the examination. Urinary bladder was moderately-filled; the examination finished in 35 to 40 min with no complication.
MRI acquisition
A dedicated MRI protocol was applied using 1.5 Tesla superconducting unit (Signa LX, GE Healthcare) and high-resolution phased array coils.
The protocol sequences and parameters included: T1WI in axial and sagittal planes, T2WI in axial, sagittal and coronal plane FOV 38, 32, and 32 mm, respectively, axial T2 with fat suppression, coronal T2WI of the abdomen including the kidneys interslice gap 0.5 mm, section thickness 5 mm, axial DWI 5 mm slice thickness and interslice gap 1 mm, b-value 1000, fat-suppressed T1-weighted 3D gradient-echo LAVA sequence in three planes 3.4 mm slice thickness. Intravenous (IV) gadopentetate contrast (70–80 ml) was administrated followed by repetition of the LAVA in three planes.
MRI interpretation
The images were interpreted by a radiologist who has 3-year experience in endometriosis cases. ENZIAN classification which provides a complete assessment of endometriosis was used (Fig. 1). [5, 6].
ENZIAN classification for deep endometriosis is based on pelvic three compartments classification (A—vagina, rectovaginal space (RVS); B—uterosacral ligaments (USL)/cardinal ligaments/pelvic sidewall; and C—rectum) as well as the urinary bladder (FB), the ureters (FU), and other extragenital lesions (FO).
The extent (size) of endometriosis is represented by the numbers 1, 2, and 3 in compartments P, O, T, A, B, and C.
The individual anatomical regions are defined by capital letters, and the size of the foci is divided into categories [7, 8].
Assessment included:
-
1.
Pelvic endometriotic nodules DIE was mentioned (A) with location and size description.
-
2.
Uterosacral ligaments on both sides (B0 and B1) were measured, and any thickening was reported.
-
3.
Rectosigmoid involvement (C) was mentioned with detailed localization in relation to the anal verge, and size was mentioned.
-
4.
The presence of adenomyosis (FA) was reported as present or absent.
-
5.
The presence of urinary bladder wall thickening (FU) was reported and the size measurement.
Laparoscopic interpretation
Patients underwent laparoscopic surgery by the same surgical team within a period not exceeding two months from the MRI examination, and otherwise, MRI was repeated.
ENZIAN classification was done based on laparoscopic findings.
MRI and laparoscopic correlation (Table 1)
Data of MRI ENZIAN classification including A, B, and C were reported and compared to the corresponding laparoscopic ENZIAN classification.
Statistical analysis
Statistical evaluation was performed using the SPSS (version 20.0; SPSS Inc., Chicago, IL, USA) software. Fisher’s exact or chi-square test was performed for categorical data, and the Kruskal–Wallis test was performed for continuous variables.
Surgical results were accepted as standard, and preoperative MRI findings were compared.
Sensitivity and specificity scores were calculated.
Results
Regarding ENZIAN classification in MRI, A0 was reported in 1 patient (1%), A1 was reported in 70 patients (70%) (Fig. 2), and A2 was reported in 2 patients (2%). B0 was reported in 30 patients (30%), and B1 was reported in 70 patients (70%) (Figs. 2, 3 and 4). C0 was reported in 50 patients (50%), and C1 was reported in 50 patients (50%) (Figs. 3 and 4). FA was reported in 90 patients (90%), and FU was reported in 20 patients (20%).
MRI sagittal T2WI A showing focal adenomyosis (long arrow), focal DIE at the back of the uterus (arrow head). Axial T2WI B shows thickening of the right uterosacral ligament (long arrow). Laparoscopic image C shows thickened uterosacral ligament (long arrow) and the DIE (short arrow). ENZIAN classification by MRI was A1 B1 B0 C0 FA and by laparoscopy A1 B1 B0 C1 FA
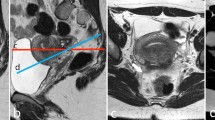
MRI axial T2WI A shows thickening of the right uterosacral ligament (long arrow). Axial T2WI B shows focal DIE on the serosal surface of the rectum (long arrow). Laparoscopic image C shows thickened uterosacral ligament (long arrow). ENZIAN classification by MRI was A1 B1 B0 C1 and by laparoscopy A1 B1 B0 C1
MRI sagittal T2WI A shows focal nodule of DIE at the back of the cervix (long arrow); note the diffuse thickening of the transitional zone consistent with adenomyosis. Axial T2WI B shows thickening of the both uterosacral ligaments (long arrows). Laparoscopic image C shows thickened of the uterosacral ligaments (long arrows). ENZIAN classification by MRI was A1 B1 B1 C1 FA and by laparoscopy A1 B1 B1 C1 FA
Regarding ENZIAN classification in laparoscopy, A0 was reported in none (0%), A1 was reported in 80 patients (80%) and A2 was reported in 2 patients (2%). B0 was reported in 15 patients (15%), and B1 was reported in 85 patients (85%). C0 was reported in 30 patients (30%), and C1 was reported in 70 patients (70%). FA was reported in 80 patients (80%), and FU was reported in 20 patients (20%) (Table 2).
Regarding detection of DIE, the sensitivity of MRI was 87.5% in small DIE (grade A1) while the detection rate was 100% in large DIE (A2). MRI detected 82.3% of uterosacral ligament involvement, specificity 80%. Detection rate in rectal involvement was 71.4%, specificity 75%. There was 100% sensitivity and specificity in adenomyosis and urinary bladder endometriosis.
Regarding pelvic compartments, MRI showed same rate of detection like laparoscopy in cases of DIE of the anterior compartment with sensitivity of 100%. For the middle compartment, MRI showed sensitivity of 90% in detecting DIE in correlation with laparoscopy. Regarding the posterior compartment, MRI showed sensitivity of 68.3% compared to laparoscopy.
Finally, regarding the size of DIE, MRI detection rate compared to laparoscopy was higher in bigger lesions; the sensitivity of MRI in detecting A1 lesions was 87.5%, while MRI sensitivity in detecting A2 lesions was 100%.
Discussion
Endometriosis is a chronic multifocal gynecologic disease that commonly affects females of reproductive age and may cause pelvic pain and infertility. The etiology of endometriosis is unknown [9]. The disease is characterized by the growth of functional ectopic endometrial glands outside the uterus.
In this study, MRI and laparoscopic scores showed significant concordance regarding compartments A, B, O, and C, which was compatible as well with previous studies using ENZIAN classification.
Regarding ENZIAN classification in MRI, our results demonstrated 73% sensitivity and specificity of MRI in evaluation of compartment A, while a study done by Burla et al. [10] demonstrated 100% MRI sensitivity and specificity in compartment A lesions.
Regarding detection of DIE, the sensitivity of MRI was 87.5% in small DIE (grade A1), while the detection rate was 100% in large DIE (A2), in comparison with a study done by Bazot et al. [11] and found that diagnostic values of MRI for DIE are quite high: sensitivity, 90%; specificity, 91%; positive predictive value (PPV), 92%; negative predictive value (NPV), 89%; and accuracy, 90%, while pelvic MRI has a reported sensitivity of 90.3% for the detection of DIE in a study performed by Siegelman et al. [1].
Hottat et al. reported MRI sensitivity of 96.3% and NPV of 93.3% in endometriosis and DIE detection [12].
Medeiros et al. [13] recently published one meta-analysis on the diagnostic efficiency of pelvic MRIs in the diagnosis of deep endometriosis. Such meta-analysis reviews 20 studies published comparing the findings from high field MRIs (1.0–3.0T) to surgical findings (laparoscopic or open) and histology as a reference pattern. MRI studies showed 83 percent sensitivity and 90 percent specificity in the diagnosis of injuries due to endometriosis. The location that showed the highest sensitivity was the pouch of Douglas (sensitivity = 89 percent, specificity = 94 percent), while in the anterior compartment, the MRI sensitivity was lower (bladder sensitivity = 64 percent, specificity = 98 percent). This may be due to the fact that since the posterior compartment is the most common location of deep endometriosis, the MRI is more precise tool for its detection.
Sensitivity and negative predictive values of MRI confirmed by surgery were 95.2% and 91.7% (lesions in the vaginal/rectovaginal space), 78.4% and 56% (uterosacral ligaments), 91.4% and 89.7% (rectum/sigmoid colon), 57.1% and 94.1% (myometrium), 85.7% and 98.3% (bladder) in a study performed by Laurin et al. [14], while in our study, the sensitivity of MRI was 87.5% in small DIE (grade A1), while the detection rate was 100% in large DIE (A2). MRI detected 82.3% of uterosacral ligament involvement, specificity 80%. Detection rate in rectal involvement was 71.4%, specificity 75%. There was 100% sensitivity and specificity in adenomyosis and urinary bladder endometriosis.
Di Paola et al. [15] compared preoperative MRI findings with intraoperative laparoscopic results by means of the ENZIAN score and found an overall correlation of 95%, with a sensitivity of 94%. In this study, the values are almost similar values specially in compartment A with the highest value of the preoperative MRI-based ENZIAN score could be confirmed.
Aysun et al. [16] found that MRI has higher sensitivity and specificity in showing the lesions of the compartments O (ovarian lesions), A (rectovaginal septum and posterior vaginal fornix), and B (uterosacral ligaments and parametrium) (100–100%, 100–100%, and 97–100%, respectively, p < 0.001) compared to the other compartments. The lowest sensitivity, specificity, accuracy, and PPV of the MRI were found in compartment P (14%, 76%, 70%, and 7%, respectively).
Our study agreed with Keckstein et al., [17] that the correlation between preoperative imaging and surgical staging using ENZIAN classification allows for a consistent and clear classification of endometriosis.
In this study, the diagnosis of endometriosis was based on the laparoscopic findings, and then the histopathologic results as a second-line confirmation.
Limitations of this study are its retrospective study approach with a limited patients number as well as limitations of patients compliance to MRI and single institute study and also having single radiologist for image reading lacks inter-reader interpretation.
Further prospective studies in a multicentric setting with consistent diagnostic protocols will be required.
Advances in noninvasive multiparametric imaging modalities are of special importance as diagnostic standard value of endometriosis with systematic diagnostic approach for better preoperative planning that will lead to a reduction of recurrent or non-indicated interventions.
Conclusions
MRI highly correlates with the ENZIAN score and has 95% accuracy in the detection and localization of endometriosis, with specially 100% detection accuracy in the anterior compartment in concordance with laparoscopic findings.
In conclusion, MRI is a valuable diagnostic tool for endometriosis, enabling a better pre-laparoscopic planning, allowing to for proper preoperative detection and better laparoscopic and clinical outcome.
The ENZIAN score detected by MRI is well correlated with the laparoscopic findings.
The ENZIAN score may be used as an anatomical mapping and valuable communication language between the radiologists and the referring gynecologists.
Availability of data and materials
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request.
Change history
14 November 2023
A Correction to this paper has been published: https://doi.org/10.1186/s43055-023-01139-1
Abbreviations
- MRI:
-
Magnetic resonance imaging
- DWI:
-
Diffusion-weighted imaging
- DIE:
-
Deep infiltrating endometriosis
References
Siegelman ES, Oliver ER (2012) MR imaging of endometriosis: ten imaging pearls. Radiographics 32(6):1675–1691
Giudice LC, Kao LC (2004) Endometriosis. Lancet 364(9447):1789–1799
Nnoaham KE, Hummelshoj L, Webster P, d’Hooghe T, de Cicco NF, de Cicco NC (2011) Impact of endome- triosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril 96(2):366–373
Chamié LP, Blasbalg R, Gonçalves MO, Carvalho FM, Abrão MS, de Oliveira IS (2009) Accuracy of magnetic resonance imaging for diagnosis and preoperative assessment of deeply infiltrating endometriosis. Int J Gynaecol Obstet 106(3):198–201
Keckstein J, Ulrich U, Possover M, Schweppe KW (2003) ENZIAN-Klassifikation der tief infiltrierenden Endometriose. Zentralbl Gynäkol 125:291
Tuttlies F, Keckstein J, Ulrich U, Possover M, Schweppe KW, Wustlich M et al (2005) ENZIAN-score, a classification of deep infiltrating endometriosis. Zentralbl Gynakol 127(5):275–281
Classification of endometriosis (1997) The American Fertility Society. Fertil Steril 32(6):633–634
Metzemaekers J, Haazebroek P, Smeets MJGH, English J, Blikkendaal MD, Twijnstra ARH, Adamson GD, Keckstein J, Jansen FW (2020) EQUSUM: Endometriosis QUality and grading instrument for SUrgical performance: proof of concept study for automatic digital registration and classification scoring for r-ASRM, EFI and Enzian. Hum Reprod Open 2020(4):hoaa053
Bazot M, Bharwani N, Huchon C et al (2017) European society of urogenital radiology (ESUR) guidelines: MR imaging of pelvic endometriosis. Eur Radiol 27(7):2765–2775. https://doi.org/10.1007/s00330-016-4673
Burla L, Scheiner D, Hötker AM, Meier A, Fink D, Boss A, Imesch P (2021) Structured manual for MRI assessment of deep infiltrating endometriosis using the ENZIAN classification. Arch Gynecol Obstet 303(3):751–757
Bazot M, Darai E, Hourani R, Thomassin I, Cortez A, Uzan S et al (2004) Deep pelvic endometriosis: MR imaging for diagnosis and prediction of extension of disease. Radiology 232:379–389
Hottat N, Larrousse C, Anaf V, Noel JC, Matos C et al (2009) Endometriosis: contribution of 3.0-T pelvic MR imaging in preoperative assessment–initial results. Radiology 253:126–134
Medeiros LR, Rosa MI, Silva BR, Reis ME, Simon CS, Dondossola ER et al (2015) Accuracy of magnetic resonance in deeply infiltrating endometriosis: a systematic review and meta-analysis. Arch Gynecol Obstet 291:611–621
Burla L, Scheiner D, Seidel EPSS, Eberhard M, Fink D, Boss A, Imesch P (2019) The ENZIAN score as a preoperative MRI-based classification instrument for deep infiltrating endometriosis. Arch Gynecol Obstet 300(1):109–116
Di Paola V, Manfredi R, Castelli F, Negrelli R, Mehrabi S, Pozzi Mucelli R (2015) Detection and localization of deep endometrio- sis by means of MRI and correlation with the ENZIAN score. Eur J Radiol 84(4):568–574. https://doi.org/10.1016/j.ejrad.2014.12.017
Tunca AF, Iliman DE, Akdogan A, Kaya GC (2023) Predictive value of preoperative MRI using the #ENZIAN classification score in patients with deep infiltrating endometriosis. Arch Gynecol Obstet 307(1):215–220
Keckstein J, Saridogan E, Ulrich UA, Sillem M, Oppelt P, Schweppe KW, Krentel H, Janschek E, Exacoustos C, Malzoni M, Mueller M, Roman H, Condous G, Forman A, Jansen FW, Bokor A, Simedrea V, Hudelist G (2021) The Enzian classification: a comprehensive non-invasive and surgical description system for endometriosis. Acta Obstetr Gynecol Scand (AOGS) 100(7):1165–1175
Acknowledgements
This research was carried out at King’s College Hospital, Dubai, which is fully equipped by dedicated machines for proper breast imaging. We want to thank our colleagues who helped us to do such research work.
Funding
There are no funding sources.
Author information
Authors and Affiliations
Contributions
HA collected patient data from the dedicated cases and was responsible for correspondence to journal. ME performed the statistical analysis and participated in manuscript drafting, writing the manuscript, and its revision. The authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocol was reviewed and approved by the local ethical committee of “Research Ethics Committee at the Faculty of Medicine, Ain Shams University.” It ruled that no formal ethics approval was required in this retrospective study, and so no reference number was given by the IRB.
Consent for publication
This research is based on retrospective study, yet, written consent for publication was obtained for these cases.
Competing interests
There is no financial or non-financial competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The title of this article has been corrected
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elsadawy, M.E.I., Ali, H.I. MRI of Endometriosis: Single institute experience including MRI classification and Laparoscopic correlation with ENZIAN classification. Egypt J Radiol Nucl Med 54, 188 (2023). https://doi.org/10.1186/s43055-023-01130-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01130-w